Migraine sufferers are not among the easiest patients for doctors to care for. It is important for the physician to “educate” his patient to a prophylaxis that is appropriate for him, in order not to lose him completely at an early stage in the therapy. Various conventional migraine prophylactics are available to him for this purpose.
Although it is one of the basics in migraine treatment, it is still often neglected in patients’ everyday lives: keeping a headache diary. This is important in order to be able to understand in the long term how regularly and in what intensities the patient has to deal with attacks. It is no less important to set realistic therapy goals in advance of pain therapy. Patients must be given goals that they can actually meet – otherwise you quickly run the risk of losing them altogether. “If a chronic migraine patient develops the expectation of becoming completely pain-free, we will not be able to satisfy him,” explained Professor Martin Marziniak, M.D., chief physician of the Department of Neurology at the kbo-Isar-Amper-Klinikum München-Ost.
“However, if we tell him we’re aiming for a 50% reduction in pain, that’s first of all a contract we can get into.” Issues such as sleep quality should also be addressed early on. As the patient improves these, the routine alone also sets up better migraine prevention. This also applies to general everyday life: anyone who works until 2 p.m., comes home and has to look after the children straight away finds themselves in a situation in which they ultimately always have to function. “And then you get the effect that on the weekend, when the tension goes down, the migraines start.”
Start low, go slow
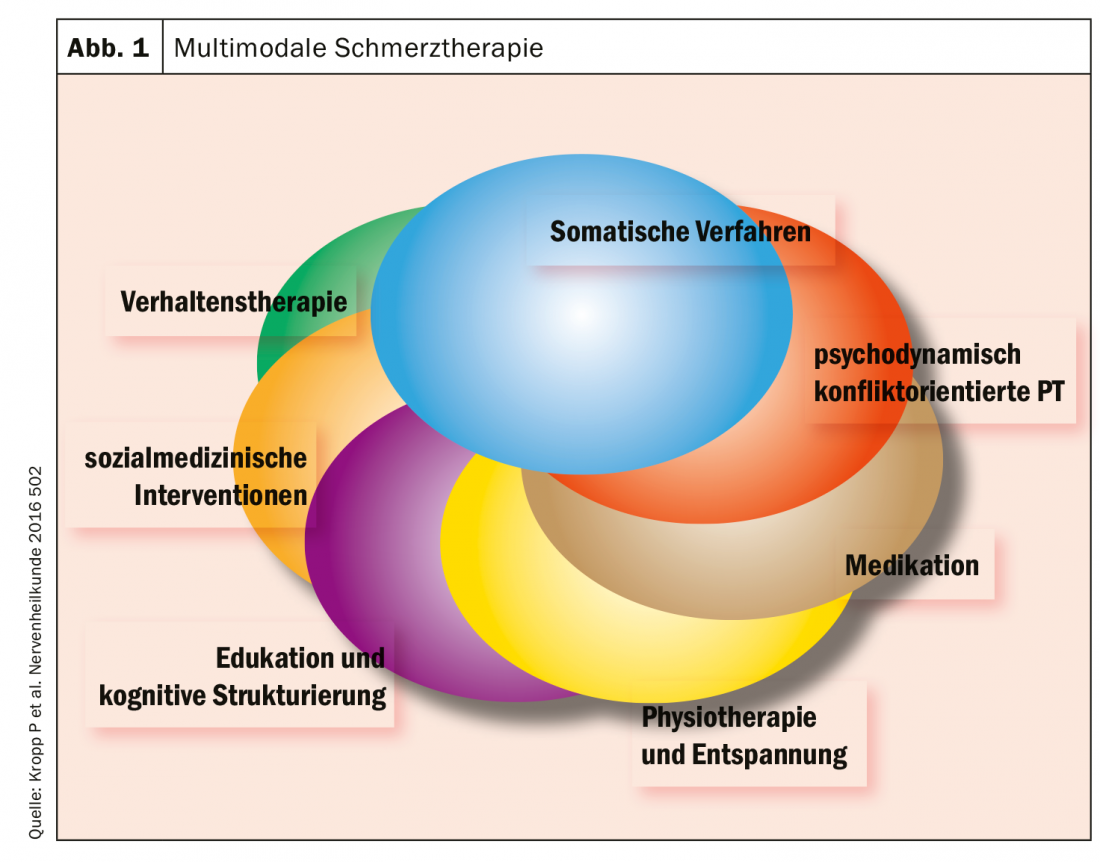
In drug prophylaxis, it is important to find individual dosages and titrations. The whole thing according to the motto Start low, go slow, Prof. Marziniak strongly advised a slow up-dosing in pain and headache patients, because otherwise there is a great risk of losing them again due to the side effects within the first 4-8 weeks. In doing so, the neurologist took up the cudgels for multimodal pain therapy: “When we talk about prophylaxis, it’s not about giving six different drugs, but about a coherent, coordinated overall package” (Fig. 1).
The list of modifiable risk factors for chronic daily headache is extensive, so factors such as smoking habits and caffeine intake should be recorded at the time of history taking. Prof. Marziniak pointed out that so-called life events, such as a move, the death of a loved one, or a stressful life situation, are not usually communicated by those affected themselves. Therefore, if a migraine seems to worsen for no apparent reason, the physician should ask specifically about it.
Drug and non-drug prophylaxis
Regarding the indication for drug prophylaxis, the colleague from Germany referred to the S1 guideline “Therapy of migraine attacks and prophylaxis of migraine” [1], which was revised in 2018 (Table 1). Non-drug prophylaxis includes first and foremost the avoidance of trigger factors. Prof. Marziniak also made it clear that this does not mean living in asceticism and doing without everything just because it could possibly trigger a migraine. “But if you know that you always get an attack after a glass of red wine, then of course you should already refrain from it in your own interest.” Other measures can include a regular sleep-wake rhythm and regular aerobic endurance sports. Behavioral therapy such as progressive muscle relaxation can also help. Good stress management is also part of migraine prophylaxis.
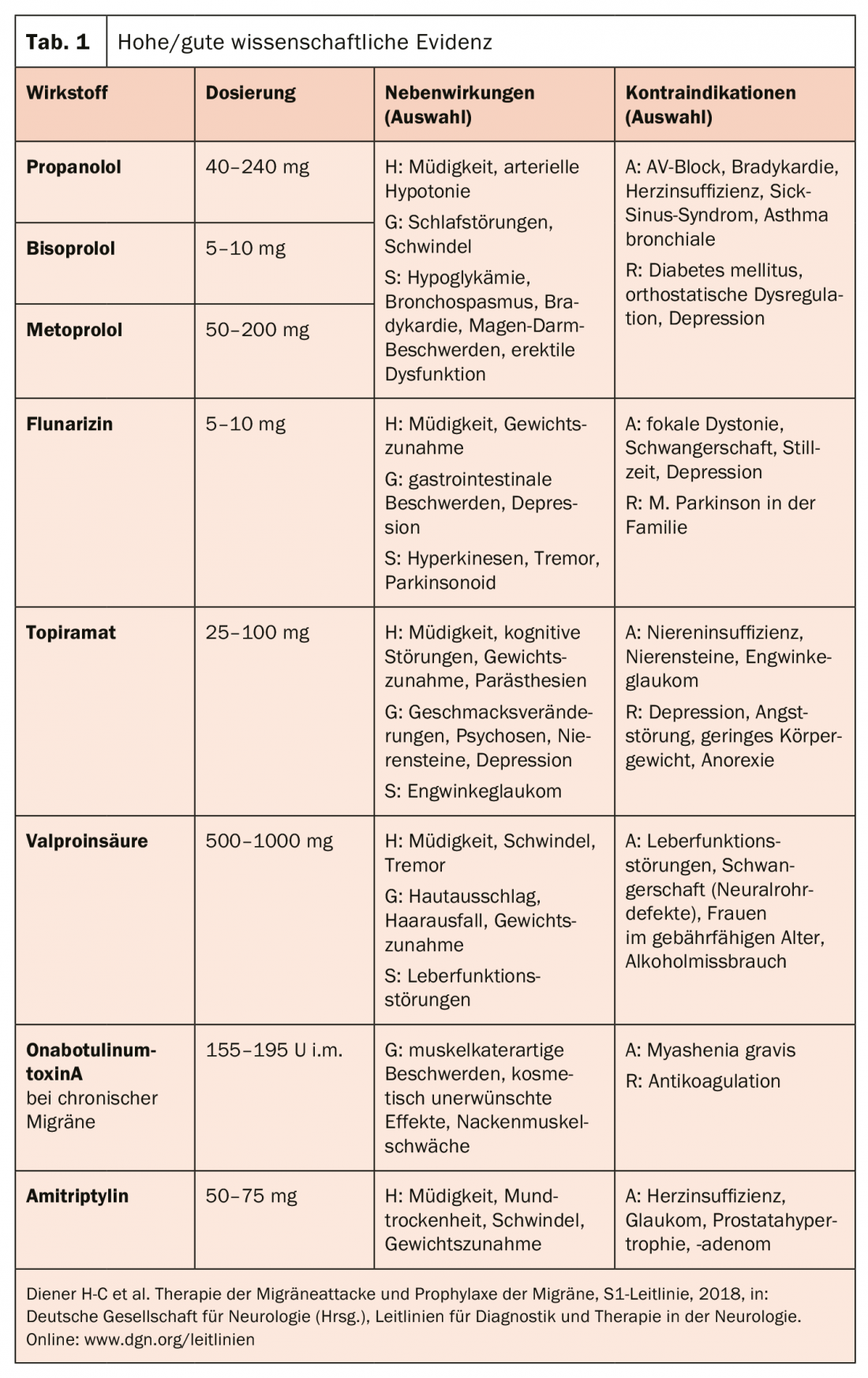
The good news, according to the expert, is that basically all migraine prophylaxis medications – whether angiotensin receptor blockers, anticonvulsants, beta blockers, serotonin agonists, SSRIs, or TCAs – are effective compared to placebo, provided they are used correctly. And proper use means increasing the dose correctly: “10 mg of amitriptyline tends to be too little, which ultimately leads to a lack of effectiveness.” Likewise, too short a duration of use (at least 3 months at the appropriate dose), discontinuation too early, failure to monitor adequately, and raising false expectations are counterproductive for prophylaxis. On the other hand, a lack of information about side effects in the run-up to treatment and a too rapid increase in dosage according to a rigid concept on the part of the physician on the one hand, and on the other hand disregard of the importance of comorbidities on the part of the patient and weight gain due to side effects too often lead to a premature discontinuation of the medication.
Source: Industry symposium “Migraine prophylaxis 2019: advantages and disadvantages of conventional and new therapies” at the German Pain Congress.
in Mannheim (D); Organizer: Lilly.
Literature:
- Diener HC, et al: Therapy of migraine attack and prophylaxis of migraine, S1 Guideline, 2018, in: German Society of Neurology (ed.), Guidelines for Diagnosis and Therapy in Neurology. Online: www.dgn.org/leitlinien
InFo PAIN & GERIATRY 2019; 1(1): 28-29 (published 11/22/19, ahead of print).










