Adequate use of inhaled medications in COPD is important. Each patient must find the product that is right for them. This reduces the still frequent errors during inhalation.
“Many patients use inhalatives incorrectly,” said PD Christian Clarenbach, MD, Department of Pneumology, UniversitySpital Zurich. Randomized clinical trials give a deceptive picture in this regard. Here, an immense amount of supervision and precise training is usually required to ensure that the participants inhale correctly. Patients will only be included if they can maintain the appropriate inhalation technique for the duration of the study. Consequently, adherence rates are in the range of 90% or higher, whereas in everyday practice much lower values, namely of about one third or less, are achieved – this is shown by real-world data.
In the clinical setting, many patients do not receive adequate training on proper inhalation technique, resulting in a significant increase in critical errors in inhalant handling. Too often, people still rely on the pharmacist to provide instructions or on the patient to read the package insert carefully himself. Internet links for patient education (handling videos from the manufacturer, etc.) are rarely mentioned in the doctor’s consultation. Nevertheless, an anonymous survey in Switzerland [1] showed that no physician is willing to admit that training in this area could be improved. Nearly 90% reported training with the patient in person at the practice. In most cases, however, regular monitoring did not take place.
“Now, unfortunately, it is the case that inhalatives do not reach their intended site of action in the lungs quite as easily as is possible, for example, with taking tablets for other diseases. To a decisive extent, this is also due to the altered airways in COPD,” the speaker explained. “The physiological conditions make correct application all the more important. This is the only way to ultimately achieve the desired effect.” Important goals of pharmacological COPD therapy are: Symptom improvement, increase in exercise capacity, prevention of exacerbations.
A possible question to initiate the control of the ongoing therapy is: “How are you doing in your daily life with the inhalation and the device?” If the answer is “good”, the patient should still demonstrate the handling once. If the inhalation technique shown is not correct or if the patient has already answered “poorly” to the first question, it is best to show and explain it again followed by a second attempt. Repeat these steps accordingly until the technique is correct. Relatives or even caregivers can be directly involved in the training. Difficulties that continue to exist are documented and – if the procedure was not performed by the physician himself – are now reported to the physician. If the sources of error cannot be eliminated in this way, a change of product should be considered.
Different types of inhalatives
But where to start with training? Regardless of the device, there are known sources of error that must be avoided – this was shown, among other things, by an international cross-sectional study in asthma patients [2]. Overview 1 lists some known errors.

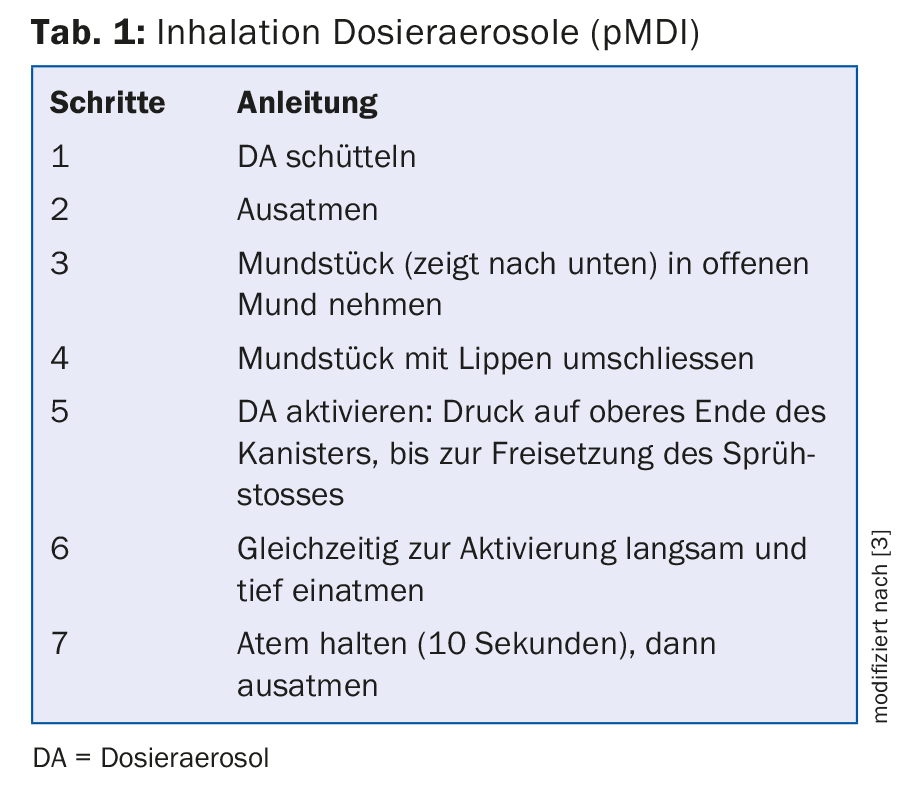
Metered dose inhalation (pMDI): Contains a drug-propellant mixture. Dose released by propellant gas at high velocity. The desired particle size is 1-2 μm. Even a small inhalation flow is sufficient. Come into question for emergency situations. However, they require precise coordination between the initiation of a burst of spray and inhalation. Instructions for use are shown in table 1. Basically: Inhale slowly and deeply, then hold your breath for a few seconds.
Inhalation with metered dose inhaler and priming chamber: This facilitates coordination (aerosol is slowed down after activation and remains in chamber until inhalation). Undesirable deposits of the active ingredient oropharyngeal are reduced. However, the use of these devices is rather cumbersome and requires regular cleaning due to possible bacterial contamination. Basically: Slow and deep inhalation from the spacer (advance chamber) over several breaths.
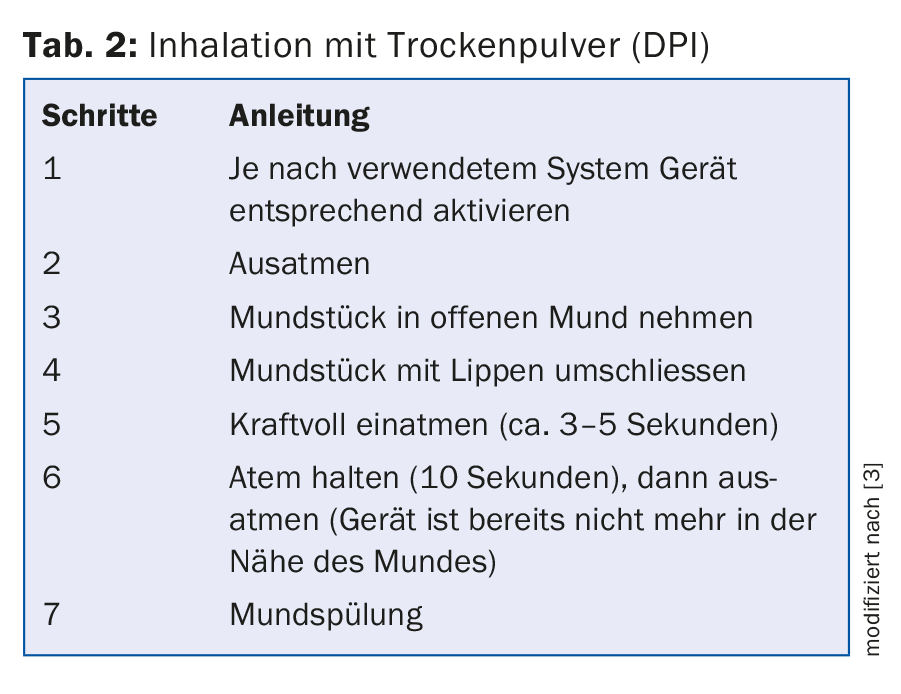
Dry powder inhalation (DPI): Examples are Diskus®, HandiHaler®, Breezhaler®, Turbuhaler® or Genuair®. Coordination is no longer a problem here, and handling is comparatively simple. In some cases, direct inhalation control is possible (e.g. via transparent capsule). However, a higher inhalation flow is required and even a small exhalation into the system can lead to clumping. Instructions for use are shown in table 2. Basically: Inhale quickly and deeply, then hold your breath.
Double jet inhaler (“soft mist inhaler”): “hermaphrodite” of nebulizer and metered dose inhaler . Is currently the only liquid nebulizer without external electrical power. Particularly suitable for patients with severe airway constriction and coordination problems, as the fine spray cloud spreads more slowly and remains in the room longer than with a propellant-operated metered dose inhaler.
Moist inhalation/nebulizer: Requires no coordination, can also be used in homes, hospitals and during exacerbations. Different active ingredients can be combined. Overall, larger quantities of aerosol can be produced. However, the therapy lasts five to ten minutes. The lung secretion is partially liquefied and can be coughed up more easily. As a general rule, inhale slowly and deeply.
Considerations before giving a holder
To select an appropriate inhalant, one should first assess the patient himself: Is he able to coordinate? How much inspirational power does he bring to the table? What is his preference, how adherent is he? In this context, of course, age and comorbidities also play a role.
In addition, there are disease factors. Severe obstruction may reduce adequate inhalation flow. In addition, COPD requires a different therapeutic strategy than asthma.
Caregivers are also part of a holistic treatment approach. It is worth involving relatives or partners in the training, especially in the case of older people, according to the principle “four eyes see more than two”. In addition, the primary care physician should be informed about the inhaler used and the appropriate inhalation profile, as should the pharmacist and caregivers.
All manufacturers also offer training and information materials as well as placebo devices for practice.
Source: COPD Day, November 11, 2017, Zurich
Literature:
- Clarenbach CF, Nicod LP, Kohler M: Real-world asthma management with inhaler devices in Switzerland-results of the asthma survey. J Thorac Dis 2016 Nov; 8(11): 3096-3104.
- Westerik JA, et al: Characteristics of patients making serious inhaler errors with a dry powder inhaler and association with asthma-related events in a primary care setting. J Asthma 2016; 53(3): 321-329.
- Rothe T: Inhalation therapy – Part 2: Inhalation technique and active substances. Switzerland Med Forum 2014; 14(21): 426-430.
HAUSARZT PRAXIS 2017; 12(12): 33-35