The classic problem areas of psoriasis such as the scalp, palms of the hands, soles of the feet, nails, face and genital area are also referred to as “difficult to treat areas”. Prof. Dr. med. Nikhil Yawalkar, Inselspital Bern, gave an up-to-date overview of what needs to be considered in the case of psoriasis in these locations and which treatment options are most promising.
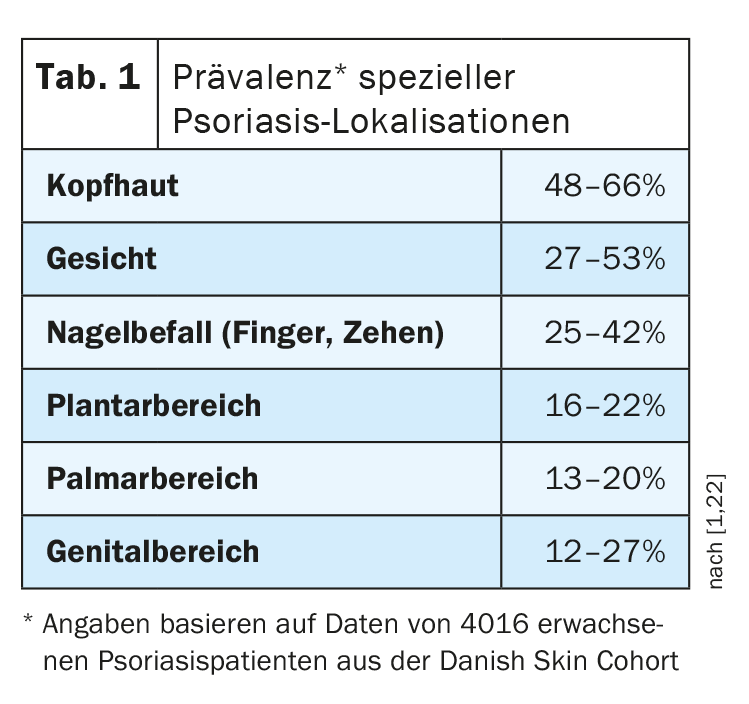
Psoriasis infestation of specific localizations occurs relatively frequently, reported Prof. Yawalkar (Table 1). As the quality of life is particularly impaired when the corresponding skin areas are affected and topical treatment can prove difficult in some cases, these were defined in the S3 guideline as upgrade criteria for classification as moderate to severe psoriasis, explained Prof. Yawalkar. This is significant in that affected patients fulfill the requirements for systemic therapy, even if the values for PASI (Psoriasis Area and Severity Index) and BSA (Body Surface Area) are less than 10 and less than 10% respectively [1]. There are cases where the PASI is 4 or 5, but the upgrade criteria are met, the speaker explained. There are both topical and systemic treatment options for all localizations.
Nail psoriasis
Nail infestation also occurs in 5% of cases in isolation and patients often have infestation of the nails prior to psoriatic arthritis (PsA). “This is an important predictor,” explained Prof. Yawalkar. Studies have shown that over 90% of patients with PsA have nail psoriasis (Fig. 1) [2]. This should be taken into account when assessing the findings and history of these patients. However, scalp infestation and lesions in the rima (ani-/perianal) are also associated with a higher risk of PsA [3]. A distinction is made between changes in the matrix (spotted nails, leukonychia, thickening of the nail plate, nail dystrophy or erythema in the lunula) and changes in the nail bed (oil stains, onycholysis, splinter hemorrhages, subungual hyperkeratosis) [4]. In terms of differential diagnosis, onychomycosis should be considered in particular, although there are also cases where this occurs simultaneously with nail psoriasis.
If only a few nails are slightly affected, a local treatment consisting of a fixed combination preparation of calcipotriol plus betamethasone diproprionate (Daivobet ointment®, Enstilar foam®) is usually used, Prof. Yawalkar explained [1,5]. The foam is a little more difficult to apply than the ointment. Intralesional corticosteroids can also be used, but are very painful, the speaker reported [1].
With regard to conventional systemic therapeutics, acitretin or methotrexate (MTX) are the main options. For acitretin, the speaker recommends a rather low dosage of 0.2-0.3 mg/kg/day over a period of 6-12 months; for MTX, 15-25 mg per week is suggested [1,6]. Ciclosporin (3-5 mg/kg/day) is now only rarely used. There are also some reports of successful treatment with dimethyl fumarate (average dose 294 mg/day) or apremilast (2×30 mg) [6].
Prof. Yawalkar emphasized that the presence of comorbidities is an important criterion in the selection of biologics for treatment [1]. In patients with PsA, he favors TNF-alpha blockers or IL-17 inhibitors, otherwise IL-23 inhibitors are also an option. “If you really want to achieve something with the nails, you usually have to treat them systemically,” summarized the speaker [1]. Last year, a network meta-analysis and a real-world study were published in which various monoclonal antibodies were compared in nail psoriasis [23,24] (box) .
| Biologics for nail psoriasis In a network meta-analysis of biologics for nail psoriasis published in 2023, adalimumab performed similarly well to IL-17 and IL-23 inhibitors [23]. And Prof. Yawalkar described the case of a 36-year-old man who had had plaque psoriasis with nail involvement mainly in the area of the hands for 10 years and in whom treatment attempts with topicals, phototherapy and acitretin were not sufficiently effective. The patient, who worked professionally as a tiler, was referred to a rheumatologist due to dactylitis, who diagnosed psoriatic arthritis. In the end, treatment with the TNF-alpha blocker adalimumab was agreed upon and a good response to therapy was achieved. In a real-world study also published last year comparing various biologics for nail psoriasis, IL-17 inhibitors (ixekizumab, secukinumab) achieved the best results, followed by the IL-12/23 inhibitor ustekinumab, the TNF-alpha blocker adalimumab and the IL-23 inhibitors [24]. |
In addition to drug therapy and the use of care ointments in the area of the nail folds and the nail surface, there are also some general measures that can help to improve the appearance. This includes keeping the nails short (especially in the area of onycholysis); avoiding mechanical stress, manipulation and nail extension; not wearing high heels; wearing gloves when working in damp conditions [7].
Palmoplantar psoriasis
A combination therapy is often required for palmoplantar psoriasis, the speaker emphasized and added: “For example, topical steroids with vitamin D analogues” [1,8]. Suitable preparations include Daivobet® and Enstilar® [1,5]. However, he advises against the use of vitamin D analogs in hyperkeratotic forms, as they can have an irritating effect. Instead, Dermovate® could be prescribed occlusively, for example. Tinctures made from tar brushes can also be very effective, but they are not easy to apply. Here too, the speaker recommends a combination therapy, e.g. low-dose acitretin plus tar brushing. Another treatment option is phototherapy (low dose acitretin + bathing PUVA) as an add-on to local therapy.
With regard to systemic therapeutics, a pooled analysis of the ESTEEM study program showed that around half of the patients treated with apremilast (Otezla®) achieved completely or almost completely appearance-free skin (PPPGA value 0/1) at week 16 [9].
Prof. Yawalkar described the case of a 60-year-old man who suffered from plaque psoriasis mainly in the area of his hands and feet and felt that his quality of life was severely restricted [1]. Therapy trials with topicals, bathing PUVA and acitretin were unsatisfactory. As the patient had latent tuberculosis and an aversion to injections, it was decided to treat him with Apremilast, which led to very good treatment results. In addition to apremilast (30 mg, 2×/d), methotrexate (10-25 mg/week), ciclosporin (3-5 mg/day) or dimethyl fumarate (240-360 mg/day) can also be used for palmoplantar psoriasis [8,10]. “You can achieve a lot more with biologics,” says the speaker [1] (box) . “A low-dose acitretin plus a biologic works well over a longer period of time in most cases”.
| Biologics for palmoplantar psoriasis In the GESTURE study, the response rates with secukinumab 300 mg (n=69) and secukinumab 150 mg (n=68) were 51.6% and 29.7% respectively at week 40 and 59.2% and 52.5% respectively after a treatment period of 132 weeks [26]. Prof. Yawalkar concluded that it would take some time. Long-term data on the use of bimekizumab and risankizumab in palmoplantar psoriasis was collected over even longer periods of time. For bimekizumab, an IGA 0 response rate of 92% was reported at week 144, and for risankizumab, the proportion with a Palmoplantar Psoriasis Severity Index score of 0 was 81.6% at week 256 [27,28]. If palmoplantar psoriasis proves to be persistent, the use of an IL-17 or IL-23 inhibitor should be considered, the speaker suggested [1]. |
Psoriasis capitis
Head infestations can lead to hair loss and scarring if the inflammation is very severe. Initially, a desquamation is usually carried out, for example with Lotio decapans® overnight with a bathing cap. Then apply a shampoo, preferably without wetting the hair first. Various preparations are available for this purpose: Zinc pyrithione (Squa-med®), selenium disulfide (Dercos Anti-Dandruff), ichthyol (Lubex Ichthyol®), ketoconazole (Lur®), clobetasol proprionate (Clobex®) [5,11,12]. The use of a fixed combination of calcipotriol and betamethasone (Daivobet Gel®, Enstilar Foam®) has proven effective as an anti-inflammatory topical therapy. When used daily over several weeks, it is a very effective treatment option, as study data show [13]. Alternatively, Clarelux Foam® can also be used. The anti-inflammatory active ingredient it contains is a class IV corticosteroid [11,12]. Maintenance therapy is very important, emphasized Prof. Yawalkar [1,14]. The frequency of application can be reduced to twice a week.
In systemic therapies, long-term studies show that 50-60% of patients treated with apremilast (30 mg, 2×/d) maintained a ScPGA 0/1 response up to week 52 [15,16]. MTX could also be tried; it is effective in around a fifth of patients and relatively inexpensive. With biologics, secukinumab 300 mg (n=51) achieved an IGA 0/1 in 60.8% at week 16, with this response rate increasing to 62.7 by week 24 [17]. Similarly high response rates were achieved with guselkumab [17–19].
Infestation of the facial area
Psoriasis lesions on the facial skin can initially be treated with a class II to III TCS (Prednitop®, Elocom®/Monovo®/Ovixan®) [5,12]. As part of proactive treatment, the patient is then usually switched to maintenance therapy with topical calcineurin inhibitors (TCI) in order to avoid the development of skin atrophy as a possible side effect of TCS in long-term use. TCIs such as tacrolimus and pimecrolimus (Protopic® ointment, Elidel® cream) influence the activation of T cells, keratinocytes and mast cells [5,12]. It is not uncommon for a seborrheic component to be present, which should also be treated, for example with Nizoral® cream or Mycoster® cream [5,12].
Genital and perianal area
Initially, induction therapy with topical corticosteroids is also used here, possibly combined with antimycotics. Suitable preparations are Prednitop®, Elocom/Monovo/Ovixan® combined with Travocort® cream or Nystalocal® cream [1,5]. For maintenance therapy, proactive therapy with TCI (Protopic® ointment, Elidel® cream) has proven successful, which can be combined with sitz baths (Tannosynt® liquid) and zinc cream as skin protection [1,5]. If necessary, systemic therapy can also be considered, although there is less evidence than for other localizations. In a study on apremilast, a modified genital PGA response was achieved in 39.6% in the verum arm at week 16 and in 19.5% with placebo. [20]. Treatment with the IL-17 inhibitor ixekizumab resulted in appearance-free skin (sPGA genitalia 0/1) in 73% of study participants at week 12 [21].
Congress: Swiss Derma Day and STI reviews and updates
Literature:
- “Psoriasis: Treatment of difficult body localizations”, Inflammatory dermatoses, Prof. Dr. med. Nikhil Yawalkar, Swiss Derma Day and STI reviews and updates, 11.01.2024.
- Scarpa R, et al: Nail and distal interphalangeal joint in psoriatic arthritis. J Rheumatol 2006; 33(7): 1315-1319.
- Wilson FC et al: Incidence and clinical predictors of psoriatic arthritis in patients with psoriasis: a population-based study. Arthritis Rheum 2009; 61(2): 233-239.
- Haneke E: Nail psoriasis: clinical features, pathogenesis, differential diagnoses, and management. Psoriasis (Auckl) 2017; 7: 51-63.
- Swismedic: Medicinal product information, www.swissmedicinfo.ch,(last accessed 14.03.2024).
- Battista T, et al: Nail Psoriasis: An Updated Review of Currently Available Systemic Treatments. Clin Cosmet Investig Dermatol 2023; 16: 1899-1932.
- Rigopoulos D, et al: Recommendations for the definition, evaluation, and treatment of nail psoriasis in adult patients with no or mild skin psoriasis: A dermatologist and nail expert group consensus. JAAD 2019; 81(1): 228-240.
- Raposo I, Torres T: Palmoplantar Psoriasis and Palmoplantar Pustulosis: Current Treatment and Future Prospects. Am J Clin Dermatol 2016; 17(4): 349-358.
- Bissonnette R, et al: Apremilast, an oral phosphodiesterase-4 inhibitor, in the treatment of palmoplantar psoriasis: Results of a pooled analysis from phase II PSOR-005 and phase III Efficacy and Safety Trial Evaluating the Effects of Apremilast in Psoriasis (ESTEEM) clinical trials in patients with moderate to severe psoriasis. JAAD 2016; 75(1): 99-105.
- Sanchez IM, et al: The Efficacy of Biologic Therapy for the Management of Palmoplantar Psoriasis and Palmoplantar Pustulosis: A Systematic Review. Dermatol Ther (Heidelberg) 2017; 7(4): 425-446.
- Schlager JG, et al: Topical treatments for scalp psoriasis: summary of a Cochrane Systematic Review. Br J Dermatol 2017; 176(3): 604-614.
- Maul J-T, et al: Topical Treatment of Psoriasis Vulgaris: The Swiss Treatment Pathway. Dermatology 2021; 237: 166-178.
- Lebwohl M, et al: Fixed Combination Aerosol Foam Calcipotriene 0.005% (Cal) Plus Betamethasone Dipropionate 0.064% (BD) is More Efficacious than Cal or BD Aerosol Foam Alone for Psoriasis Vulgaris: A Randomized, Double-blind, Multicenter, Three-arm, Phase 2 Study. J Clin Aesthet Dermatol 2016; 9(2): 34-41.
- Régnier A, Trüeb RM: Efficacy of Calcipotriol/Betamethasone Dipropionate Fixed-Combination Aerosol Foam in the Treatment of Localized Scalp Psoriasis: A Real-Life Case Series from Switzerland. Dermatol Ther (Heidelb) 2022; 12(9): 2181-2188.
- Rich P, et al: Apremilast, an oral phosphodiesterase 4 inhibitor, in patients with difficult-to-treat nail and scalp psoriasis: Results of 2 phase III randomized, controlled trials (ESTEEM 1 and ESTEEM 2). JAAD 2016; 74(1): 134-142.
- Crowley J et al. P 894, AAD Annual Meeting 2015, San Francisco.
- Bagel J, et al: The effect of secukinumab on moderate-to-severe scalp psoriasis: Results of a 24-week, randomized, double-blind, placebo-controlled phase 3b study. JAAD 2017; 77(4): 667-674.
- Blauvelt A, et al: P 4768, AAD Annual Meeting 2017, Orlando.
- Reich K, et al: P4827, AAD Annual Meeting 2017, Orlando.
- Merola JF, et al: Efficacy and safety of apremilast in patients with moderate-to-severe genital psoriasis: Results from DISCREET, a phase 3 randomized, double-blind, placebo-controlled trial. JAAD 2024; 90(3): 485-493.
- Ryan C, et al: IXORA-Q Study Group. Efficacy and safety of ixekizumab in a randomized, double-blinded, placebo-controlled phase IIIb study of patients with moderate-to-severe genital psoriasis. Br J Dermatol 2018; 179(4): 844-852.
- Egeberg A, et al: Epidemiology of psoriasis in hard-to-treat body locations: data from the Danish skin cohort. BMC Dermatol 2020; 20(1): 3.
- Egeberg A, et al: Network meta-analysis comparing the efficacy of biologic treatments for achieving complete resolution of nail psoriasis at 24-28 and 48-52 weeks. J Dermatol Treat 2023; 34(1): 2263108.
- Piaserico S, et al: Comparative effectiveness of biologics for patients with moderate-to-severe psoriasis and special area involvement: week 12 results from the observational Psoriasis Study of Health Outcomes (PSoHO). Front Med (Lausanne) 2023 Jun 29; 10: 1185523.
- Krajewska-Wlodarczyk M, Owczarczyk-Saczonek A: Usefulness of ultrasound examination in the assessment oft he nail apparatus in psoriasis. Int J Environ Res Publich Health 2022; 19: 5611. www.mdpi.com/1660-4601/19/9/5611/htm,(last accessed 14.03.2024)
- Gottlieb A, et al: Secukinumab shows significant efficacy in palmoplantar psoriasis: Results from GESTURE, a randomized controlled trial. JAAD 2017; 76(1): 70-80.
- Merola J, et al: Poster presentation, EADV Annual Meeting 2023, Berlin.
- Elewski BE, et al: Poster presentation, EADV Annual Meeting 2022, Milan.
DERMATOLOGY PRACTICE 2024; 34(2): 24-27 (published on 26.4.24, ahead of print)