In every occupation and leisure activity, one is exposed to possible allergen sources. The story shows with a concrete example how manifold allergies can be even in an absolutely quiet activity like fishing and how important it is to survey the whole environment and possible exposures.
Family man Biner (name chosen purely by chance) was under quite a bit of pressure as an IT specialist and therefore decided on a hobby that would really “de-stress” him: Fishing. He spent a small fortune on it. He bought a rowboat, high boots, a fishing rod, crushed pumpkin seeds for bait, suitable clothing, books, a freezer, a net, accessories – just everything that goes with it. And soon he was in action.
So far, he had not been an allergy sufferer (except for a mild hay fever in May and June to grasses). Soon, however, he noticed that when he fished, his eyes began to water, so he refrained from fishing during those months. After a few months, by now it was September and no longer pollen season, sneezing plagued him shortly after casting his fishing line and he had trouble exhaling. What had happened? He noticed that he developed discomfort whenever he scattered ground-up pumpkin seeds, but not when he used only pieces of meat as bait. In addition, he had also developed oral allergy syndrome when eating zucchini and even penile edema the last time. “That must be it,” he thought. So no more pumpkin seed meal, just chunks of meat.

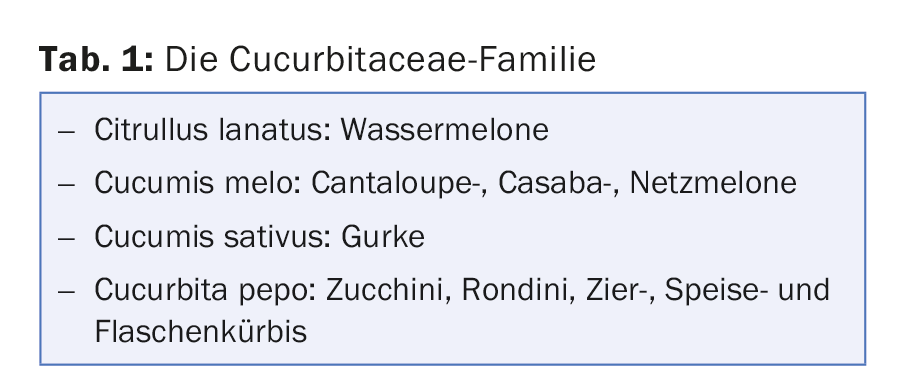
Note: Fish bait, animal feed and the like should not be scattered against the wind. Inhalation sensitization occurs much more easily than, for example, ingestion and even more easily than immediate-type sensitization through the skin (repetitive contacts through pre-damaged skin). This is a primary sensitization to pumpkin in an atopic patient and a cross-reaction to taxonomically related foods (Fig. 1). Theoretically, allergy to cucumbers and watermelons would also be possible (Tab. 1).
Two weeks later, the fisherman on the boat was attacked by a bee and stung in the hand, the first sting since childhood (at that time it had been a hornet’s nest). Within 20 minutes he was itching all over his integument, wheals were shooting up everywhere and he was struggling with severe nausea. He did not move, called for help across the water and could be brought ashore. “Now I need an allergist,” he realized. The allergist had an appointment available in four weeks, just in time to do serological testing. These revealed monosensitization to the recombinant and relevant allergen of wasp ves v1 3.7kU/l and ves v5 8.5 kU/l and were negative for bee (api m1 <0.35 kU/l). His allergist said, “Mr. Biner, you have not been stung by a bee, but by a wasp. In the future, you must carry this emergency kit with you at all times.” He gave him emergency tablets and an epinephrine auto-injector and instructed him on how it worked.
In fact, three weeks later, Mr. Biner was stung again by a wasp, this time causing a reaction within 10 minutes with nausea, urticaria and respiratory distress. Immediately after the sting, he took the pills – as soon as shortness of breath occurred, he used the syringe and had his breath back in a few seconds. Without haste, he went back to shore and spent a comfortable evening, until in the middle of the night it came again to asthma and consecutively to an emergency visit to the hospital and monitoring until the next afternoon.
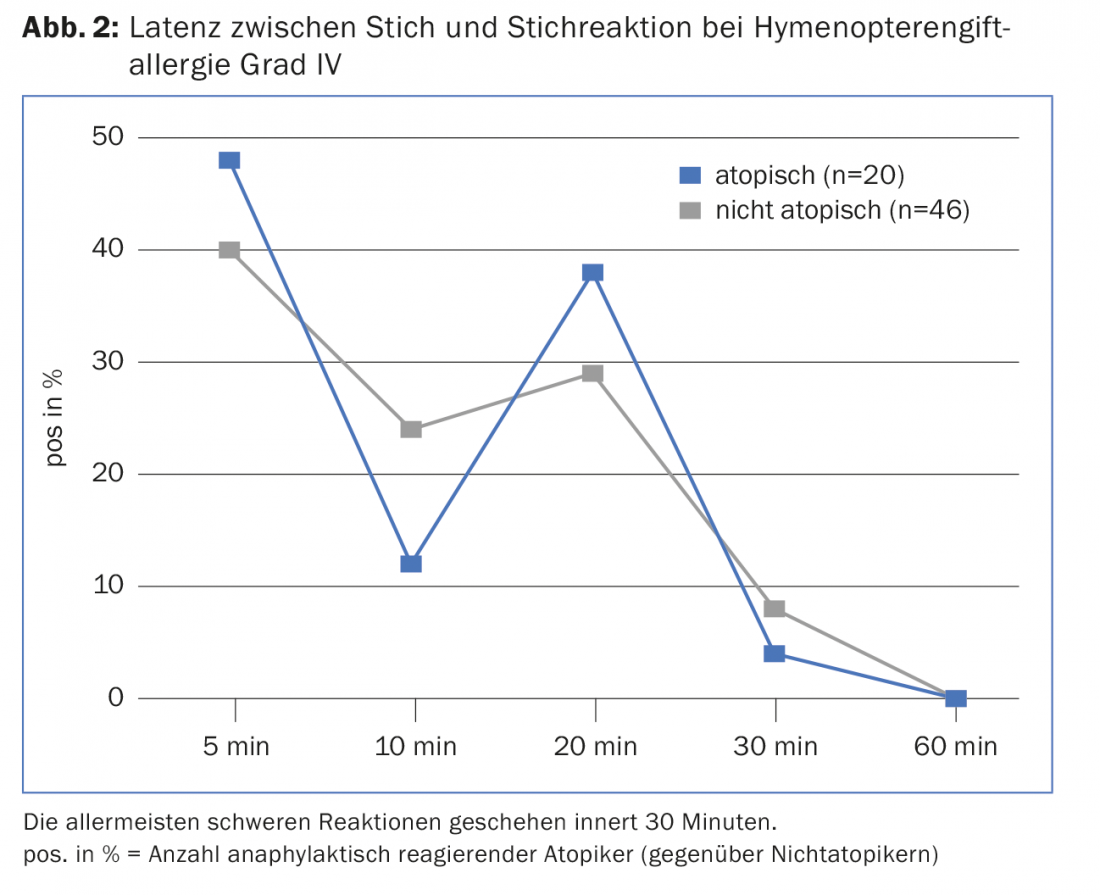
Note: The wasps had been attracted by the meat, which was now used as bait. Typically, wasps sting in the second half of the year, they do not leave a stinger. Crescendo symptomatology is typical, occurring in 80% of hymenopteran venom allergy sufferers if they are stung again within two years. Moreover, the anaphylaxis always occurs within less than 30 minutes (Fig. 2), which means that the emergency tablets are not yet effective. The effect of cetirizine and levocetirizine occurs only after 25 minutes, that of cortisone only after six hours.
Adrenaline is a lifesaver and should therefore be applied immediately in the event of any systemic reaction. Not as uncommon is the biphasic reaction in severe allergic patients, which can occur 20 minutes to 48 hours after the first application of epinephrine. In such patients, especially those without desensitization and with a high risk of being stung away from civilization, the carrying of two auto-injectors should be considered.
The level of specific IgE to wasp venom does not indicate allergy risk. Particularly in atopics, very high values are often measured, even in some cases with allergy grade I, i.e. with only excessive local swelling. On the other hand, in case of risk of exposure in case of allergy grade II n. H.L. Müller, but at the latest after severe biphasic anaphylaxis. The indication for desensitization to bee/wasp venom is shown in Table 2. Sensitization occurred via hornet stings in youth, whose venom is related to wasp venom.
Mr. Biner opted for Ultrarush desensitization under monitoring in the hospital for five hours. This was followed by monthly maintenance therapy with the primary care physician. Everything went without problems. Immediately after the Ultrarush initiation, he was protected from reactions and therefore went back on the boat. But when winter came and the cool wind blew in his face, he noticed redness and swelling on his face and generalized itching. Even the tablets for hay fever, which he took once or twice a day, did not help. He again saw the allergist, who did some blood tests and diagnosed cold urticaria. Mr. Biner was new to take four antihistamines per day. He already had an emergency kit.
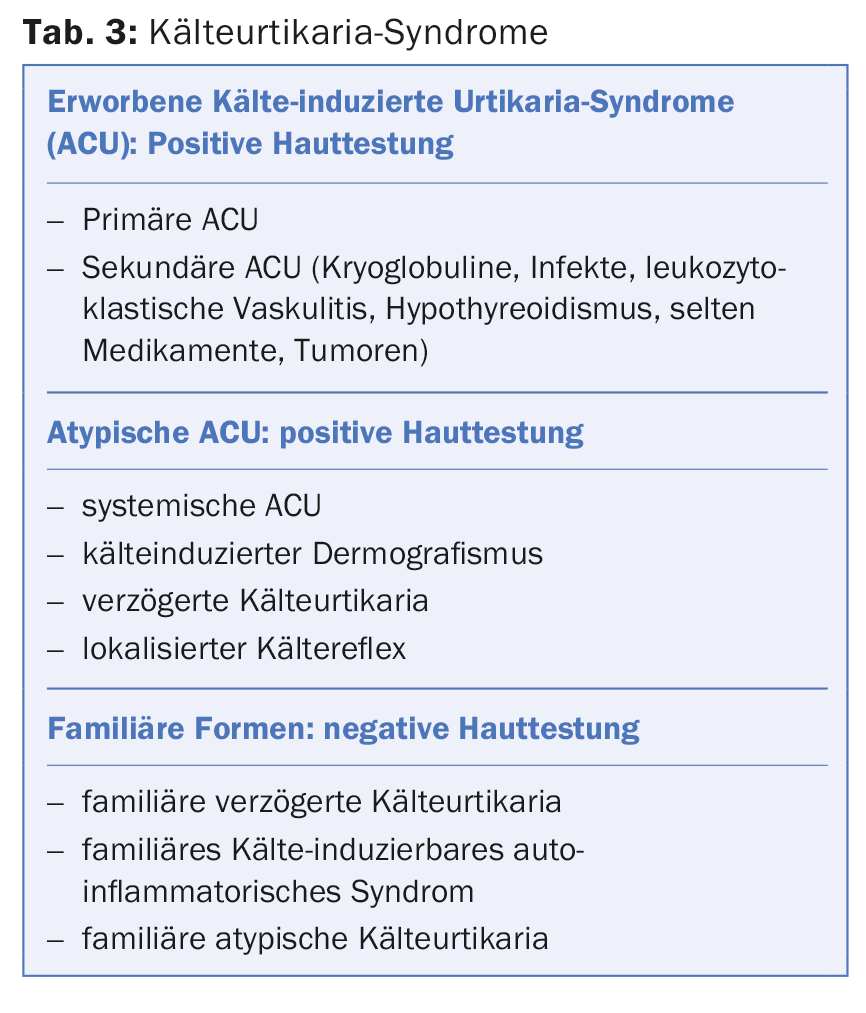
Note: Cold urticaria is a form of physical urticaria, although it can result in anaphylactic shock with appropriate exposure. In most cases, patients can specify exactly at which temperature the complaints begin. Wind increases the feeling of cold. In most cases, cold urticaria is idiopathic and lasts an average of four years. Rarely, one of the associations listed in Table 3 is found. Mastocytosis should be excluded serologically. There are cases of familial cold urticaria with wasp venom allergy.
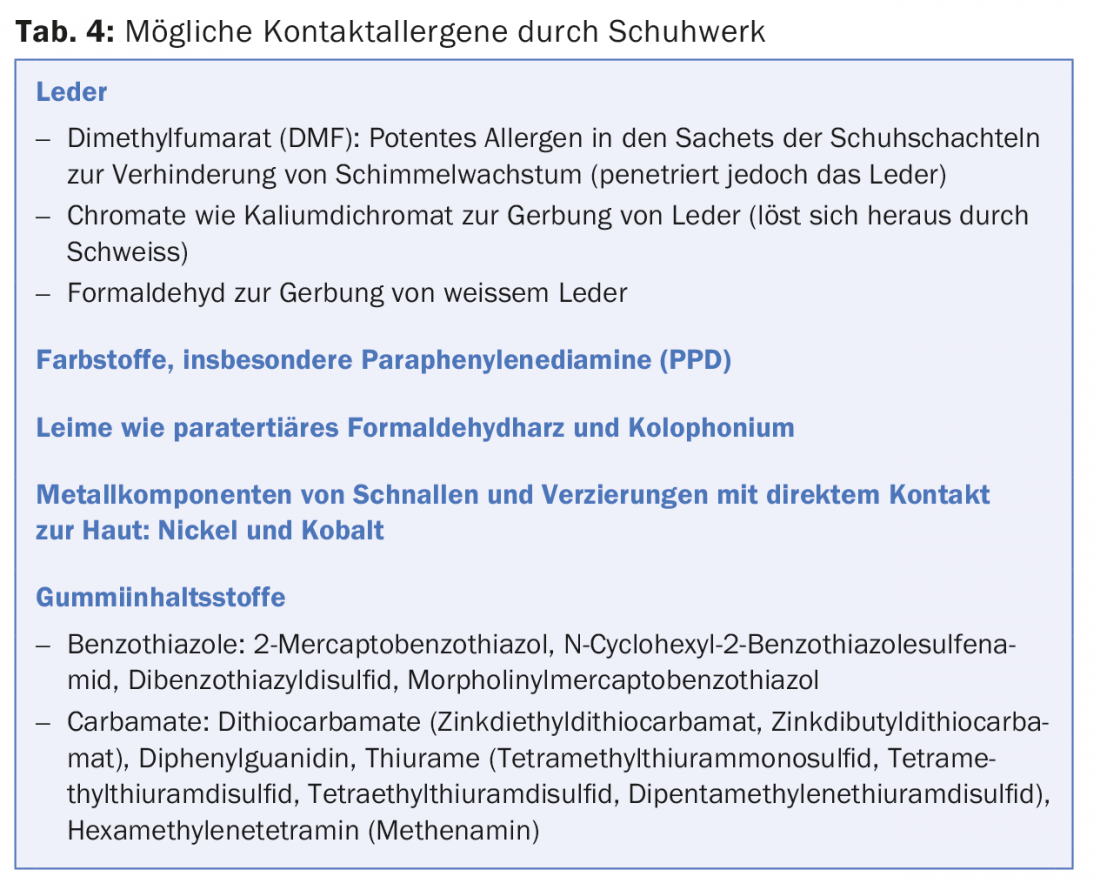
Now, under four antihistamines, Mr. Biner was doing better while fishing. Suddenly, however, his feet itched and he developed increasing papulovesicles on the inside of both feet, which spread to his knees (even after changing rubber boots). Therefore, an extensive search for contact allergies by epicutaneous test at the dermatologist’s office was now carried out. Late type sensitization to thiuram and mercapto mix, rubber ingredients was found.
Note: The possible contact allergens on the foot are manifold and range from care products, leather ingredients to a wide range of rubber ingredients (mostly vulcanizers, Tab. 4). Glue components and dyes can also be allergens. Bacterial infections such as gram-negative foot infection also sometimes lead to severe palmoplantar eczema. Not only boots can trigger one, but also tennis shoes, sandals and flip-flops (Tab. 4).
Contact allergic eczema of the foot (Fig. 3) usually begins at the base of the big toe and progressively spreads to the other toes and the rest of the foot.

On a very warm spring morning at 6 o’clock, Mr. Biner caught a salmon trout. But for a dinner it needed another catch. So he stayed and a few hours later ate a sesame roll with Emmental and butter for lunch. Soon after, he noticed that breathing became a little heavier for about two hours. What had he reacted to?
Note: grain and cereal allergies in grass pollen allergy are possible. Cross reactions/allergies are: Mugwort pollen, millet, sunflower seeds, buckwheat, sesame, corn (rare), rice (rare), barley (very rare), oats (very rare), wheat, spelt and rye flour (especially in commercial contact, e.g. bakers).
But the second catch did not want to succeed – not all morning and not in the afternoon. Until finally at 5 pm a salmon trout bit again. Both fish were later served for dinner, which, however, did not taste equally good to his wife. She thought the fish was too soft. An hour after eating, she vomited with abdominal cramps; in addition, she developed marked redness on her face and all over her upper body with itching. Quickly, the husband handed her the emergency kit. What had happened? The emergency doctor said: fish poisoning!
Note: Scombroid poisoning is a poisoning condition caused by eating certain types of fish (fish from the Scombridae family such as tuna and mackerel). The fish flesh is rich in free histine, so in the process of spoilage by decarboxylases, high concentrations of histamine are produced, which are responsible for the symptoms. Spoilage often begins before the fish is canned. In histamine poisoning (biogenic amines), the threshold toxicological dose of fish meat is 100-500 mg/kg. Within a few minutes to three hours after eating the fish, nausea, nausea, diarrhea, headache, skin redness, urticaria, and angioedema occur. Burning of the lips is often noticed while eating.
After that, Mr. Biner had enough of fishing. And what has become of him? First, he sold all his things (including the remaining pumpkin seed flour). As an IT specialist, he then created a fish app in which you can go deep-sea fishing virtually anywhere in the world – including big fish, with or without histamine.
Further reading:
- Reindl J, Anliker MD, et al: Allergy caused by ingestion of zucchini (Cucurbita pepo): characterization of allergens and cross-reactivity to pollen and other foods. J Allergy Clin Immunol 2000 Aug; 106(2): 379-385.
- Anliker MD, Wüthrich B: Atopy and hymenopteran venom allergy. Allergology 1999; 22suppl: 46-47.
- Confino-Cohen R, Goldberg A: Allergen immunotherapy-induced biphasic systemic reactions: incidence, characteristics, and outcome: a prospective study. Ann Allergy Asthma Immunol 2010 Jan; 104(1): 73-78.
- Yu GP, Wanderer AA, Mahmoudi M: Cold urticaria. In: Mahmoudi M (Ed.): Challenging Cases in Allergic and Immunologic Diseases of the Skin. Springer Verlag 2010; 25-42.
- Matthys E, Zahir A, Ehrlich A: Shoe allergic contact dermatitis. Dermatitis 2014; 25(4): 163-171.
- Thyssen JP, et al: Consumer leather exposure: an unrecognized cause of cobalt sensitization. Contact Dermatitis 2013 Nov; 69(5): 276-279.
- Gruber P, et al: Role of the polypeptide backbone and post-translational modifications in cross-reactivity of Art v 1, the major mugwort pollen allergen. Biol Chem 2009; 390(5-6): 445-451.
- Garcia Ortiz JC, Cosmes PM, Lopez-Asunsolo A: Allergy to foods in patients monosensitized to Artemisia pollen. Allergy 1996 Dec; 51(12): 927-931.
- Palacin A, et al: Anaphylaxis to wheat flour-derived foodstuffs and the lipid transfer protein syndrome: a potential role of wheat lipid transfer protein Tri a 14. Int Arch Allergy Immunol 2010; 152(2): 178-183.
- Moon JS, et al: Isolation and characterization of histamine-producing bacteria from fermented fish products. J Microbiol 2013 Dec; 51(6): 881-885.
DERMATOLOGIE PRAXIS 2016; 26(3): 6-9











