Based on data from large clinical trials, it is currently recommended that all patients with diabetes and chronic heart failure – regardless of left ventricular ejection fraction – are treated with an SGLT-2 inhibitor as an add-on. As a result, studies have shown a significant reduction in heart failure-related hospitalization and cardiovascular mortality. SGLT-i should be used as part of a multimodal therapy.
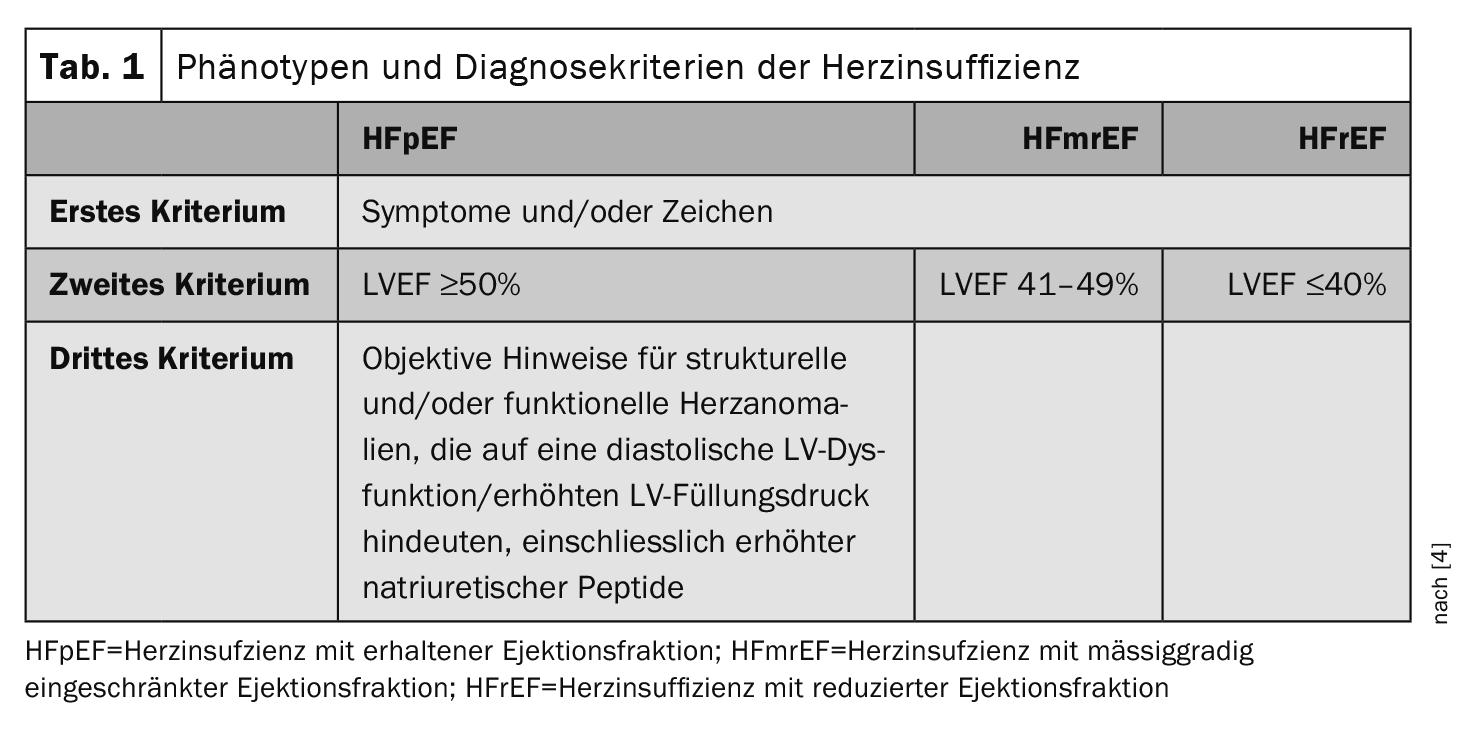
Around a third of all patients with diabetes have heart failure (Table 1). The risk of heart failure is 2-5 times higher in diabetics compared to the general population, explained Dr. Amadea Erben from the German Heart Center Munich [1]. “We need to screen diabetes patients regularly,” said the speaker, asking about symptoms such as reduced performance, dyspnea or leg edema. Conversely, patients with heart failure have an increased risk of developing diabetes. 30-40% of patients with heart failure have diabetes or prediabetes. Therefore, all patients who have been diagnosed with heart failure for the first time should be screened for the presence of diabetes. For patients over 45 years of age with negative results, the guidelines recommend repeating this screening every three years, reported Dr. Erben [1].
Empagliflozin and dapagliflozin useful for HFpEF, HFmrEF and HFrEF
Until recently, no mortality-improving therapy could be offered to HFpEF patients. For example, the recommendations in the 2021 ESC guideline for this subgroup of heart failure patients were limited to using diuretics and controlling comorbidities as well as possible. “This has changed in the meantime,” the speaker admitted [1]. Based on the results of the EMPA-PRESERVED study on empagliflozin and the DELIVER study on dapagliflozin, a class I recommendation for these SGLT-2 inhibitors (SGLT-2-i) in HFpEF was postulated in the 2023 update of the ESC guideline [8,9]. “Both studies showed that the addition of an SGLT-2-i significantly reduced cardiovascular death and heart failure-related hospitalization. With empagliflozin by 21% and with dapagliflozin by 18%,” said Dr. Erben from [1,8,9].
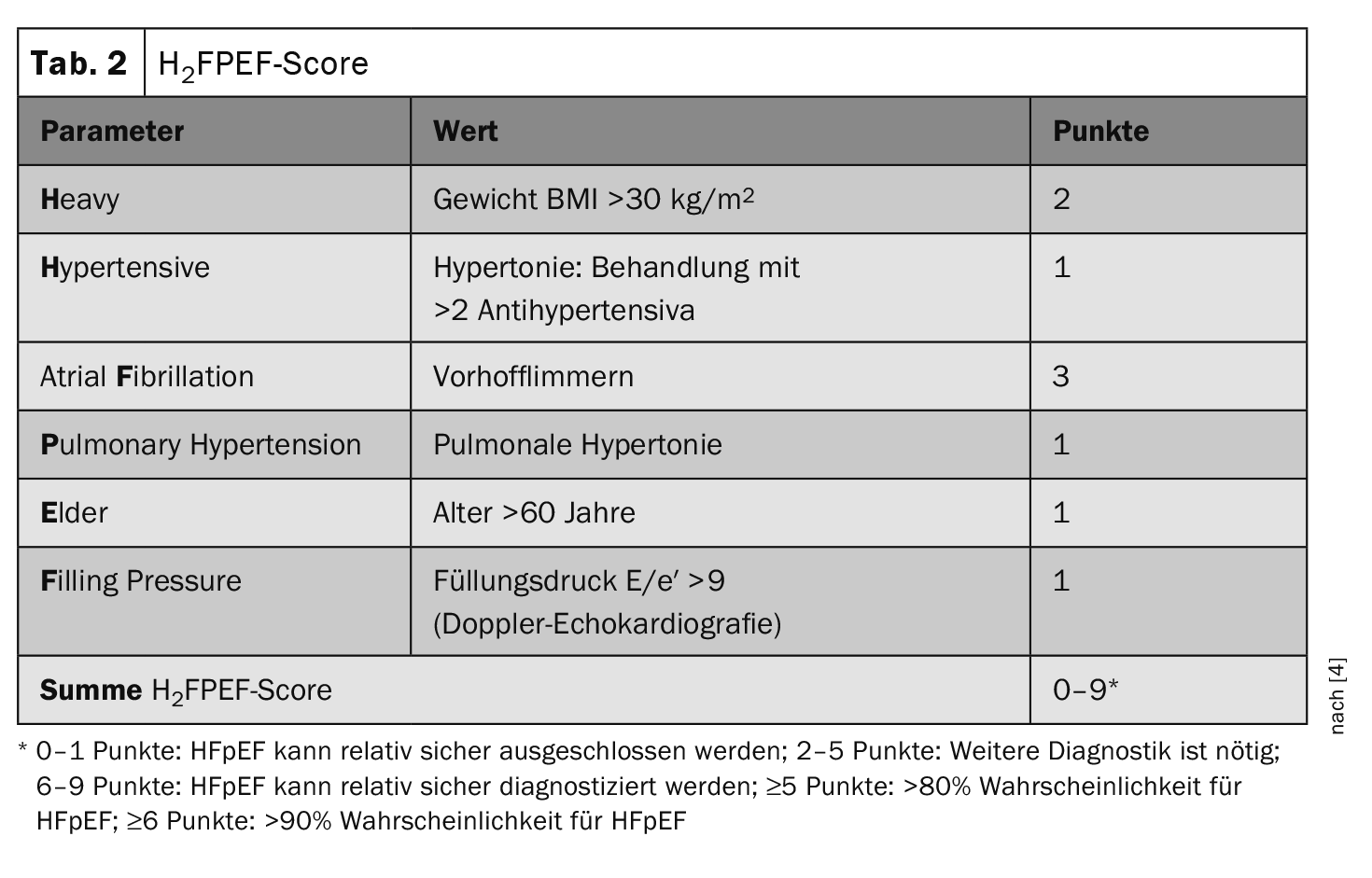
H2FPEFscore as a diagnostic aid
“Comorbidities play an important role in the development of HFpEF,” emphasized the speaker [1]. Comorbid concomitant symptoms such as arterial hypertension, obesity or iron deficiency are mapped in the H2FPEF score. This score recommended in the ESC guidelines (Table 2) was developed in 2018 and validated using retrospective data from people referred for invasive arterial blood pressure measurement due to unexplained dyspnea. Whether HFpEF is present is assessed in the H2FPEF score using 6 parameters from different areas (risk factors, previous illnesses and echocardiography) [2,3]. In the validation study, this score allowed patients with HFpEF to be well differentiated from those with non-cardiac causes of dyspnea (p<0.0001).
Which combination therapy is best for HFrEF?
For the treatment of HFrEF (LVEF ≤40%), a class I recommendation for the use of the “Fantastic four” has been in place since 2021: ACE inhibitor or ARNI, SGLT-2-i, beta blocker and mineralocorticoid receptor antagonist. In the two landmark studies DAPA-HF and EMPEROR-Reduced, SGLT-2-i as an add-on was shown to significantly reduce the combined endpoint of death and heart failure-related hospitalization [10,11]. Dr. Erben pointed out that these prognosis-improving effects proven in studies only apply to patients with type 2 diabetes, while there is no recommendation for the use of SGLT-2-i for type 1 diabetics [1]. It is also important to inform patients not only about the benefits of SGLT-2-i, but also about possible side effects. For example, it can lead to an increased urge to urinate and a reduction in blood pressure, and sufficient fluid intake has proven to be useful in preventing urogenital infections, the speaker reported [1]. You should also follow the “sick day rules” to prevent ketoacidosis. In concrete terms, this means that the SGLT-2-i should be paused if food and liquid intake is lacking and only resumed when eating habits normalize. This refers, for example, to phases of illness with fever, diarrhea and vomiting, but also to the time before or after major operations or stays in the intensive care unit [4].
With regard to implementation and titration of the “Fantastic four”, it is recommended to start all four substance classes promptly at low doses and to titrate them slowly depending on the underlying patient profile [4]. There are controversial opinions as to whether an ACE inhibitor or an ARNI should be given preference in the four-drug combination. The European guideline favors ACE-i; according to the American guideline, an ARNI should be used first. According to current knowledge, the “Fantastic four” is a lifelong therapy. This can be deduced from the TRED-HF study (“Therapy withdrawal in REcovered Dilated cardiomyopathy – Heart Failure”): a relapse occurred in each case following gradual discontinuation [5]. On the other hand, drugs such as saxagliptin or pioglitazone with potentially negative effects on heart failure should be discontinued. And, of course, regular checks are important, especially of the HbA1c values.
Holistic therapeutic approach including comorbidities
“The treatment of heart failure requires an interdisciplinary team,” emphasized Dr. Erben [1]. Comorbidities are prognostically unfavorable not only in HFpEF, but also in patients with HFrEF or HFmrEF and should be treated adequately. “The more comorbidities there are, the worse the patient’s prognosis and the more we are required to take these comorbidities into account,” summarized the speaker [1]. Iron deficiency is an important and frequent comorbidity in heart failure. Up to two thirds of patients are affected. If an iron deficiency is detected (transferrin saturation below 20% or serum ferritin below 100 ng/ml), treatment with intravenous iron should be given. The speaker pointed out that this recommendation applies even though no significant mortality benefit could be demonstrated in the IRONMAN study [6]. However, it has been shown that correcting iron deficiency can improve patients’ symptoms and quality of life. The results of the large randomized outcome study FAIR-HF2 are still pending [12]. Last but not least, non-drug treatment components such as patient education, physical training and nutrition are also important factors in the management of heart failure. If patients remain symptomatic, device therapy (e.g. ICD) should be considered.
Congress: Diabetologie grenzenlos
Literature:
- «Herzinsuffizienz», Dr. med. Amadea Erben, Diabetologie grenzenlos, München, 02.–03.02.2024.
- «In 3 einfachen Schritten zur HFpEF-Wahrscheinlichkeit», https://herzmedizin.de, (letzter Abruf 27.02.2024).
- Reddy YNV, et al.: A Simple, Evidence-Based Approach to Help Guide Diagnosis of Heart Failure With Preserved Ejection Fraction. Circulation 2018; 138(9): 861–870.
- Schütt K, et al.: Positionspapier Herzinsuffizienz und Diabetes, Kardiologie 2022; 16: 358–371.
- Halliday BP, et al.: Withdrawal of pharmacological treatment for heart failure in patients with recovered dilated cardiomyopathy (TRED-HF): an open-label, pilot, randomised trial. Lancet 2019; 393(10166): 61–73.
- Kalra PR, et al.: IRONMAN Study Group. Intravenous ferric derisomaltose in patients with heart failure and iron deficiency in the UK (IRONMAN): an investigator-initiated, prospective, randomised, open-label, blinded-endpoint trial. Lancet 2022; 400(10369): 2199–2209.
- Sun Y, et al.: Predictive value of H2FPEF score in patients with heart failure with preserved ejection fraction. ESC Heart Fail 2021; 8(2): 1244–1252.
- Anker SD, et al.: EMPEROR-Preserved Trial Investigators. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. NEJM 2021; 385(16): 1451–1461.
- Solomon SD, et al.: on behalf of the DELIVER Trial Committees and Investigators. Dapagliflozin in Heart Failure With Mildly Reduced or Preserved Ejection Fraction. NEJM 2022; 387: 1089–1098.
- McMurray JJV, et al.: DAPA-HF Trial Committees and Investigators. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. NEJM 2019; 381(21): 1995–2008.
- Packer M, et al.: EMPEROR-Reduced Trial Investigators. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. NEJM 2020; 383(15): 1413–1424.
- FAIR-HF2-DZHK5, https://fair-hf2.dzhk.de,(last accessed 28.02.2024).
HAUSARZT PRAXIS 2024; 19(3): 34-35 (published on 20.3.24, ahead of print)
CARDIOVASC 2024; 23(1): 32–33
InFo DIABETOLOGIE & ENDOKRINOLOGIE 2024; 1(2): 26