Biologic anti-T2 therapies can effectively reduce acute exacerbations and the need for daily doses of oral steroids in severe eosinophilic asthma. However, expiratory flow (FEV1) benefits little and shows only modest improvements despite the good efficacy of biologics. Researchers therefore asked the question: are there other factors that better address small airway dysfunction (SAD)?
The team of scientists from the LungenClinic Grosshansdorf (D) wanted to investigate whether SAD measurements in patients with severe eosinophilic asthma can better correlate or even be helpful to predict clinical response to biologic therapy and possibly describe a specific phenotype within this severe asthma population. For this purpose, they evaluated data from patients previously enrolled in the German prospective longitudinal All Age Asthma Cohort (ALLIANCE) [1]. ALLIANCE recruits asthma patients of all severities and inflammatory phenotypes. Ultimately, 20 adult patients were included who had severe eosinophilic asthma and were under treatment with anti-T2 biologic agents (mepolizumab, n=18; benralizumab, n=1; dupilumab, n=1).
All patients received inhaled corticosteroids (ICS; mean inhaled fluticasone equivalent 818 ± 403 µg) and long-acting β2-adrenoceptor agonists (LABA). 55% were treated with long-acting muscarinic receptor antagonists (LAMAs) and 80% received oral corticosteroids (OCS, mean daily prednisolone dose 6.4 ± 4.9 mg) before initiation of biologic therapies. The mean predicted FEV1 at baseline was 76 ± 21%.
Asthma control was assessed by impulse oscillometry (IOS) through an asthma control test (ACT) and the number of severe exacerbations. Small airway function was derived using frequency dependence of resistance (FDR) and mean expiratory flow from 25 to 75% of forced vital capacity (FEF25-75). Other parameters studied were residual volume (RV and RV/DC), blood eosinophils, and FeNO. Clinical response was defined as at least a 50% reduction in annual severe exacerbations and daily oral steroid doses accompanied by a 3-point increase in ACT score.
FDR and eosinophils with best predictive power
There were no significant differences in baseline values of all clinical variables between responders and partial/non-responders except for FDR%pred, which was significantly higher in responders. The area under the curve (AUC) for FDR%pred was better than for FeNO, blood eosinophils and FEV1 (Table 1). With a cut-off of 191%, a sensitivity of 75%, a specificity of 71% and an AUC of 79% (95% CI 59-99; p=0.035) were observed for FDR%. The best AUC was obtained when FDR%pred was combined with blood eosinophils. With cut-off values for FDR of 216%pred and blood eosinophils of 365/μl, the ROC curve showed a sensitivity of 75%, a specificity of 87%, and an AUC of 85% (95% CI 67-100; p=0.01) (Fig. 1).
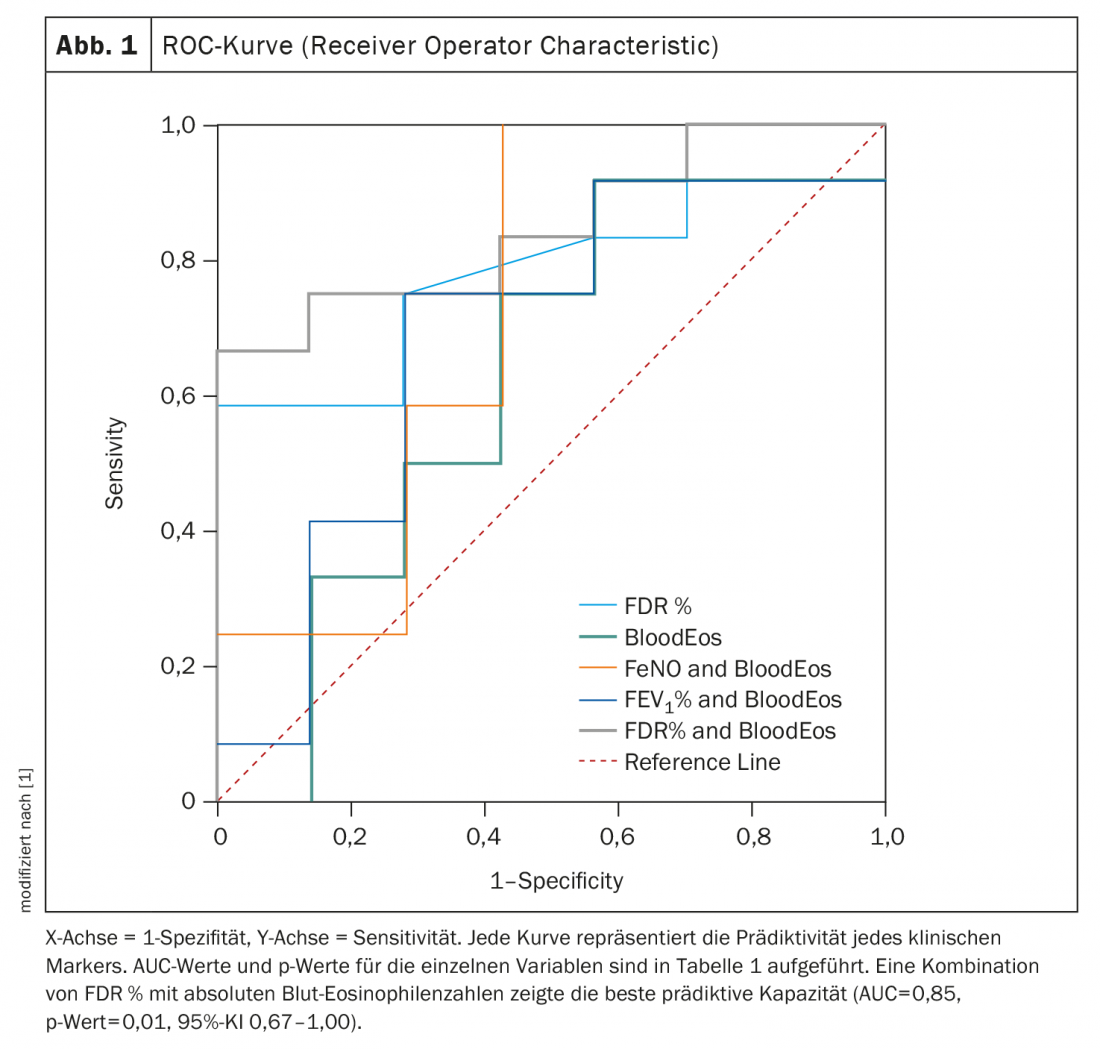
Within the response groups, responders to anti-T2 biologic therapies showed significant improvements in all clinical markers (FeNO, FEV1, FDR, blood eosinophils) versus partial or non-responders. The combination of FDR and blood eosinophils had the best predictive capacity for clinical response among all clinical markers tested. Compared respectively with FEV1 (R2=0.25, p=0.013), FDR score had better correlations with both ACT score (R2=0.42, p=0.001) and reduction of exacerbations (R2=0.41, p=0.001; FEV1:R2=0.20, p=0.025).
These data, the authors concluded, demonstrate that severe small airway dysfunction improves substantially with biologic anti-T2 therapy. In addition, pretreatment IOS measures of SAD were found to be meaningful predictors of clinical response, suggesting that severe SAD may describe a distinct phenotype with therapeutic implications in patients with severe eosinophilic asthma. According to them, oscillometric SAD measurements appear to be viable tools in the selection of appropriate patients qualifying for anti-T2 biologic therapy beyond the rather crude measurement of blood eosinophil count, which is often influenced by a variety of factors (e.g., dose of inhaled or oral steroids, diurnal variation, atopic comorbidities).
Literature:
- Abdo M, Watz H, Veith V, et al: Small airway dysfunction as predictor and marker for clinical response to biological therapy in severe eosinophilic asthma: a longitudinal observational study. Respir Res 2020; 21: 278; doi: 10.1186/s12931-020-01543-5.
GP PRACTICE 2021, 16(3): 32-34
InFo PNEUMOLOGY & ALLERGOLOGY 2021; 3(2): 22-23.












