There are skin regions that are sometimes somewhat neglected in everyday practice. These include the oral mucosa and lesions of the anogenital region. Especially with the latter, patients present late due to shame.
PD Dr. Dr. med. Antonio Cozzio, Chief Physician, Clinic for Dermatology, Venereology and Allergology, Cantonal Hospital St. Gallen, first presented some (mucous) skin changes that are normally harmless. One example is the so-called lingua plicata (or scrotalis). This increased tongue furrowing is usually asymptomatic and considered a harmless normal finding. Sometimes, however, there is an association with other syndromes: If, in addition, a lip swelling is found that slowly increases over weeks and months and does not remit spontaneously, sometimes even assuming grotesque forms, this is referred to as cheilitis granulomatosa, which, together with lingua scrotalis and facial paresis, forms the Melkersson-Rosenthal syndrome. Lingua plicata may also be a component of acromegaly, Down syndrome, or Sjögren’s syndrome.
Another, usually also completely harmless disease of the tongue, is lingua geographica (synonym exfoliatio areata linguae, “wandering plaques”) with a daily changing appearance, which often affects children, adolescents and young adults. “Because the tongue is a part of the body that many people look at extraordinarily closely, carcinophobia can even occur when there are tongue changes,” the speaker noted. If the patient presents with other symptoms accordingly, migratory plaques should be considered as a differential diagnosis for lues II.
Lip changes
Chapped lips with scaling crusts and radial tears usually correspond to cheilitis simplex and are due to a drying effect (lip licking, in eczema or psoriasis), mechanical insults (lip chewing/chheilophagy), medications (e.g., in acne therapy with retinoids), or contact toxins (allergic or toxic). It should be noted in this context that pasta cerata, which is not infrequently used as a lip balm, also contains lanolin – an ingredient that is one of the most common contact allergens.
Cheilitis actinica, which can be divided into an acute and chronic form, must be distinguished from this. Acute light traumatization (the so-called “glacier burn” or “summer cheilitis”) or a phototoxic/allergic reaction can be the cause of cheilitis actinica acuta. Longer courses, on the other hand, involve chronic UV damage to the lower lip, which predominantly affects men in outdoor occupations and makes leukoplakia-like changes. This form should not be trivialized. A possible squamous cell carcinoma should be considered and a histological exclusion is necessary. Surgical treatment is usually used because breakthrough into the lymphatic vessels occurs more rapidly than with similar lesions in the skin. With a conservative approach, follow-up must be performed all the more carefully.
Cheilitis angularis (marginal lip eczema) is often localized and associated with sialorrhea, artificial dentition/disordered mouth closure (due to, for example, folds at the corners of the mouth, so-called “marionette folds”), but also with microbial and other factors such as malalimentation (iron deficiency, vitamin B deficiency). Here, a trial of zinc paste at night and disinfecting cream during the day will help, as well as the appropriate search for the cause. Differentially one should not forget – as so often – syphilis, which can be a systemic cause, especially in unilateral cheilitis angularis. “In any case, an ulcer of unclear genesis should always make us think of lues. Testing is indicated. TPPA is the most suitable screening test. If it is positive, an activity test should be reordered or performed directly by the laboratory,” Dr. Cozzio said.
Again, completely harmless and not requiring therapy are ectopic sebaceous glands, which can occur, for example, orally or genitally (synonym Fordyce’s condition). These are pinhead-sized white-yellowish nodules disseminated in the cheek fringe area or on the lips. Onset at puberty and regression at menopause are common.
Another leading symptom is oral ulceration. These must be analyzed bioptically if persistent. In erosive mucosal processes of the skin, conditions such as Behçet’s disease, chronic discoid lupus, the autoimmune bullous skin diseases pemphigus and pemphigoid, as well as lichen ruber and oral squamous cell carcinoma should also be considered and actively sought.
Adamantiades-Behçet’s disease and cutaneous lupus
Typically, Behçet’s disease presents with several of the following symptoms:
- Bipolar aphthosis (ulcerative aphthae of the oral cavity, aphthous ulcers of the genitals).
- Uveitis/Iridocyclitis (Hypopyon)
- Skin lesions, e.g. acneiform, folliculitis, pustules, erythema nodosum, thrombophlebitis, pathergy phenomenon
- Vascular changes such as vasculitis, phlebothrombosis
- Arthralgias
- Central nervous and gastrointestinal involvement.
In case of oral ulcers as well as scarring alopecia, chronic cutaneous lupus erythematosus (LE) should be considered, in which a very important therapeutic and preventive measure is consistent photoprotection. Topically, corticosteroids followed by calcineurin inhibitors may be considered in chronic discoid LE; systemically, hydroxychloroquine, methotrexate, and possibly mycophenolate mofetil are agents of choice. In smokers, the effect of hydroxychloroquine is greatly reduced, so smoking cessation should be aimed for.
Balanitis and perianal dermatitis
Initial treatment of trivial balanitis may initially include swing baths with Betadine® solution (light-light brown solution) once or twice daily and a topical antifungal cream (but not Imazol® cream because of rare risk of necrosis). A check-up in two to three weeks will show whether the therapy has taken effect. If not, at the latest then the differential diagnoses should be sought and possibly also a biopsy and further clarifications should be considered.
One of these differential diagnoses is balanitis circinata, which occurs in the setting of reactive arthritis (formerly Reiter’s disease). This disease is characterized by the postinfectious (dysenteric, urethritic) symptom triad:
- Arthritis
- Urethritis
- Conjunctivitis
Concomitant psoriasiform dermatoses are common. Young men are affected in over 90% of cases.
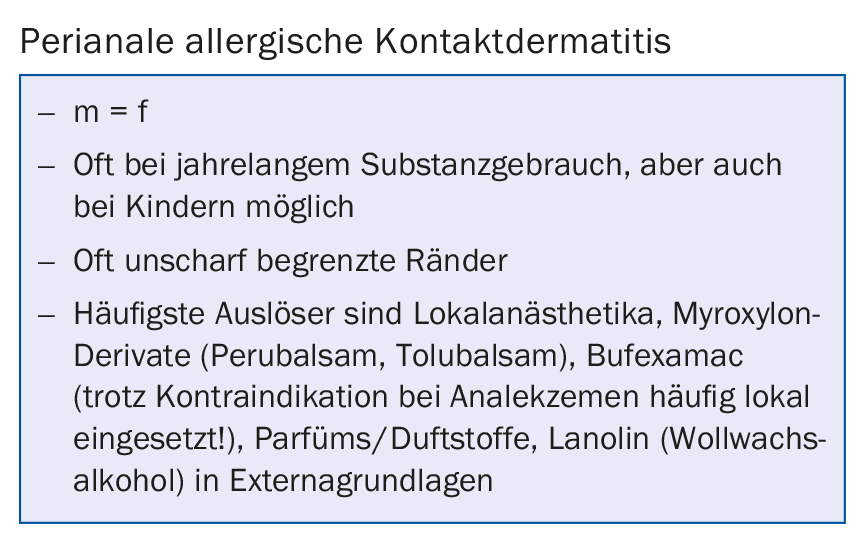
In the anal region, perianal dermatitis should primarily be thought of as perianal cumulative-toxic dermatitis, which is the most common cause of anal eczema, accounting for over 50%. Also very common is contact allergic eczema. Not infrequently, on the ground of chronic-irritative damage, contact allergy occurs in addition. Thus, 25-78% of patients with perianal dermatitis show a positive patch test. In addition, however, the causes of atopic or seborrheic dermatitis, which are also not uncommon, must also be taken into account.
The approach to perianal dermatitis, which is often relatively monomorphic erythematous and pruritic, is anamnesis-directed. With regard to cumulative-toxic damage, causes of fecal smearing and additionally a bacterial and mycological genesis (possibly oxyuria search) should be considered. An initial pragmatic therapy may consist of draining treatment with zinc paste, Eosin aqueous 0.5-2%, Solutio Castellani sine colore and possibly Imazol® cream paste. In case of resistance to therapy, further investigations such as proctological clarification, epicutaneous tests or a biopsy must be evaluated.
Source: Rheuma Top, August 24, 2017, Pfäffikon SZ
HAUSARZT PRAXIS 2017; 12(9): 38-40
DERMATOLOGIE PRAXIS 2017; 27(5): 37-38











