The development of highly effective biologics was preceded by research efforts over several decades. Advances in immunopathogenetic and molecular genetic analyses contributed significantly to the generation of these innovative system therapeutics. The Guenter Goerz Memorial Lecture of this year’s annual meeting of the Working Group for Dermatological Research was dedicated to this topic and spanned from milestones of psoriasis research to the biologics available today.
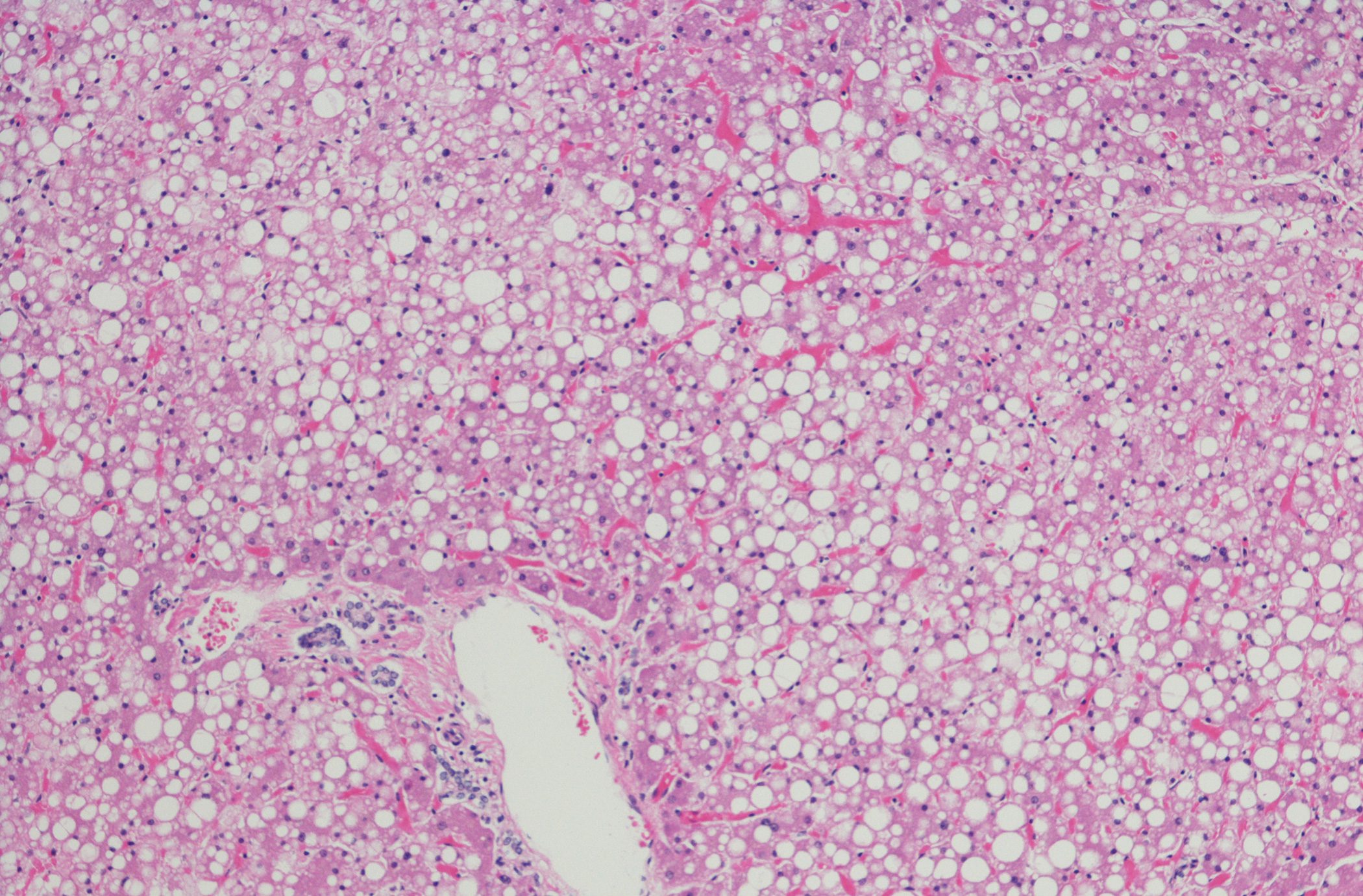
Clinical and experimental evidence led to the recognition that psoriasis is a genetically predisposed immune-mediated inflammatory skin disease (Fig. 1). That T cells play a role in the pathogenesis of psoriasis has become increasingly clear over the years, explained Prof. Wolf-Henning Boehncke, MD, Chief of the Department of Dermatology, Hôpitaux Universitaires de Genève [1]. The successful treatment of psoriasis patients with ciclosporin, an immunosuppressant that inhibits T cell proliferation and cytokine production, was the first clinical evidence for a possible role of T cells in the pathogenesis of psoriasis [2,3]. Other T cell-targeting drugs such as anti-CD4 monoclonal antibodies and cytotoxic T lymphocyte-associated antigen 4 (CTLA4) also showed significant therapeutic efficacy in the treatment of psoriasis [4–6]. A previous in vitro study indicated that activated CD4+ T cells from psoriatic lesions can enhance keratinocyte proliferation via secretion of interferon-γ(IFN-γ)8 , and the establishment of a xenogeneic transplantation model in mice further confirm the importance of T cells in psoriasis [4–6].
Discovery of psoriasis-relevant autoantigens
The finding that psoriasis is a T cell-mediated autoimmune disease raises the important question of how pathogenic T cells are activated during the course of the disease. For some time, the antimicrobial peptide LL37, which is overexpressed in psoriatic skin, was thought to play a role in this process. However, researchers only succeeded in providing empirical evidence a few years ago. In a 2014 paper in Nature Communication Lande et al. reported that chronic overexpression of LL37 causes persistent nucleic acid-mediated activation of these receptors, resulting in maturation of dendritic cells (DCs) [7]. Since then, in addition to LL-37, three other psoriasis-relevant autoantigens have been discovered, namely cathelicidin, ADAMTSL5, PLA2G4D, and keratin-17. In numerous patients with moderate to severe plaque psoriasis, autoreactive T cells against these autoantigens were detected [8].
| “Tissue-resident memory T cells. Currently, one focus of psoriasis research is on tissue-resident memory CD8+ T cells ( TRMs). This is a specific population of memory T cells in the epidermis and dermis that maintain an immunological memory over years and contribute to the typical lesions [25]. Even in skin areas that have never been affected by lesions, psoriasis patients have higher numbers of TRM cells than healthy individuals [25]. One hypothesis, which is the subject of current empirical studies, refers to the fact that by reducing the accumulation of TRM cells in the skin, the long-term course of psoriasis disease can be positively influenced [27]. |
T lymphocytes as a trigger of psoriatic disease
The important role of T lymphocytes has been demonstrated in a xenogeneic transplantation model [9,10]. The observation that skingrafts of non-lesional skin from psoriasis patients in immunodeficient mice resulted in spontaneous development of the lesional skin phenotype was taken as evidence for the presence of tissue-resident memory T cells (TRM) [11]. In addition to anti-CD4 antibodies and T-lymphocyte-associated antigen-4 immunoglobulin, two agents that inhibit T-cell functions, efalizumab and alefacept, have been developed [2]. Efalizumab is a humanized monoclonal antibody that binds to the CD11a subunit of LFA-1 (lymphocyte function-associated antigen-1), which is located on the surface of lymphocytes. Efalizumab was approved in Switzerland and the EU in 2004. However, the biologic has been off the market for several years due to a warning issued by the FDA regarding infection risks such as bacterial sepsis, viral meningitis, invasive fungal disease, and progressive multifolacial leukoencephalopathy [2]. Alefacept is a recombinant fusion protein consisting of parts of the signaling molecule LFA3 from antigen-presenting cells and the antibody IgG1 [2]. Alefacept prevents LFA3 from binding to activated memory T cells involved in the development of psoriasis. Alefacept was approved in the USA in 2003, but has not been marketed since 2011. To date, the biologic has not received marketing authorization in the EU.
Pathophysiological significance of the IL-23/Th17 axis.
That the interleukin (IL)-23/T helper cell (Th)17 axis plays an important role in the pathophysiology of psoriasis and psoriatic arthritis is a major finding [14]. But initially, psoriasis was thought to involve a Th1 response driven by the cytokines IFNγ and IL-12 [15]. However, this was contradicted by the lack of efficacy of anti-IFNγ therapies for the treatment of psoriasis [16]. When increased expression of p40 was discovered in psoriatic lesions, this led to the initial conclusion that IL-12 expression is increased in psoriasis [17]. However, when it was later shown that the p40 subunit of IL-12 is also found in IL-23 [18], Dr. Lee and colleagues demonstrated that the increased expression of p40 in psoriatic skin was due to IL-23 and not IL-12 [17,19]. Since IL-23 is involved in the Th17 axis, while IL-12 drives the development of Th1 cells, the IL-23/Th17 immune axis was then considered central to the pathogenesis of psoriasis [18,20]. Concomitantly, IL-23, tumor necrosis factor (TNF)-α, and IL-17 have been identified as pathogenetically significant cytokines in psoriasis. IL-23 has a regulatory effect on the maintenance of Th17 cells, whereas IL-17 and TNF-α mediate effector functions of innate and adaptive immune cells.
| Predisposition: Molecular genetics sheds light on the subject Psoriasis is a multifactorial disease, and genetic determination appears to play an important role. Genome-wide association studies identified 36 susceptibility loci [12,13]. The PSORS1 locus in the histocompatibility region on chromosome 6p21 appears to be of particular importance. There lies the allele HLA-Cw*0602, which has the strongest association with psoriasis. Through advances in molecular genetic technologies and statistical analysis methods, psoriasis-relevant biological pathways were encountered, for example, regarding the epidermal barrier, NFκB-associated mechanisms, and Th17-mediated immune responses [2]. |
Highly effective biologics – a modern achievement
The first generation of biologics for the treatment of psoriasis that targeted cytokines focused on TNF-α [21]. However, TNF-α inhibitors are known risk factors for serious lower respiratory tract infections or skin and soft tissue infections. Ustekinumab, another interleukin inhibitor, was launched in 2009 (EU) and 2010 (CH). Ustekinumab targets the common protein subunit p40 of IL-12 and IL-23 and blocks signal transduction of their corresponding receptors. In the ACCEPT study published in 2010, ustekinumab was shown to be superior to the TNF-α inhibitor etanercept. PASI75 and PASI90 response rates at week 12 were 73% and 44%, respectively, with ustekinumab, compared with 56% and 23%, respectively, of patients treated with etanercept. [29]. In contrast, in studies comparing ustekinumab with the IL-17 inhibitors secukinumab, brodalumab, and ixekizumab, the IL-12/23 inhibitor showed significantly lower therapeutic efficacy. [21]. The approval of the IL-17 inhibitors was followed by that of the IL-23 inhibitors guselkumab, risankizumab, and tildrakizumab. In the CLEAR study published in 2017, secukinumab was subjected to a head-to-head comparison with ustekinumab [22]. In a sample of 676 randomized subjects, the IL-17A inhibitor proved significantly superior to ustekinumab at week 52 with respect to PASI-90 response rates (76% vs. 61%) as well as IGA 0/1** (80% vs. 65%) (both p<0.0001). A head-to-head trial of secukinumab (n=514) vs guselkumab (n=534) was the ECLIPSE study published in 2019 [23]. On treatment with the IL23p19 inhibitor, a significantly higher proportion achieved a PASI90 response at week 48 compared to secukinumab (84% vs. 70%; p<0.0001). In studies with indirect comparisons between tildrakizumab and guselkumab, neither agent proved superior or inferior [30]. Also in 2021, a head-to-head comparison between bimekizumab (n=373) and secukinumab (n=370) was published [24]. Here, bimekizumab (dual inhibition of IL17A and IL17F) proved neither superior nor inferior to secukinumab (anti-IL17A).
** IGA= Investigator’s Global Assessment (0=appearance-free, 1=almost appearance-free).
Congress: ADF Annual Meeting
Literature:
- “Psoriasis – mirror image trends in cutaneous biology,” Guenter Goerz Memorial Lecture, Prof. W.-H. Boehncke, MD, 49th ADF Annual Meeting, Innsbruck, Feb. 22-25, 2023.
- Cai Y, Fleming C, Yan J: New insights of T cells in the pathogenesis of psoriasis. Cell Mol Immunol 2012; 9(4): 302-309.
- Mueller W, Herrmann B: Cyclosporin A for psoriasis. N Engl J Med 1979; 301: 555.
- Nicolas JF, et al: CD4 antibody treatment of severe psoriasis. Lancet 1991; 338: 321.
- Prinz J, et al: Chimaeric CD4 monoclonal antibody in treatment of generalised pustular psoriasis. Lancet 1991; 338: 320-321.
- Abrams JR, et al: Blockade of T lymphocyte costimulation with cytotoxic T lymphocyte-associated antigen 4-immunoglobulin (CTLA4Ig) reverses the cellular pathology of psoriatic plaques, including the activation of keratinocytes, dendritic cells, and endothelial cells. J Exp Med 2000; 192: 681-694.
- Lande R, et al: The antimicrobial peptide LL37 is a T-cell autoantigen in psoriasis. Nat Commun 2014; 5: 5621.
- Ten Bergen LL, et al: Current knowledge on autoantigens and autoantibodies in psoriasis. Scand J Immunol 2020; 92(4): e12945.
- Boehncke WH, et al: Pulling the trigger on psoriasis. Nature 1996; 379: 777.
- Boehncke WH, Brembilla NC: Autoreactive T lymphocytes in inflammatory skin dis-eases. Front Immunol 2019; 10: 1198.
- Boyman O, et al: Spontaneous development of psoriasis in a new animal model shows an essential role for resident T cells and tumor necrosis factor-alpha. J Exp Med 2004; 199: 731-736.
- Clop A, et al: An in-depth characterization of the major psoriasis susceptibility locus identifies candidate susceptibility alleles within an HLA-C enhancer element. PLoS One 2013; 8(8): e71690.
- Capon F, et al: Psoriasis and other complex trait derma-toses: from loci to functional pathways. J Invest Dermatol 2012; 132(3 Pt 2): 915-922.
- Girolomoni G, et al: The role of IL-23 and the IL-23/TH 17 immune axis in the pathogenesis and treatment of psoriasis. J Eur Acad Dermatol Venereol 2017; 31(10): 1616-1626.
- Schlaak JF, et al: T cells involved in psoriasis vulgaris belong to the Th1 subset. J Invest Dermatol 1994; 102: 145-149.
- Harden JL, et al: Humanized anti-IFN-gamma (HuZAF) in the treatment of psoriasis. J Allergy Clin Immunol 2015; 135: 553-556.
- Yawalkar N, et al: Expression of interleukin-12 is increased in psoriatic skin. J Invest Dermatol 1998; 111: 1053-1057.
- Oppmann B, et al: Novel p19 protein engages IL-12p40 to form a cytokine, IL-23, with biological activities similar as well as distinct from IL-12. Immunity 2000; 13: 715- 725.
- Lee E, et al: Increased expression of interleukin 23 p19 and p40 in lesional skin of patients with psoriasis vulgaris. J Exp Med 2004; 199: 125-130.
- Aggarwal S, et al: Interleukin-23 promotes a distinct CD4 T cell activation state characterized by the production of interleukin-17. J Biol Chem 2003; 278: 1910- 1914.
- Ten Bergen LL, et al: The TNF/IL-23/IL-17 axis-Head-to-head trials comparing different biologics in psoriasis treatment. Scand J Immunol 2020 Oct; 92(4): e12946.
- Blauvelt A, et al: Secukinumab is superior to ustekinumab in clearing skin of subjects with moderate-to-severe plaque psoriasis up to 1 year: results from the CLEAR study. J Am Acad Dermatol 2017; 76(1): 60-69.e9.
- Reich K, et al: Guselkumab versus secukinumab for the treatment of moderate-to-severe psoriasis (ECLIPSE): results from a phase 3, randomised controlled trial. Lancet 2019; 394(10201): 831-839.
- Reich K, et al: Bimekizumab versus secukinumab in plaque psoriasis. N Engl J Med 2021; 385(2): 142-152.
- Clark RA: Resident memory T cells in human health and disease. Sci Transl Med 2015; 7(269): 269rv1
- Gallais Sérézal I, et al: A skewed pool of resident T cells triggers psoriasis-associated tissue responses in never-lesional skin from patients with psoriasis. J Allergy Clin Immunol 2019; 143: 1444-1454.
- Eyerich K, et al: IL-23 blockade with guselkumab potentially modifies psoriasis pathogenesis: rationale and study protocol of a phase 3b, randomised, double-blind, multicentre study in participants with moderate-to-severe plaque-type psoriasis (GUIDE). BMJ Open 2021; 11(9):e049822
- Hu P, et al: The Role of Helper T Cells in Psoriasis. Front Immunol 2021 Dec 15; 12: 788940. https://www.frontiersin.org/articles/10.3389/fimmu.2021.788940/full,(last accessed 17.05.2023).
- Griffiths CE, et al: ACCEPT Study Group. N Engl J Med 2010; 362(2): 118-128.
- Ghazawi FM, et al: Front Med (Lausanne) 2021; Aug 10; 8:702776. fmed.2021.702776.
DERMATOLOGIE PRAXIS 2023; 33(3): 14-15 (published 8.6.23, ahead of print).