Across Europe, there has been a significant increase in sexually transmitted diseases such as syphilis, chlamydia and gonorrhea in recent years. A clear diagnosis is clinically relevant, as the dose and duration of antibiotic treatment differ between different sexually transmitted diseases and stages of the disease. For example, low doses of penicillin can temporarily reduce the syphilis pathogens, but have an inadequate effect, particularly if the central nervous system is affected.
“Syphilis infections have risen sharply,” says Dr. Susanne Buder, Head of the Clinic for Dermatology and Venereology at Neukölln Hospital, Berlin [1]. Between 2010 and 2019, the number of syphilis cases among 15 to 49-year-olds in Europe rose by 87% and the number of cases of chlamydia and gonorrhea also increased dramatically [2]. The Robert Koch Institute (RKI) reported a new high in syphilis incidence in Germany in 2022 [3]. At 10.0 cases per 100,000 inhabitants nationwide, the incidence was above the median of 8.9 in the five previous years. The median age for women was 35 years (range 0-85) and for men 40 years (range 0-86). The speaker reported that a striking number of people in the 30-39 age group were affected [1]. Epidemiological data shows that the incidence is particularly high in large cities. In Berlin, this figure is currently 40 per 100,000 inhabitants. In Switzerland, too, the number of cases has been rising continuously since the pandemic-related low in 2020. In 2022, the incidence in Germany was 9.3 cases per 100,000 people in the resident population [4]. Syphilis (Lues) only occurs in humans and is transmitted sexually, through blood and intrauterine from mother to child [3]. The majority of those affected by syphilis are men who have sex with men (MSM) and female sex workers.
Serological IgM and IgG-Ak detection provides clarity
The cause is an infection caused by the spirochete species Treponema pallidum (Fig. 1) . “There are various differential diagnoses that need to be considered,” emphasized Dr. Buder [1]. The staging of syphilis is an important aspect of the diagnosis [3]:
- Primary stage: a mostly painless ulcer forms at the entry site a few days to weeks after infection
- Secondary stage: general symptoms and skin symptoms noticeable
- Tertiary stage (years after the initial infection): Damage to the central nervous system and blood vessels
In the first stage, the clinical picture is relatively clear and can be confirmed by syphilis serology, but not all patients consult a doctor because of the non-painful ulcerations, explained Dr. Buder [1]. The ulcerations typically occur in the genital area, but can also occur in the lip area or on the sputum of infected patients, depending on the entry point of the pathogen, and disappear again after around three weeks, even without treatment. However, the disease progresses in the meantime and, as described above, can be accompanied by various clinical manifestations, some of which are non-specific.
It therefore becomes more difficult if progression to the second stage has occurred, which is usually accompanied by general symptoms such as fever and malaise. Organ involvement such as hepatitis is also possible, Dr. Buder reported [1]. The cutaneous manifestations are multiple skin and mucous membrane lesions that are not very specific and can also be interpreted as exanthema or early HIV infection, the speaker pointed out [1].
If a diagnosis of syphilis is suspected on the basis of the clinical images, appropriate testing should be carried out, the expert recommends [1]. A PCR test (swab of an ulceration) is available for the primary stage. The second option is serology, which must be performed within a certain diagnostic window, as it is an antibody detection. “It takes on average 2-4 weeks until we see seroconversion,” explained Dr. Buder [1]. While IgM antibodies(Ak) fall relatively quickly, IgG-Ak remain even after treatment (so-called seronarcosis). Unfortunately, the production of the previously used Treponema pallidum agglutination test (TPPA) was discontinued in the fall of 2022, the speaker said [1]. This is a shame, as it was a very valid and reliable test. Individual laboratories still have remaining stocks, but in general it has since been necessary to switch to alternative Ak detection (box) [1,5].
| Syphilis serology: Laboratory diagnostic work-up |
| First, polyvalent immunoglobulin (Ig)G and Ig-M tests such as chemiluminescence tests (CMIA, CLIA) and an enzyme-linked immunosorbent assay (ELISA, EIA) are performed for confirmation. In order to determine the sensitivity of a particular test, the speaker recommends testing “in-house” against confirmed syphilis samples and always sending the samples to the same reference laboratory. |
| In order to determine the disease activity and the need for treatment, IgG and IgM tests are subsequently carried out in the case of positive test results using a Veneral Disease Research Laboratory test (VDRL test) or a Cardiolipin Microflocculation Test (CMT) or a Rapid Plasma Reagin test (RPR). If the test results are unclear, a Western blot is also performed. |
| to [1,5] |
DD for genital, perianal and oral ulcers
The question of how to proceed with patients who have genital ulcers but a negative syphilis serology is a recurring issue in everyday clinical practice. The speaker recommends repeating syphilis serology several times and carrying out differential diagnostic investigations in parallel [1]. The main differential diagnoses are:
- Herpes simplex I/II: “Herpes simplex is a classic differential diagnosis in the case of a genital ulcer and negative syphilis serology,” said Dr. Buder, illustrating this with a case study of a patient with chronic lymphocytic leukemia [1].
- Mpox: Since spring 2020, Mpox (“monkeypox”) has also been a classic differential diagnosis. Patients present with genital or oral skin lesions and suffer from fever, headache and lymphadenopathy. The cutaneous manifestations are single or multiple skin lesions, some of which are pustular. Several perianal ulcers often manifest themselves. The speaker reported that they had Mpox cases in Berlin until January 2023, then not for a few months and regularly again since September 2023 [1]. In Germany as a whole, Mpox cases have been reported in 12 out of 16 federal states since this period.
- Lymphogranuloma verum: This is another DD that should be considered [1]. This is a sexually transmitted disease caused by the bacterium Chlamydia trachomatis, which has been spreading in Europe and North America for around 20 years. Genital ulcers are rather rare, but do occur. These patients also show swelling of the lymph nodes.
- Chancroid (ulcus molle): This is a rare DD, it is a venereal disease caused by infection with the bacterium Haemophilus ducreyi [1]. Those affected initially show non-painful lesions, which develop into painful ulceration as the disease progresses.
- Donovanosis: This DD, also known as “granuloma inguinale”, is also rare [1]. Patients often show many granulomatous changes. For the purpose of DD, it is important to look specifically for the pathogen (Klebsiella granulomatis).
- Lipschütz ulcer: The last DD mentioned by the speaker is ulcus vulvae acutum, which is also known as Lipschütz ulcer. This is an extremely rare form of genital ulcer. The majority of those affected are young women, who usually suffer from accompanying symptoms such as fever and lymphadenopathy and have rheumatoid arthritis or an EBV infection [1].
Treating syphilis with stadium-adapted antibiotics
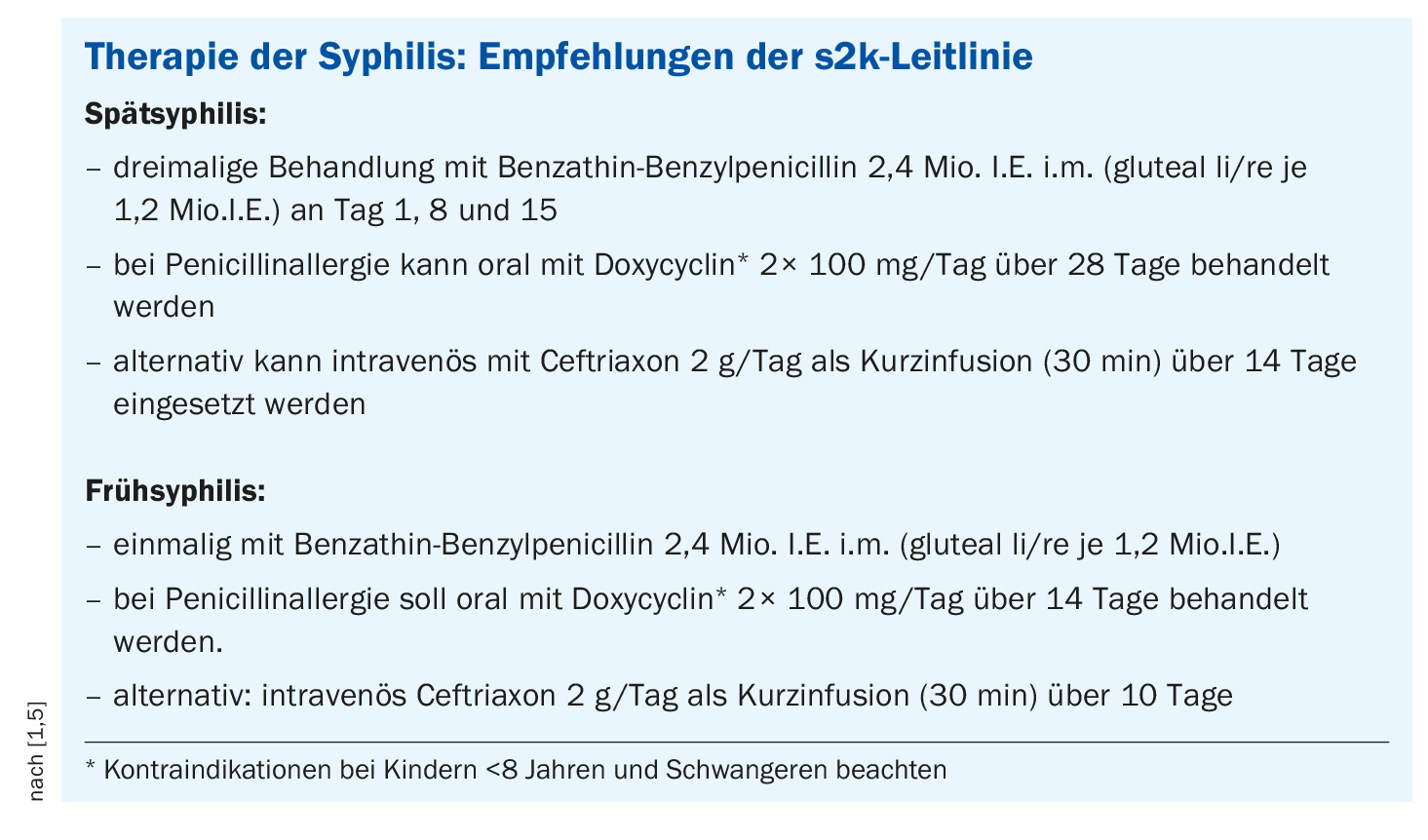
The German s2k guideline for the treatment of syphilis is regularly updated [5]. Penicillin has been the treatment of choice for many decades. “We provide stage-adapted therapy,” says Dr. Buder [1]. Benzathine benzylpenicillin can be used in all stages, but at different frequencies (box). In a late stage, three treatments at one-week intervals are recommended; in an early stage, a single treatment is sufficient. To prevent a drug reaction to penicillin, steroids can be administered 30 minutes before the start of treatment [1]. Immunocompromised persons with syphilis can also be treated with standard antibiotics, but immunocompression can lead to simultaneous primary and secondary inflammation and the neurological and psychiatric symptoms associated with the tertiary stage occur more frequently. Headaches, ophthalmologic and otologic symptoms are also included. If this is suspected, a lumbar puncture is recommended. If neuro-syphilis is confirmed, intravenous antibiotics are administered over a longer period of time. “Patients with a penicillin allergy are difficult,” Dr. Buder admitted [1]. The broad-spectrum antibiotic ceftriaxone can be used as an alternative to penicillin. The guideline also mentions doxycycline (box) . For the monitoring of treated syphilis patients, the first serology check is recommended four weeks after successful treatment, after which the interval can be extended to three months. “Always try to determine the titres in the same laboratory,” Dr. Buder emphasized again in conclusion [1].
Congress: Swiss Derma Day and STI reviews and updates
Literature:
- «Syphilis: Practical diagnosis and pitfalls», Dr. med. Susanne Buder, Swiss Derma Day and STI reviews and updates, 11.01.2024.
- «Rekordhoch bei sexuell übertragbaren Erkrankungen in Europa», www.meduniwien.ac.at/web/ueber-uns/news/2023/news-im-oktober-2023/rekordhoch-bei-sexuell-uebertragbaren-erkrankungen-in-europa, (letzter Abruf 10.04.2024).
- Robert Koch Institut, Epidemiologisches Bulletin 7/24, 15.02.2024, www.rki.de/DE, (letzter Abruf 10.04.2024).
- Bundesamt für Gesundheit: BAG-Bulletin 48/2023, Ausgabe vom 27.11.2023.
- “S2k guideline on the diagnosis and treatment of syphilis”, 2020, register number 059 – 002, https://register.awmf.org,(last accessed 10.04.2024).
HAUSARZT PRAXIS 2024: 19(4): 45–46 (veröffentlicht am 18.4.24, ahead of print)
DERMATOLOGY PRACTICE 2024; 34(2): 34-35