In more than half of all patients with lung cancer, metastases are already present at the time of diagnosis. In recent years, new compounds have been developed that can be targeted to patients with metastatic non-small cell lung cancer and oncogenic mutations. Dr. med. Martin Früh, St. Gallen, informed in his presentation about the current possibilities and the future prospects.
In non-small cell lung cancer (NSCLC), histology is critical for planning systemic therapy. In patients with squamous cell carcinoma, molecular testing and therapies with pemetrexed (Alimta®) resp. Bevacizumab (Avastin®) is not useful. Recent studies show a small survival benefit in patients with squamous cell carcinoma when necitumumab is added to first-line chemotherapy (gemcitabine plus cisplatin) or When adding ramucirumab to docetaxel therapy in the second-line setting.
In our latitudes, only about 15% of patients can benefit from the new mutation-targeted therapies. About 10% of patients have an EGFR mutation, about 4% have an ALK mutation, and another 1-2% have one of the remaining oncogenic mutations (BRAF, MET, ROS1+, etc.).
Treatment with EGFR tyrosine kinase inhibitors
EGFR mutations are clustered in patients with adenocarcinomas, low or no smokers, women, and Asians. EGFR mutations are rare in smokers. “Therefore, if rapid treatment is clinically indicated, we always start chemotherapy immediately in smokers at St. Gallen without waiting for the result of EGFR testing,” the speaker said. Approximately 70% of patients with EGFR mutation respond to therapy with an EGFR tyrosine kinase inhibitor (TKI), compared with only 1.1% of patients without mutation.
Gefitinib (Iressa®) and erlotinib (Tarceva®) are referred to as first-generation EGFR TKIs; they bind reversibly to the EGFR receptor. Second-generation EGFR TKIs such as afatinib (Giotrif®) and dacomitinib cause irreversible inhibition of the receptors. Therefore, there is hope that they are superior to first-generation EGFR TKIs in their efficacy – corresponding studies are currently underway. Treatment costs are approximately the same for all EGFR TKIs, but the agents differ in side effects.
Prolongation of progression-free survival
In trials to date with EGFR TKIs (gefitinib, erlotinib, afatinib), they significantly prolonged median progression-free survival (PFS) and quality of life compared with treatment with chemotherapy. However, overall survival was not affected due to the high cross-over rate, and over time all patients developed resistance to the EGFR TKI. The addition of bevacizumab to erlotinib in a Japanese study prolonged the median PFS from just under 10 to 16 months, presumably by delaying the development of resistance [1].
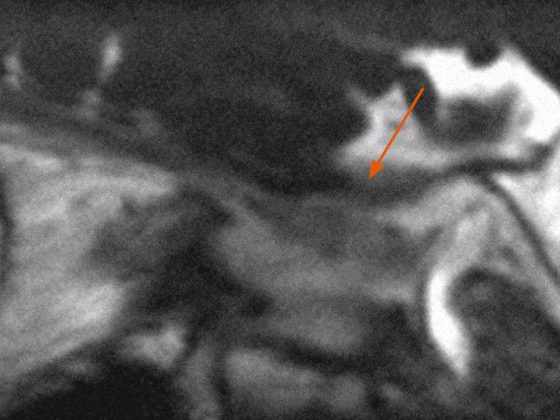
Possible causes of resistance include transformation to small cell carcinoma (in approximately 5%), cancer cell resistance mutations (T790 mutations in 50-60% of cases), or other genetic alterations such as BRAF mutation or MET amplification. “If the EGFR TKI is no longer working, a re-biopsy is recommended so that any alterations can be diagnosed,” Dr. Früh explained. If no alterations are present, patients may be treated with combination chemotherapy (e.g., permetrexed and a platinum). Combination therapy is also more effective than monotherapy in elderly patients and patients with performance status 1 or 2, but is associated with higher toxicity.
How to proceed in case of disease progression?
Can treatment with erlotinib have a benefit beyond disease progression? In the study by Park et al. presented at the 2014 ESMO Congress, continued erlotinib therapy showed a prolongation of PFS2 by about three months [2]. “With disease progression, there is always the question of how threatening it is,” Dr. Früh said. “If there is a threatening systemic progression, treatment must be switched immediately. For local progression, such as brain metastases, local therapy should be given. For nonthreatening systemic progression, I would recommend continuing with EGFR TKI treatment.” Another option would be to switch to another TKI, but good data are still lacking.
BRAF and ALK mutations
A BRAF mutation is present in just under 2% of NSCLC patients, more often in smokers, of which about 50% have a V600E mutation. In various case reports and studies, the agents vemurafenib (Zelboraf®) and dabrafenib (Dafinlar®), which are approved in Switzerland for the treatment of metastatic malignant melanoma, were tested in the indication of advanced NSCLC. These early data indicate some efficacy. Crizotinib (Xalkori®) for the treatment of ALK-positive NSCLC has been on the market since last year. Other ALK inhibitors are being tested in clinical trials.
Inhibitors of the PDL-1 receptor
A new therapeutic approach that can also be used in patients with squamous cell carcinoma is inhibitors of the so-called PD-1 and PDL-1 receptor (“programmed cell death ligand 1”). The compounds most advanced in testing are nivolumab and pembrolizumab (approved as “Keytruda” in the USA). Several studies are currently underway to test such inhibitors in PDL-1 receptor-positive and unselected patients. Immunotherapy with a PDL-1 receptor inhibitor is expected to last one to two years. Initial preliminary results are promising.
Such trial results are not only noticed in the scientific community, as Dr. Früh noted, “We often have inquiries from patients asking about treatment with a PD-1/PDL-1 receptor inhibitor.”
Source: 25th Physician Continuing Education Course in Clinical Oncology, February 19-21, 2015, St. Gallen, Switzerland.
Literature:
- Seto T, et al: Erlotinib alone or with bevacizumab as first-line therapy in patients with advanced non-squamous non-small-cell lung cancer harbouring EGFR mutations (JO25567): an open-label, randomised, multicentre, phase 2 study. Lancet Oncol 2014 Oct; 15(11): 1236-1244.
- Park et al. ASPIRATION: first-line erlotinib until and beyond RECIST progression in Asian patients with EGFR mutation-positiveNSCLC. Ann Oncol 2014; 25 (suppl 4): abstr 12230.
HAUSARZT PRAXIS 2015; 10(3): 51-52