The possible limitations caused by multiple sclerosis have an influence on the social framework of people with MS and their relatives. Changes in opportunities for participation in education, work, interaction in the social environment and within families influence quality of life and thus also have a direct impact on well-being. The tendency of stigmatization and relegation to “IV structures” not only hurts affected people, but also fails to recognize the enormous potential associated with active integration into social structures. Physicians, therapists and the Swiss MS Society can work together to help integrate and improve the quality of life for people with MS and their families. Important areas of action are: access to the best possible treatment, financial security, social and professional integration.
The diagnosis of MS confronts affected individuals and their families with a variety of challenges. Health issues, therapy options, chances and risks of therapy offers are always of essential importance for the affected person and his environment: How will it go on professionally? What will my and my family’s future look like if I am limited in my ability to work or even completely dependent on an IV pension? Can I or do I still want to participate in the social activities of my environment? Will I need walkers or even a wheelchair? How am I covered by health insurance? What services can or must I take advantage of? This all follows a diagnosis that many patients perceive as a shock. A change in social role, dropout from education or loss of work, change in standard of living, psychological well-being, change in social interaction, and family structures and circle of friends are indicators by which social impact can be measured [1].
Phase-dependent constraints and possibilities
At different stages, the social consequences of the diagnosis of MS vary individually according to the possibilities and limitations. For example, limitations in the ability to walk often lead not only to a restriction of the radius of activity without aids, but also to the stigmatization by the social environment, which is perceived very sensitively by those affected. Affected individuals face allegations and insinuations at work or at home and among friends, for example, due to the gait pattern with suspected alcohol use, the challenges of dealing with incontinence, or due to the effects of fatigue. These limitations correspond to numerous everyday, sometimes insurmountable hurdles that were not perceived before. Stairs – even without a wheelchair -, curbs or train platforms can be just as much of an obstacle for people with MS as tightly coordinated train connections, over-parked handicapped parking spaces or excessively high room temperatures. Even meeting friends in a restaurant can become impossible due to structural barriers. At the same time, uncertainties about the possible course of the disease and the resulting fears about the future create a psychologically stressful situation, both for those affected and their families. The direct social consequences such as job loss and loss of financial independence [1] are therefore the most frequent topics in the social counseling of the Swiss MS Society even after diagnosis. In 2013, more than 4,000 clients throughout Switzerland used the Swiss MS Society’s social counseling services, both in face-to-face or brief telephone consultations and for advice, support and representation in complex social insurance or case management settings.
The family system and the social environment are affected by the consequences of the disease. The changes in the family structure sometimes pose great challenges to those involved and often lead to conflicts that affect the closest social fabric. Professional support and care, including for the relatives, is therefore crucial in order to be able to meet the challenges to the social environment. In the extended social environment, affected individuals often find themselves forced to adapt their lifestyles. For example, participation in the activities of the sports club is no longer possible, although exercise, sporting activity and the associated social integration would have a positive influence on the health situation.
Problematic terminology
The individual situation of those affected must be given priority in the sense of effective support. Medical diagnosis and support are at the heart of all further measures, but it is often important to involve people with MS in the wide range of counseling and support services offered by the MS Society at an early stage. In addition to specialized MS social work care and representation, services include case management for job retention, caregiver and family support, events, continuing education, sports and exercise opportunities, children’s and youth camps, vacations and caregiver-led recreation for those with various support needs, and a nationwide social network of 50 regional groups. Close collaboration with the FPMS (specialist group for physiotherapy in MS) and a specifically qualified psychologist network makes appropriate therapeutic support available throughout Switzerland. In addition, the MS Society supports those affected by providing direct financial assistance.
Stigmatization of those affected after diagnosis by focusing on the terms and requirements of “disability insurance” leads to social disintegration, loneliness and ultimately also to a deterioration in the health development of those affected.
Already the term “disability insurance” shows the outdated and also wrong image of affected people: A systematic classification into the category “invalid” and its opposite (“valid”) is discriminatory. The fundamentally extremely positive fact that the federal government supports those people who are unable to fully support themselves financially due to health restrictions is counteracted by the fundamental stigmatization of “IV recipients”.
Therefore, a change both in the terminology and in the orientation of the working method in the sense of an “integration insurance” [2] makes sense.
The current public discussion creates unfair discrimination. “Social parasites” and “lazy people” – especially MS sufferers with different and changing symptoms are exposed to suspicions: That a person with MS can walk a few meters without a wheelchair one day and this is different the next,
is as difficult to convey as, for example, are the effects of fatigue. This is also an important task of the MS Society in particular: educating and informing the public.
Moreover, numerous attempts at reform and massive interference by courts with physicians’ authority [3] have not contributed to an improvement in the situation of people who are dependent on support. Affected persons who are confronted with considerable health and social limitations due to multiple sclerosis can remain integrated or be reintegrated into society according to their possibilities with the help of mainly medical expertise in cooperation with health professionals, social workers and the support of the services of the Swiss MS Society. The false basic assumption that sufficient social and financial pressure on patients would result in an improvement of the IV situation leads to the opposite: namely, only to a shift of costs to social assistance, which unnecessarily damages and humiliates affected persons. The negative health effects of this approach tend to result in higher rather than lower costs.
How can we promote the integration of people with MS?
The social counseling practice of the MS Society shows that efforts to integrate chronically ill fellow human beings must begin even before a so-called IV application. The individual situation of those affected and their relatives as well as the preservation of independence and a high quality of life, taking into account the different courses of MS (the “disease with a thousand faces”), require professional support in a complexly regulated social system. Especially in their professional environment, many affected people feel insecure. How should I deal with a diagnosis of MS in the workplace? Is early information to the employer necessary or will it result in dismissal? Those affected often reduce their workload because they hope to be able to meet professional requirements in this way. Such decisions can have existentially negative financial consequences for many affected persons in the long term if this reduction is not accompanied by a corresponding registration with the IV in the required cases.
The positive effects of professional social support on the health status of people with MS [4] – which then in turn also lead to a reduction in costs – are undisputed [5]. The integration of people with MS – in the sense of “integration insurance” – has a business benefit for companies, especially in times of a universally lamented shortage of skilled workers, who can productively deploy experienced and qualified employees according to their capabilities. For example, the savings for a company that creates opportunities for continued employment for a person with MS can be as much as 134,000 euros over a ten-year period [6]. For some people with MS, maintaining a work opportunity that is tailored to them means maintaining the important social work environment and the social recognition that comes with it – and in turn, a positive impact on health status. Finally, the positive economic balance for society through “integration” instead of “invalidization” is proof that it is worthwhile for all sides not to take the supposedly easy paths of exclusion and subsequent minimization of financial support. Professional social support in integration and job retention for people with MS not only helps to reduce the costs of MS-related absenteeism from work (36% of total MS-related costs). The financial benefit to society is as high as 320,000 euros/per person with MS over a ten-year period on the basis of an average retention rate of 50% over this period [6].
Job retention is only one aspect
In the practice of social work of the MS Society, an average of 25 clients per year can remain professionally integrated within the framework of case management together with the respective employer. While job integration may be an improvement for some people with MS, it is important to emphasize that these measures are not appropriate for the majority of people with MS, nor are they the central determinant of quality of life.
Very many people with MS respond to stress and pressure with marked deterioration in their health, and again, generalization is counterproductive. Not all affected individuals and their employers can be included in successful case management – for example, physically demanding work generally leads to earlier retirement: while non-physically working affected individuals were retired on average 12.8 years after diagnosis, this was the case for physically working individuals after eleven years [7]. The medical diagnosis and monitoring are the valid bases for further options.
However, integration means much more than professional integration in the primary labor market. Social integration is the basis for improving the quality of life of those affected and the family system – and thus also the state of health. The importance of social integration for the quality of life of people with MS is demonstrated by Schwartz and Frohner, who found that people with MS without a job did not experience a lower quality of life when they were involved in appropriate activities [5]. The services offered by the MS Society both in the form of events, seminars, vacations, social groups and networking and in the form of nursing, psychological and social work counseling and support meet the requirements for social support for those affected [4].
Motivation and integration: collaboration required
The social participation and integration of people living with MS can be effectively supported by good cooperation between physicians, therapists and the MS society. To focus not on what cannot be done, but on motivating and positive support for those affected and their relatives, is a social task and at the same time a social benefit. The potential and health benefits of integration, support, encouragement and demand for people with MS are great.
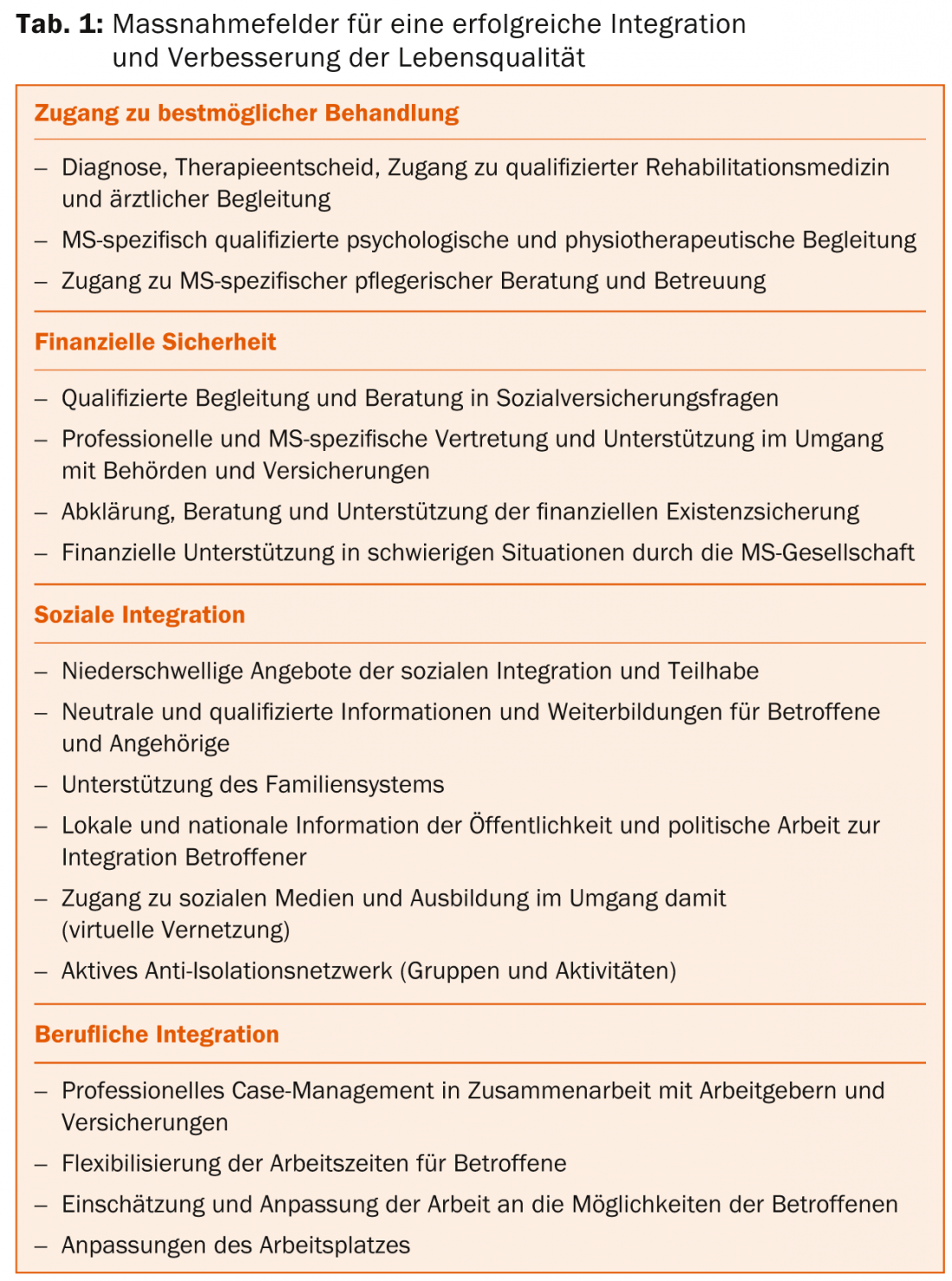
Four areas of action can be defined as the basis for successful integration and improvement of quality of life for people with MS (Table 1).
Close collaboration between physicians, therapists, nurses, health professionals and the MS Society creates an excellent opportunity to engage people with MS in a medically effective and socially supportive network.
To this end, the existing cooperation must be further intensified: The effect of social integration on the health status and well-being of people with MS has been impressively proven. Individual players in the healthcare system are doing important and great work in their field – but it is only when they work together that an anti-isolation network is created: multiple sclerosis becomes “MS” – “More Solidarity”. The important positive effects of this active social solidarity for those affected, their children and relatives can be measured and felt. When visiting a group stay for people with MS in need of care of the Swiss MS Society, one can personally experience how joy of life and quality of life, despite considerable health limitations, are present through care and social integration.
Dr. Christoph Lotter
Prof. Dr. med. Jürg Kesselring
Literature:
- Hakim EA, et al: The social impact of multiple sclerosis – a study of 305 patients and their relatives. Disability and Rehabilitation 2000; 22(6): 288-293.
- Basler Zeitung: With a new name against old stigma. Rehab chief Jürg Kesselring wants to rename the IV to integration insurance. July 11, 2014; 4.
- Tagesanzeiger: The doctor is no longer taken seriously. www.tagesanzeiger.ch/schweiz/standard/Der-Arzt-wird-nicht-mehr-ernst-genommen/story/30521158. Online 30.07.2014.
- Krokavcova M, et al: Social support as a predictor of perceived health status in patients with multiple sclerosis. Patient Education and Counseling 2008; 73: 159-165.
- Schwartz C, Frohner R: Contribution of Demographic, Medical, and Social Support Variables in Predicting the Mental Health Dimension of Quality of Life among People with Multiple Sclerosis. Health & Social Work 2005; 30(2): 203-212.
- Knülle E, et al: From disability to ability at work – Successful case management approaches in multiple sclerosis. Report 2011 Swiss Multiple Sclerosis Society Zurich ISBN: 978-3-908104-17-9. Pfleger CCH,
- Flachs EM, Koch-Henriksen N: Social consequences of multiple sclerosis: clinical and demographic predictors – a historical prospective cohort study. European Journal of Neurology 2010; 17: 1346-1351.
- Steck B, Kappos L, Bürgin D: Psychosocial impact of multiple sclerosis on family and children. Swiss Archives of Neurology and Psychiatry 1999; 150(4): 161-168.
- Castro Costa D, José Sá M, Calheiros JM: The effect of social support on the quality of life of patients with multiple sclerosis. Arq Neuropsiquiatr 2012; 70 (2): 108-113.
InFo NEUROLOGY & PSYCHIATRY 2014; 12(6): 16-19.











