Hymenoptera venom allergy – commonly called insect venom allergy – is one of the so-called “Big 3” of severe allergic reactions, along with food and drug allergies. No one is immune: the risk of anaphylactic reaction after a bee or wasp sting is estimated at about 5%, and the recurrence rate is not insignificant. Anyone who has had a systemic reaction should therefore always have an emergency kit at hand.
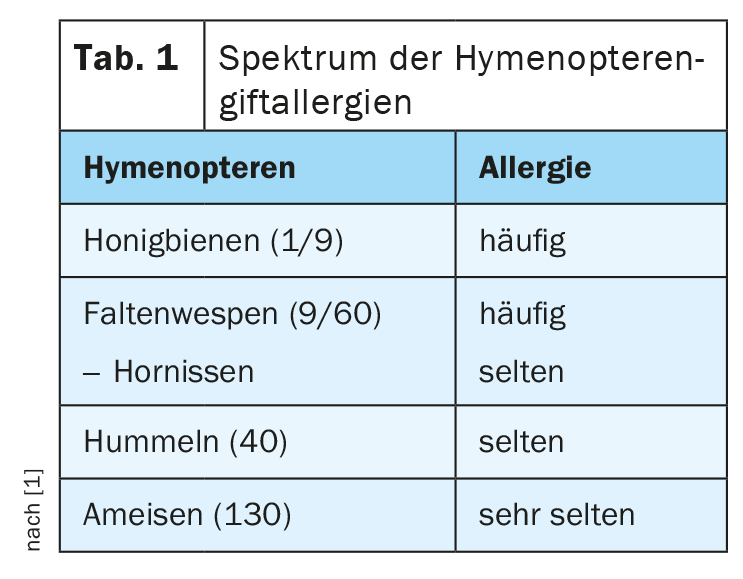
The next summer is sure to come – and with it the Hymenoptera. In our latitudes, stings from bees and wasps are relatively common. In Switzerland, nine different species of wasps are known (out of a total of around 60) that sting and can cause allergic reactions. However, bumblebees and ants can also cause allergies, although this happens rather rarely (Tab. 1) . Ants are counted among the hymenoptera because they have wings before they build their nests. These are not shed until the nest is built.
Hymenoptera venom allergies are classified as accidents. According to the Swiss accident insurance company Suva, more than 10,000 such accidents due to hymenopteran stings occur every year, causing annual costs of about 20 million CHF (the average cost per accident is estimated at about 750 CHF). Regardless of whether it is a bee or wasp sting, about one in ten stings triggers an allergy. About 40 stings per year result in reactions so severe that work absences of >3 months occur. “These severe cases may be accompanied by paralysis, cerebral stroke or myocardial infarction, which not only has serious consequences for the affected person, but is also statistically significant with high costs,” explained Prof. Dr. Arthur Helbling, University Department of Pneumology and Allergology at the Inselspital Bern [1]. In such cases, the clarification is rarely carried out via the accident insurance, but as a rule via the health insurance.
Evaluate severe reactions allergologically
Any severe reaction such as airway obstruction, dyspnea, or circulatory involvement should be evaluated by an allergist for allergen-specific immunotherapy (VIT). If, on the other hand, a patient reacts only locally, e.g. by swelling after a prick in the tongue, this is unpleasant for the person concerned, but does not need to be clarified, as it does not entail any therapeutic consequences. In such cases, he said, prophylaxis rather than diagnosis or treatment should be considered.
For individuals who have exhibited systemic allergic reactions (SAR) – whether involving the skin, gastrointestinal tract, respiratory system, or circulatory system – Prof. Helbling strongly advises carrying kits of emergency medications. This would include an epinephrine auto-injector. “Even mild systemic reactions such as urticaria are associated with a fourfold increased risk of recurrence. If a shock reaction has been suffered, the risk of recurrence with a next sting is 50-70%. From these numbers alone, you can already see the point of VIT.” Treatment with bee or wasp venom lasts at least 5 years. Successful VIT reduces the risk of relapse, but the effect does not last a lifetime. It is believed that the risk after aborting a VIT is about 10% per stitch.
Take-Home Messages
- Insect venom allergy is a common cause of anaphylaxis – and it
can affect anyone. - Any more severe reaction should be allergologically evaluated for VIT.
Evaluate. - After anaphylaxis, equip each patient with emergency medication/epinephrine auto-injector.
- Even after completion of successful VIT for 5 years, relapse of SAR is possible.
Source: 1st FomF – WebUp 6 highlights in 60 minutes “Update Allergology”, lecture “Hymenoptera venom allergies”, 12.12.2022.
InFo PNEUMOLOGY & ALLERGOLOGY 2023; 5(1): 23 (published 2/23/22, ahead of print)











