It may sound a bit old-fashioned, but with any medical problem, the classic order applies: history, clinical examination, additional clarifications. Imaging therefore comes in third place if there is already an idea of the pathology. The physician knows to a certain extent what additional information he needs, which consequently enables him to choose the best clarification method. This statement is also valid in sports medicine. But admittedly, with the variety of imaging techniques, the choice is not always easy. What should be used most optimally in sports traumatology? Standard X-ray, MRI, with/without contrast agent, CT scan, ultrasound? Or even SPECT? And if more than one is used, in what order?
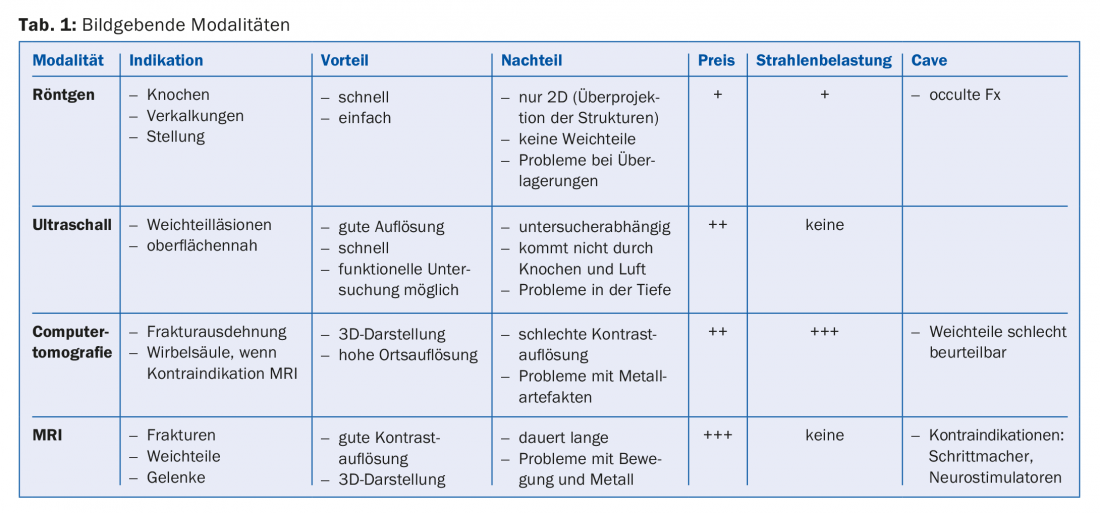
Since the discovery of X-rays and the associated X-ray images by Conrad Röntgen in 1895, a lot has happened in the field of medical imaging and a clean choice of the appropriate technique, first of all independent of one’s own interests, is based on information that is not always easy to find. However, the fact that this choice is very important for various reasons hardly needs to be mentioned. Table 1 attempts to summarize the advantages and disadvantages of the most common imaging modalities.
Scintigraphy for fatigue fractures
Fatigue fractures, which are more common in sports medicine than elsewhere, are still investigated with scintigraphy in a relatively large number of cases. This is a nuclear medicine procedure with intravenous administration of a radioactive substance, electively absorbed from the bone. In the case of increased bone metabolism, as is usually the case in pathological situations, a “hot spot” is formed on the documents created by gamma camera. This examination is relatively time-consuming (20-70 minutes), invasive, and rejected by some patients because of radioactivity. Radiation exposure is slightly higher than with ordinary X-ray, but lower than with CT.
MRI and sonography
In the case of magnetic resonance imaging (MRI), the claustrophobic state that can be triggered during this examination must also be mentioned as a disadvantage. There are alternatives to open systems, but these usually offer a worse resolution than the closed devices.
Sport means movement and movement is the result of muscle work. Thus, this tissue must be damaged more often during physical exertion than in other human activity areas. Sonography is actually a very interesting technique in the search for muscle damage: relatively cheap, without the slightest harmful radiation, repeatable, dynamic, with the possibility of side comparison. And not insignificantly: Sonography can be learned by the practicing physician, which brings great advantages (contact with patients, proof of competence, etc).
SPECT/CT
For the sake of completeness, we must finally mention an imaging technique that holds great promise for joint assessment: SPECT/CT (“single photon emission tomography/computed tomography”). This multimodal technique, which is composed of 3D scintigraphy (SPECT) and conventional CT, is able to provide accurate information on cartilage and bone metabolic changes in a single imaging session. Since these pathological changes can thus be detected very early – in some cases even before clinical symptoms are present – and the early treatment of cartilage damage is thus all the more successful and less invasive, SPECT/CT will certainly become more widespread.
Proceed individually
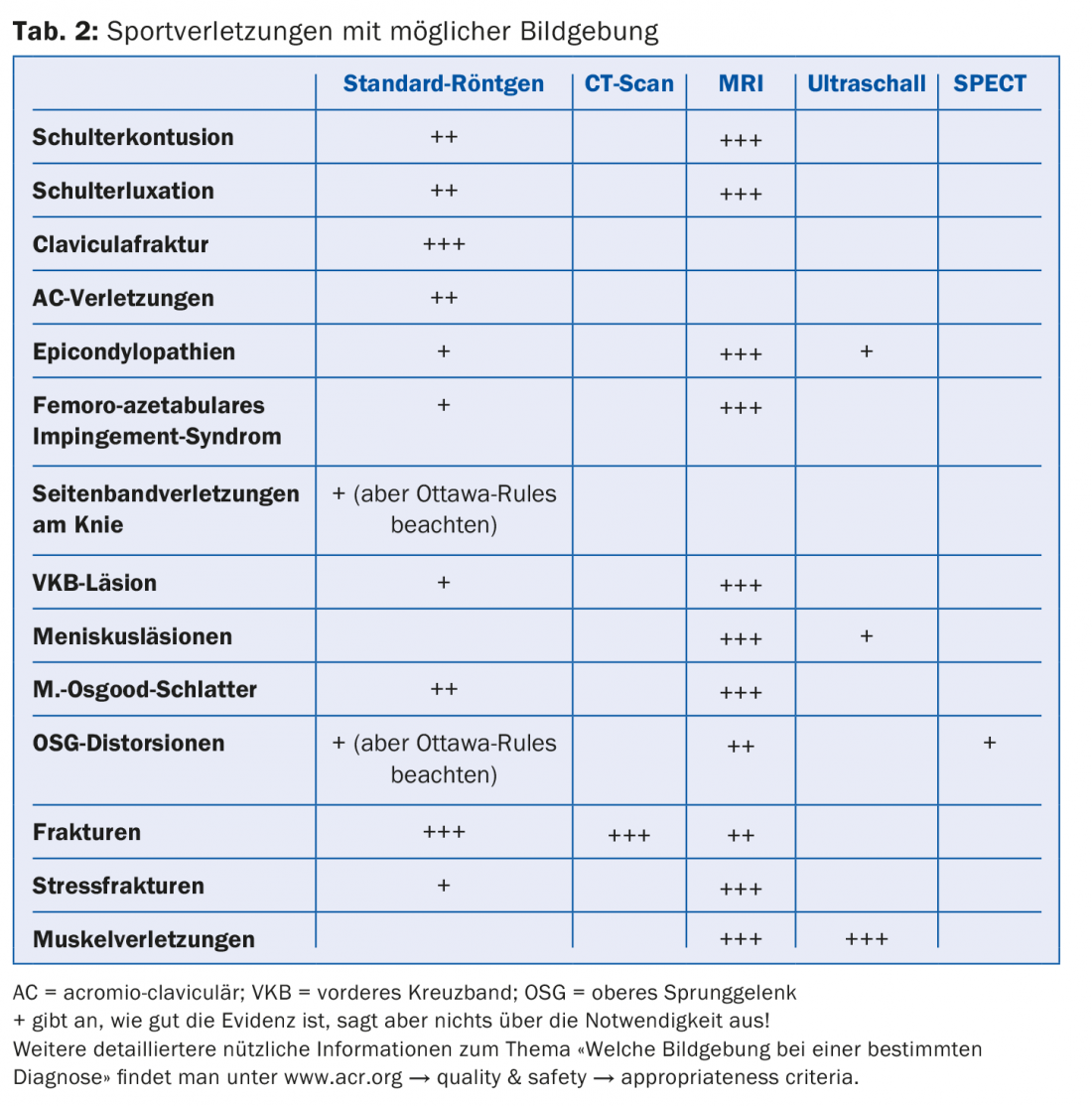
In Table 2, I have listed common sports injuries and indicated the reasonable possible imaging in my experience. However, this classification is to some extent arbitrary, and as almost always in medicine, one should proceed on an individual basis. Every patient is different; for example, a growing adolescent is approached differently than an adult. Trauma plays another role – and since we’re in sports: You don’t necessarily treat a professional the same as a recreational athlete. Furthermore, not every sports injury needs to be confirmed with imaging. The Ottawa rules for the ankle and knee joints remind us that an x-ray is not routine, as it is in certain emergency departments, and should be ordered before the patient is consulted.
Radiation exposure
Finally, a few remarks on the ionizing rays to which mankind is exposed. There are those of natural origin and those of artificial nature. The latter include those produced by medical radiation diagnostics; they account for 98% of this category. In addition, national studies by the FOPH show that the amount is increasing – by as much as 20% between 1998 and 2008, the last period studied. Conventional radiography accounts for 46% of all examinations, dental radiography 42%, and CT 6%. For this, irradiation produced by CT is responsible for 68% of the effective collective dose, while dental X-ray is responsible for only 1%. These comments show very clearly that we physicians play an essential role in the generation of ionizing radiation. A fact we should probably be more aware of!
HAUSARZT PRAXIS 2015; 10(9): 6-7











