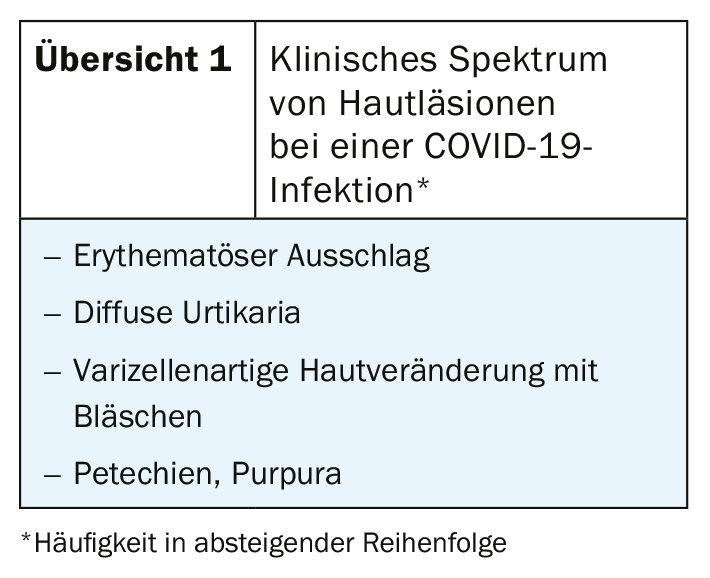
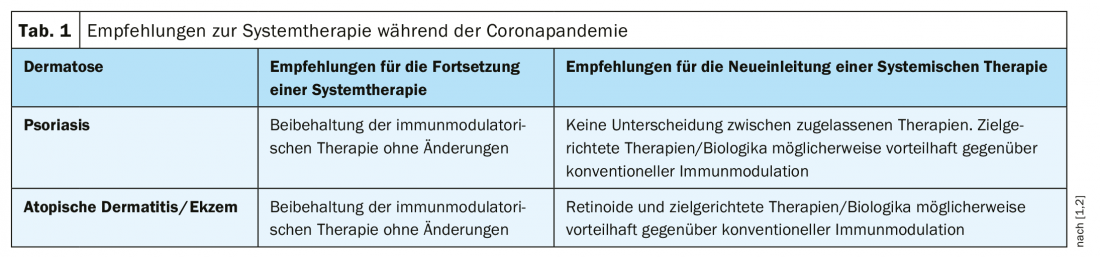
Based on current data and pathophysiologic considerations, recommendations for the management of patients during the pandemic are continually updated by professional societies. So also for common skin diseases with complex immunological pathogenesis. In particular, it addresses the question of what should be considered in patients on systemic therapy or with regard to the initiation of such therapy.
When it comes to treatments of primary dermatoses that interfere with the immunologic response, the treatment decision may be tangential. Which treatments are safe and what should be considered in terms of risk-benefit balance? Prof. Dr. med. Margitta Worm, Charité Medizin Berlin, spoke on this topic at a web event of the FomF (D), Dermatology and Allergology Refershers [1].
Maintain symptom control, avoid exacerbations
As with psoriasis, immunomodulatory therapies should generally be continued in atopic dermatitis [2]. With regard to initiating new systemic therapy, retinoids or dupilumab tend to be preferable to treatment with conventional systemic therapeutics because they have a lesser impact on the immune response to viral infection [2,3]. Since exacerbations of the underlying disease could have a negative impact on immunity, it is important to control symptoms as well as possible, which argues for continuing immunomodulatory treatments [4]. In addition, general precautions and hygiene measures should be followed. In the context of frequent hand washing, patients should be reminded to perform basic skin care consistently including moisturizing skin care products.
For patients with established COVID-19 disease, a June issue of the JEADV COVID-19 Special Forum recommends the following [4]: Whether or not to interrupt immunomodulatory therapy should be decided based on an interdisciplinary risk assessment and guideline recommendations. It is also important to consider that immunomodulators for the treatment of atopic dermatitis may also influence any comorbidities that may be present, such as asthma, chronic obstructive pulmonary disease, eosinophilic esophagitis, renal disease, and severe allergies, and the abrupt discontinuation of a stable systemic treatment regimen may lead to exacerbations in this regard. If the decision is made to discontinue systemic treatment of atopic dermatitis, patients should be provided with topical therapy that is as effective as possible so that flares can be prevented. It is also important to monitor and treat any comorbidities, such as asthma.
Literature:
- Worm M: COVID-19: Significance for dermatology and allergology. Prof. Dr. med. Margitta Worm, Dermatology and Allergology Refresher, FomF.de, Hofheim (D), 10.09.2020.
- Buhl T, et al: COVID-19 and implications for dermatological and allergological diseases. JDDG 2020;18(8): 815-825.
- Ruzicka T, et al: Efficacy and safety of oral alitretinoin (9-cis retinoic acid) in patients with severe chronic hand eczema refractory to topical corticosteroids: results of a randomized, double-blind, placebo-controlled, multicentre trial. Br J Dermatol 2008; 158: 808-17.
- Wollenberg A, et al: European Task Force on Atopic Dermatitis statement on severe acute respiratory syndrome coronavirus 2 (SARS-Cov-2) infection and atopic dermatitis. COVID-19 SPECIAL FORUM. JEADV 2020; 34(6): e241-e242.
- De Giorgi V: Cutaneous manifestations related to coronavirus disease 2019 (COVID-19): A prospective study from China and Italy. J Am Acad Dermatol 2020; 83(2): 674-675.
DERMATOLOGY PRACTICE 2020; 30(5): 4