Tailored individual surgical treatment is sought for surgical candidates with low back pain. With fusion surgery, good and very good results can be achieved in selected cases, superior to non-surgical treatment. Minimally invasive techniques reduce morbidity and shorten rehabilitation time. New motion preservation techniques are not superior to fusion surgery. In motion preservation techniques, outcomes after disc arthroplasty are at least as good as those after spondylodesis.
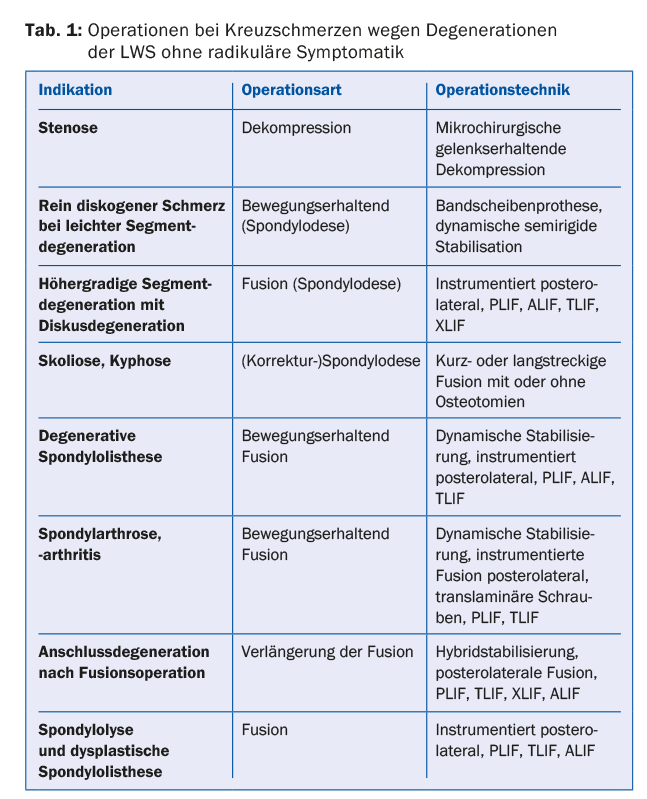
Surgical treatment of low back pain with or without pseudoradicular radiation is controversial. However, if a defined source of pain can be identified with a high degree of probability, the question of eliminating the source of pain also becomes reasonable (Table 1). In general, there is no urgent or compelling indication for surgery in low back pain due to degenerative changes.
Decompression surgery
Microsurgical decompression surgery alone for back pain is an exception. In our experience, however, some patients with spinal stenosis have mainly low back pain and little or no leg pain. In these cases, microsurgical decompression, in which the spinal canal is widened via joint-preserving interlaminar fenestration, can achieve pain relief. The dorsal ligamenta supra- and interspinosus are preserved. Even in “stable spondylolisthesis”, this minimally invasive technique can often achieve a good to very good outcome without the need for instrumented fusion in the course.
Spondylolysis and dysplastic spondylolisthesis.
Spondylolysis and dysplastic spondylolisthesis, although not primarily degenerative, may become symptomatic in late adulthood. Bilateral spondylolysis can cause low back pain, but the prognosis is favorable with nonoperative therapy. Increasing spondylolisthesis in adulthood is rare. However, with increasing disc degeneration and spondylolisthesis, refractory low back pain with or without radicular symptoms may occur. While surgery may be discussed early for radicular pain, six months of conservative therapy should be tried for low back pain alone.
Fusion operation
The most commonly performed surgery for back pain is fusion surgery (spondylodesis) [1]. This immobilizes pain-causing structures, primarily the innervation of the annulus fibrosus and the facet joints. This eliminates mechanical pain caused by inhomogeneous load transfer with pressure peaks on the end plates.
Despite many clinical studies, the usefulness of surgery, especially fusion surgery, for chronic low back pain is critical and controversial [2]. In a systematic review of randomized trials comparing lumbar fusion surgery with nonsurgical treatment, surgery was superior to unstructured conservative therapy but not to cognitive behavioral therapy. Due to the methodological weaknesses of many randomized trials, no conclusive statements can be made in this regard. In the few randomized trials, there are relatively many cross-over patients, small numbers of cases, or no intention-to-treat analysis [2]. Therefore, the superiority of spondylodesis over conservative therapy for low back pain cannot be clearly demonstrated [3–5]. However, in selected cases, good to excellent results are achieved in up to 89% of patients operated on [6–11]. Central to this is patient selection. It is of utmost importance to identify a defined morphologic correlate that, based on the evidence to date, triggers low back pain.
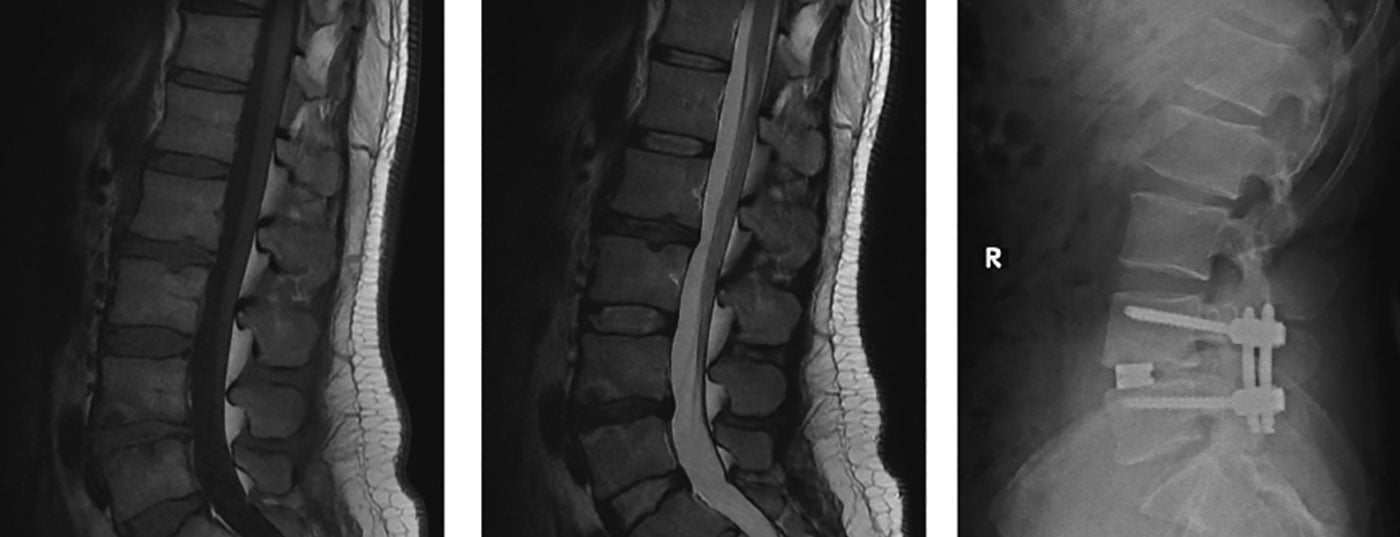
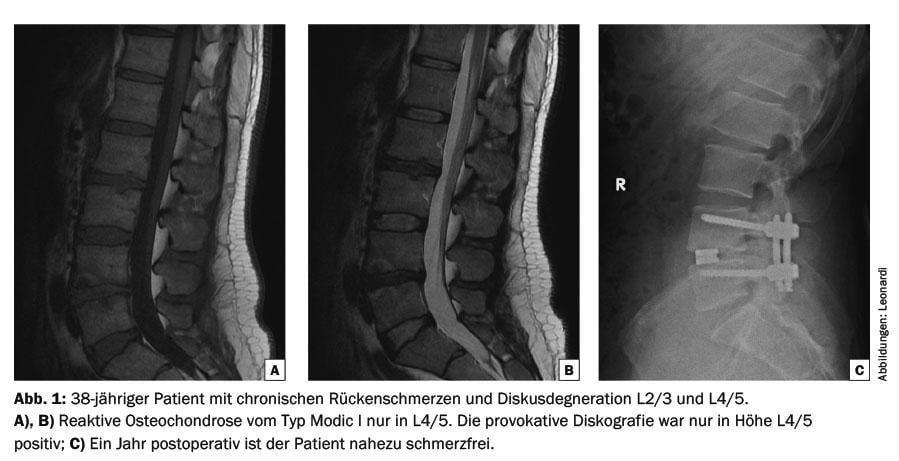
The early postoperative results of the randomized-controlled Swedish Lumbar Spine Study showed a positive effect of fusion compared with patients who received only physiotherapy [12]. Long-term analyses of the same study over 12.8 years showed that three of four primary endpoints had significantly better outcomes for patients who underwent surgery. Differences were most pronounced in cross-over patients [13]. Only in the intention-to-treat analysis were the results not significantly better. There were also no significant differences in secondary outcomes (Oswestry Disability Index [ODI], back pain according to visual analog scale [VAS], work status, pain medication consumption, pain frequency). The authors concluded that, taking into account the Global Assessment, lumbar fusion surgery is a reasonable treatment for chronic low back pain. Thus, if a pathomorphologic correlate for the pain is present, surgery should be considered early to avoid chronicity of the pain. If degenerative changes are present in only one or at most two segments, a good outcome can be expected (Fig. 1) . In contrast, a surgical indication for multisegmental changes is difficult to establish. On the other hand, a 100% fusion rate is not clearly associated with a good or very good outcome, so it is essential to consider other factors for low back pain before surgery [7,12,14].
Non-instrumented fusion
Non-instrumented fusion, i.e. fusion without implant, of two or more vertebrae is rarely used today. Fusion is achieved by bone apposition (with or without bone substitutes) to the posterolateral elements, particularly the facet joints and the transverse process, but may also occur interbody between the discs. This is possible from a posterior, anterior, transforaminal or lateral approach. With non-instrumented fusion, fusion rates are significantly lower than with instrumented fusion, at approximately 50%.
Instrumented fusion
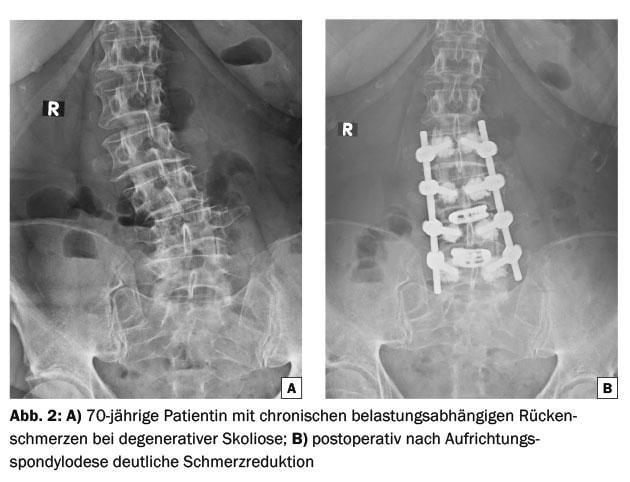
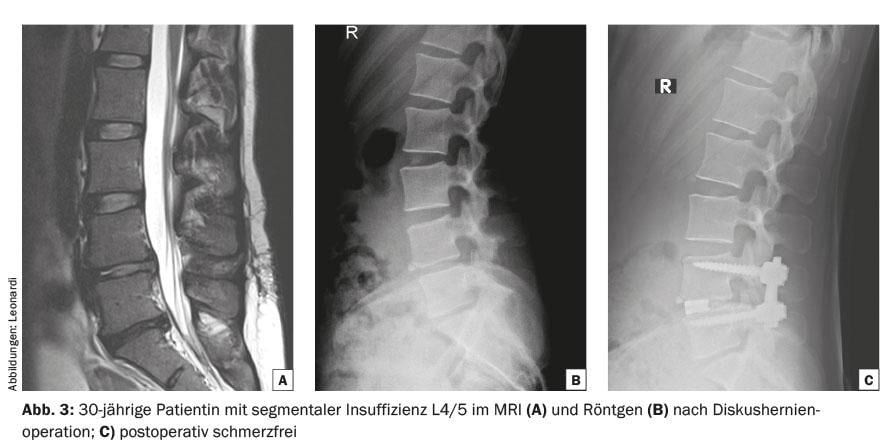
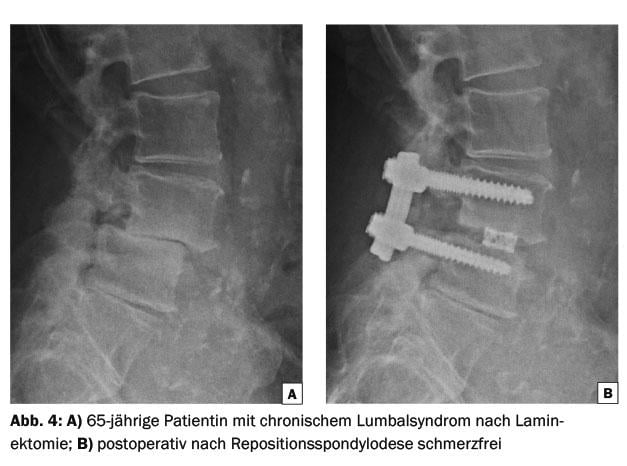
Although the technique has aged somewhat, instrumented fusion remains the gold standard of surgical treatment for low back pain. Two pedicle screws per vertebra are connected to the pedicle screws of the adjacent vertebra via longitudinal rods. In addition, disc evacuation may also be performed between the vertebrae to be fused. So-called cages are then placed in the disc space and filled with bone (Fig. 2-4) . Cage implantation increases primary stability, restores disc height and can widen the neuroforamina. This can increase the fusion rate to over 90%. Some studies show a slightly better outcome with additional cages than without additional cages. This is explained by the fact that in discogenic pain, the pain correlate in the disc is directly switched off.
The disc space for cage implantation can be accessed from posterior, anterior, transforaminal and lateral. Accordingly, the technique is named: Posterior Lumbar Interbody Fusion (PLIF), Anterior Lumbar Interbody Fusion via a retroperitoneal approach (ALIF), Transforaminal Interbody Lumbar Fusion (TLIF), and Extreme Lateral Interbody Fusion via a lumbotomy (XLIF). Postoperative rest for approximately six weeks is recommended. Heavy physical exertion and flexion, extension and rotational movements with the upper body should be avoided for three months.
None of the instrumented fusion techniques was shown to be superior to any other in terms of clinical outcome. It is important to find the best tailored technique for each patient once the indication is given.
Minimally invasive approaches for fusion
Technical advancements also enable minimally invasive techniques in spine surgery. Minimally invasive here refers to access. The goal of surgery must be achieved at the site of pathology as safely as with the open method. However, minimally invasive approaches lower access morbidity: they primarily reduce blood loss, shorten convalescence, and accelerate return to work. In particular, the insertion of pedicle screws by percutaneous techniques (stab incision and dilatation cannulas) has proven effective. This can significantly spare the paravertebral muscles and reduce blood loss.
Connection degeneration after mergers
Above a fusion, biomechanical overloading of the segment occurs. To date, evidence is lacking as to whether this connection degeneration is favored by fusion or whether it is the natural progression of degeneration [15]. Ghiselli reports a rate of reoperation for follow-up problems of 16.5% after five years and 36.1% after ten years [16]. He estimates the risk of reoperation for connection degeneration at 3.9% per year.
Motion preservation techniques
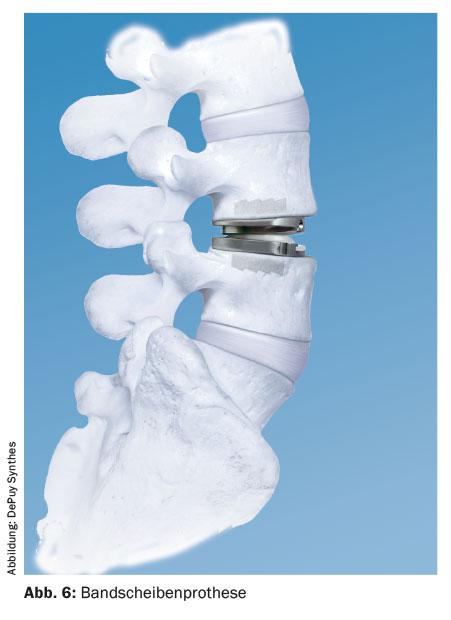
Since the lumbar spine is a motion segment, it is obvious to perform the rehabilitation with a motion preserving implant or technique. However, the mobility of the motion segment is very individual. Therefore, it is not known when a motion segment is unstable or which individual mobility resp. stiffness of a single motion segment is necessary. Movement-preserving techniques are divided into dynamic stabilizations (Fig. 5), which can also be combined with rigid ones (hybrid solutions), and disc prostheses (Fig. 6).
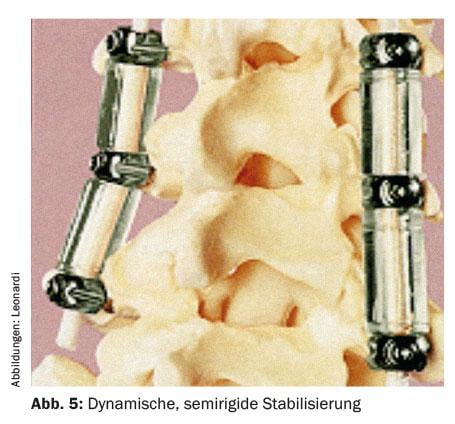
Dynamic stabilization
Indications in which dynamic stabilization might be useful are minor segmental degenerations (first-degree degenerative spondylolistheses, stenoses), both isolated and those at the end of a prolonged rigid fusion (hybrid stabilization). Some spine surgeons use dynamic stabilization at the cranial end of a fusion to protect the connecting segment. Overall, however, the indications are not clearly defined.
There are various systems on the market for dynamic stabilization. A widely used system (Dynesys), which has been in use for many years, consists of pedicle screws connected to a buffer made of polyurethane. In the buffer runs a cord made of polyethylene, which is anchored to the screw heads. The system allows a small extension and flexion of the motion segment, but is biomechanically stiffer than the physiological motion segment. Bone apposition is omitted, but nevertheless, connection degeneration or even fusion between the vertebrae has not infrequently been observed. Unfortunately, revision surgeries were often necessary due to pedicle screw loosening [17,18].
This system, as well as many others, is often implanted as an adjunct after decompression surgery for radicular symptoms. Thus, a comparison with fusion surgery used only in back pain patients cannot be made.
The ideal motion preserving implant does not yet exist. To date, there are no data demonstrating fewer connection problems after the use of motion preserving stabilizations or after hybrid stabilizations.
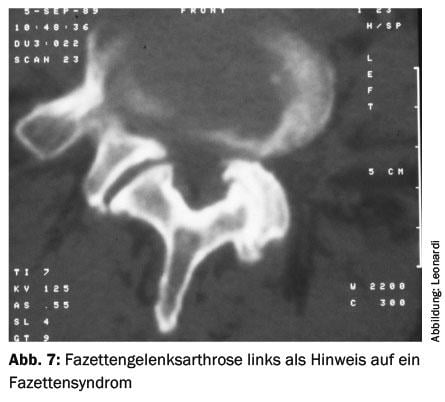
Facet joint prosthesis
The indication for a facet joint prosthesis is severe facet joint arthrosis with corresponding facet syndrome (Fig. 7) . However, the technique is still in the experimental phase. The anchoring in particular could be a weak point.
Interspinous implants
Interspinous implants are inserted between two spinous processes. Primarily, these implants were developed for stabilization after decompression surgery for stenosis. Secondarily, the indication was also extended to back pain patients. The implantation of these implants in stenosis and in so-called instabilities with back pain is controversial. It is not clear when which patient will benefit. The clinical utility is therefore questioned [19].
Intervertebral disc prostheses
Disc prostheses are designed to preserve segmental mobility as opposed to fusion, even if they do not exactly restore individual biomechanics. It is hoped that this technique will reduce the problem of follow-up degeneration after fusion surgery, but this has not yet been proven. The main indication is back pain (purely discogenic pain) with the motion segment still relatively well preserved. Severe disc degeneration and facet joint arthrosis are not good indications. Contraindications include osteoporosis, elderly patients, multisegmental degeneration, deformities, instability, higher grade spondylolisthesis, and extreme obesity. The disc prosthesis is implanted exclusively via a ventral, usually retroperitoneal approach.
For the corresponding same indication, randomized controlled trials (RCTs) showed that the clinical outcome for both 1- and 2-level disc prostheses was at least equivalent to fusion surgery [20–23]. There are hardly any RCTs that allow a conclusive statement [7]. A meta-analysis of five RCTs with 837 patients failed to show that prosthesis patients had a significantly better outcome than fusion patients. Patients with disc prostheses had a non-significantly better outcome on ODI and VAS. Patient satisfaction was higher in patients with prosthesis. However, when one of these five studies was excluded, there were no longer any differences. Thus, the benefit of motion preservation has not been clearly demonstrated [24].
The good results after operations with disc prostheses can only be partially compared with fusion operations. The majority of patients in a spine surgery practice who are candidates for fusion surgery are not also candidates for implantation of a disc prosthesis. Thus, the prosthesis is an alternative to fusion only in individual cases. In principle, indications for fusions are much more frequent than for disc prostheses: The incidence of an indication for prostheses in assigned patients was only 0.5% in one study [25]. Even if disc prostheses have a biomechanically more favorable loading profile compared with fusion, follow-up studies also observed follow-up degeneration after implantation of a disc prosthesis [26,27].
Back pain in case of decompensation of the sagittal perpendicular
With age, the center of gravity shifts forward. At the same time, disc degeneration increases in the ventral disc segment. This results in a decrease in lumbar spine lordosis and an increase in thoracic spine kyphosis. The musculature tries to counteract this ventral perpendicular displacement with ventral traction, but after a short time the musculature becomes overloaded with pain. Not all people with this unfavorable biomechanical constellation get back pain. However, in patients who have exhausted pain management and are significantly disabled, long-axis corrective spondylodesis may be discussed. Because it is major surgery, it is only considered in otherwise healthy patients with no or few comorbidities.
Part 1 of this article appeared in issue 2/2016 of HAUSARZT PRAXIS.
Literature:
- Deyo RA, et al: Low back pain. N Engl J Med 2001; 344: 363-370.
- Mirza SK, Deyo RA: Systematic review of randomized trials comparing lumbar fusion surgery to nonoperative care for treatment of chronic back pain. Spine 2007; 32(7): 816-823.
- Brox JI, et al: Lumbar instrumented fusion compared with cognitive intervention and exercises in patients with chronic back pain after previous surgery for disc herniation: a prospective randomized controlled study. Pain 2006; 122(1-2): 145-155.
- Brox JL, et al: Randomized control trial of lumbar instrumented fusion and cognitive intervention and exercises in patients with chronic low back pain and disc degeneration. Spine 2003; 28(17): 1913-1921.
- Mannion AF, et al: Comparison of spinal fusion and nonoperative treatment in patients with chronic low back pain: long term follow-up of three randomized controlled trials. Spinal J 2013; 13(11): 1438-1448.
- Gibson JN, et al: The Cochrane review of surgery for lumbar disc prolapse and degnerative lumbar spondylosis. Spine 1999; 24: 1820-1832.
- Gibson JN, et al: Surgery for degenerative lumbar spondylosis: updated Cochrane review. Spine 2005; 30: 2312-2320.
- Parker LM, et al: The outcome of posterolateral fusion in highly selected patients with discogenic low back pain. Spine 1996; 21: 1909-1916.
- Colhoun E, et al: Provocative discography as a guide to planning operations on the spine. JBJS Br 1988; 70: 267-270.
- Blumenthal SL, et al: The role of anterior lumbar fusion for internal disc disruption. Spine 1988; 13: 566-569.
- van Tulder MW, et al: Outcome of invasive treatment modalities on back pain and sciatica: an evidence-based review. Eur Spine J 2006; 15 Suppl 1: S82-92.
- Fritzell P, et al: Volvo Award Winner in Clinical Studies: lumbar fusion versus nonsurgical treatment for low back pain: a multicenter randomized controlled trial from the Swedish Lumbar spine study Group. Spine 2001; 26: 2521-2534.
- Fritzell P, et al: Fusion as treatment for chronic low back pain – existing evidence, the scientific frontier and research strategies. Eur Spine J 2005; 14(5): 519-520.
- Fritzell P, et al: Chronic low back pain an fusion: a comparison of three surgical techniques: a prospective multicenter randomized study from the Swedish lumbar spine study group. Spine 2002; 27: 1131-1141.
- Kumar MN: Correlation betweeen sagittal plane changes and adjacent segment degneration following lumbar spine fusion. Eur Spine J 2001; 10: 314-319.
- Ghiselli G, et al: Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am 2004; 86-A: 1497-1503.
- Bothmann M, et al: Dynesys fixation for lumbar spine degeneration. Neurosurg Rev 2008; 31: 189-196.
- Beastall J, et al: The Dynesys lumbar spinal stabilization system: a preliminary report on positional magnetic resonance imaging findings. Spine 2007; 32: 685-690.
- Gillet P: Comment on “long-term acturarial survivorship analysis of an interspinous stabilization system”. Eur Spine J 2007; 16(8): 1289-1290.
- Blumenthal S, et al: A prospective, randomized, multicenter Food & Drug Administration investigational device exemptions study of lumbar total disc replacement wih the Charite artificial disc versus lumbar fusion: part I: evaluation of clinical outcomes. Spine 2005; 30: 1565-1575, E387-391.
- Delamarter R, et al: Five year results of the prospective randomized multicenter FDA DIE Prodisc-l clinical trial. Spine J 2008; 8: 62S-63S.
- Guyer RD, et al: Prospective, randomized, multicenter Food & Drug Administration investigational device exemptions study of lumbar total disc replacement wih the Charite artificial disc versus lumbar fusion: five-year follow-up. Spine J 2009; 9: 374-386.
- Ziegler J, et al: Results of prospective, randomized, multicenter Food & Drug Administration investigational device exemption study of he proDISC L total disc replacement versus circumferential fusion for the treatement of 1-level degnerative disc disease. Spine 2007; 32: 1155-1163.
- Yajun WU, et al: A meta-analysis of artificial total disc replacement versus fusion for lumbar degnerative disc disease. Eur Spine J 2010; 19: 1250-1261.
- Kingsley, RC: Epidemiology of indications and contraindications to total disc replacement in an academic practice. Spine J 2007; 7: 392.
- Putzier M, et al: Charite total disc replacement – clinical and radiological results after an average follow up of 17 years. Eur Spine J 2006; 15: 183-195.
- Huang RC, et al: Range of motion and adjacent level degeneration after lumbar total disc replacement. Spine J 2006; 6: 242-247.
GP PRACTICE 2016, 11(3): 37-42