The changes in temperature and humidity typical of the cold season are associated with an increase in respiratory viral infections. For respiratory infection control, consistent hygiene and a healthy lifestyle are recommended, in addition to vaccinations and antiviral medications. If COVID-19 is suspected, point-of-care testing and PCR diagnosis should be performed as soon as possible.
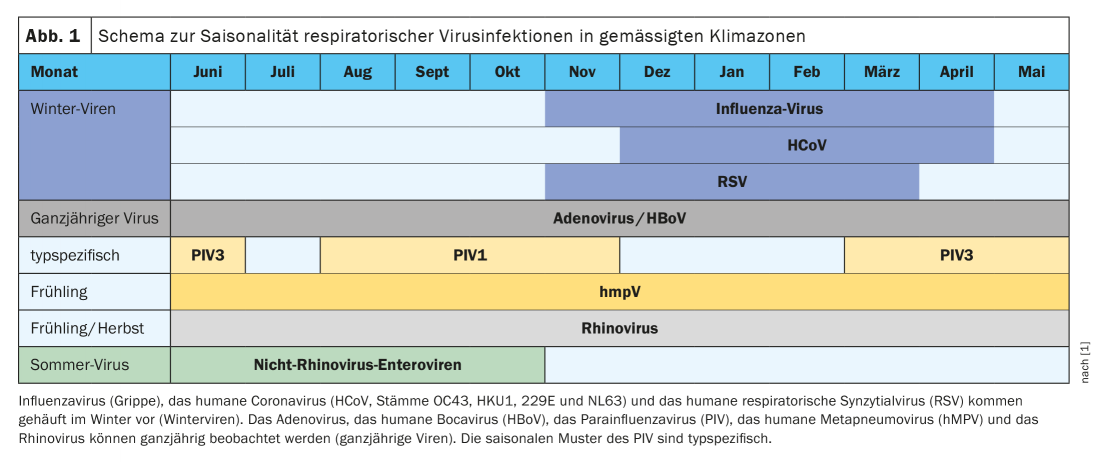
The fact that susceptibility to respiratory viral infections is increased in winter is due to several reasons. First, inhalation of cold air directly affects the mucous membranes of the upper respiratory tract, impairing mucociliary clearance and increasing mucus production. Second, cold and dry air weakens local innate antiviral immune responses [1]. A drop in absolute humidity is a major environmental factor that triggers a seasonal increase in influenza illness by resulting in low relative humidity in heated indoor environments [1,14]. Seasonal vitamin D deficiency also weakens direct pathogen clearance. In addition to the annual cold and flu waves in the cold season, the novel SARS-CoV-2 has also appeared in winter [1]. Influenza viruses, human coronaviruses, and the human respiratory syncytial viruses are also referred to as winter viruses (Fig. 1) . The year-round viruses include the adenoviruses, human bocavirus, human metapneumovirus (hMPV), and the rhinoviruses. In summary, seasonality of respiratory viruses is due to environmental parameters and human behavior.
Seasonal environmental factors: Temperature and humidity
The nasal and tracheal mucosa is affected by the temperature and moisture content of the ambient air during breathing. Several recent studies show that temperature and humidity can affect host innate antiviral immunity against respiratory viral infections [2–4]. The efficiency of transmission pathways is also affected by seasonal changes in outdoor climate and indoor climate. Temperature and humidity are thought to modulate the infectivity of viruses by affecting the properties of their surface proteins and lipid membrane [1,5,6]. It has been empirically demonstrated that low temperatures improve the arrangement of lipids on the virus membrane and contribute to the stability of the influenza virus [7]. Mucociliary clearance (MCC) is an important mechanism for the elimination of inhaled pathogens from the surface of respiratory epithelia, and the double layer of mucus with different viscosities is a prerequisite for efficient MCC [8]. Human experiments show that dry breath does not affect nasal MCC in young, healthy individuals. Overall, there are rather few human experimental findings, but in an older study in humans of different ages, it was found that a gradual reduction in the relative humidity of the breathing air from 70% to 20% was associated with a gradual reduction in MCC [1,9].
Colds caused by human rhinoviruses
Human rhinoviruses are major causes of colds during the winter months. Studies indicate that influences of cold winter air favor strong rhinovirus replication in the nasal mucosa [1]. A robust host antiviral immune response can block the spread of rhinovirus into the lower respiratory tract at core body temperature (37°C) by a strong IFN response. In contrast, the attenuated immune responses resulting from lower temperatures in the nasal cavity during the cold season allow efficient rhinovirus replication because of low production of type I IFN by epithelial cells. Keeping the nose warm can strengthen the innate antiviral defense against the cold virus and prevent colds.
Do not underestimate influenza viruses
Although influenza is often dismissed as a harmless flu-like illness, the influenza virus can also cause fatal symptoms and spread epidemically. This is illustrated by the examples of the Spanish flu (1918-1920), the Asian flu (1957/1958), and the Hong Kong flu (1968-1970). The new H5N1 virus that emerged in Hong Kong in 1997 was of avian origin and achieved a lethality of over 50% in humans. Fortunately, the spread of this virus and the SARS outbreak recorded in China in 2002/2003 was small. The global spread of the so-called swine flu influenza virus in 2009 led to approximately eight billion US dollars being spent worldwide on the antiviral drug Tamiflu [10]. However, the epidemic turned out to be more harmless than expected.
Regulation of the indoor climate as a preventive measure
In addition to vaccinations and antiviral medications, a healthy lifestyle (balanced diet, more than 7 hours of sleep) and consistent hygiene (hand washing, wearing face masks) can increase antimicrobial resistance and reduce the risk of transmission [1]. Regulation of the indoor environment can also help prevent respiratory infections. Interventions with humidifiers have produced good results in several studies. An empirical study in the U.S. demonstrated that air humidification in kindergartens from January to March to ~45% relative humidity resulted in a substantial reduction in total influenza virus and viral gene copies in the air and on objects compared with control kindergartens without air humidification [11]. However, it is important to use humidifiers in living spaces in a targeted manner and with the necessary care.
Literature:
- Moriyama M, et al: Seasonality of respiratory viral infections. Annu Rev Virol 2020; 7: 2.1-2.19.
- Kudo E, et al: Low ambient humidity impairs barrier function and innate resistance against influenza infection. PNAS 2019; 116: 10905-10910.
- Foxman EF, et al: Two interferon-independent double-stranded RNA-induced host defense strategies suppress the common cold virus at warm temperature. PNAS 2016; 113: 8496-8501.
- Moriyama M, Ichinohe T: High ambient temperature dampens adaptive immune responses to influenza A virus infection. PNAS 2019; 116: 3118-3125.
- Shaman J, Kohn M: Absolute humidity modulates influenza survival, transmission, and seasonality. PNAS 2009; 106: 3243-3248.
- Marr LC, et al: Mechanistic insights into the effect of humidity on airborne influenza virus survival, transmission and incidence. J R Soc Interface 2019; 16: 20180298.
- Polozov IV, et al: Nat Chem Biol 2008; 4: 248-255.
- Bustamante-Marin XM, Ostrowski LE: Cilia and mucociliary clearance. Cold Spring Harb Perspect Biol 2017; 9:a028241.
- Ewert G. On the mucus flow rate in the human nose. Acta. Otolaryngol Suppl 1965; 200: Suppl. 200
- Zylka-Menhorn V: Pandemic prophylaxis with Tamiflu®. A case of multi-system failure. German Medical Journal 2014; 111: A665
- Reiman JM, et al: Humidity as a non-pharmaceutical intervention for influenza A. PLoS One 2018; 13: e0204337.
- Hufert F, Spiegel M: Coronaviruses: from the common cold to severe lung failure. Monatsschr Kinderheilkd 2020: 1-11.
- Chinese Clinical Guidance for COVID-19 Pneumonia Diagnosis and Treatment (7th edition), http://kjfy.meetingchina.org/msite/news/show/cn/3337.html
- Shaman J, et al: PLoS Biol 2010; 8:e1000316.
HAUSARZT PRAXIS 2020; 15(10): 32-33