Diabetes does not hurt – one would almost like to add “unfortunately”. This is because the number of unreported cases of affected patients is still high. Possible late effects of the disease, especially if it is not treated or treated late, can be serious. In the process, the therapy has been steadily improved in recent years. Glucagon-like peptide 1 (GLP1) analogs have also provided a new treatment option that works quickly and effectively.
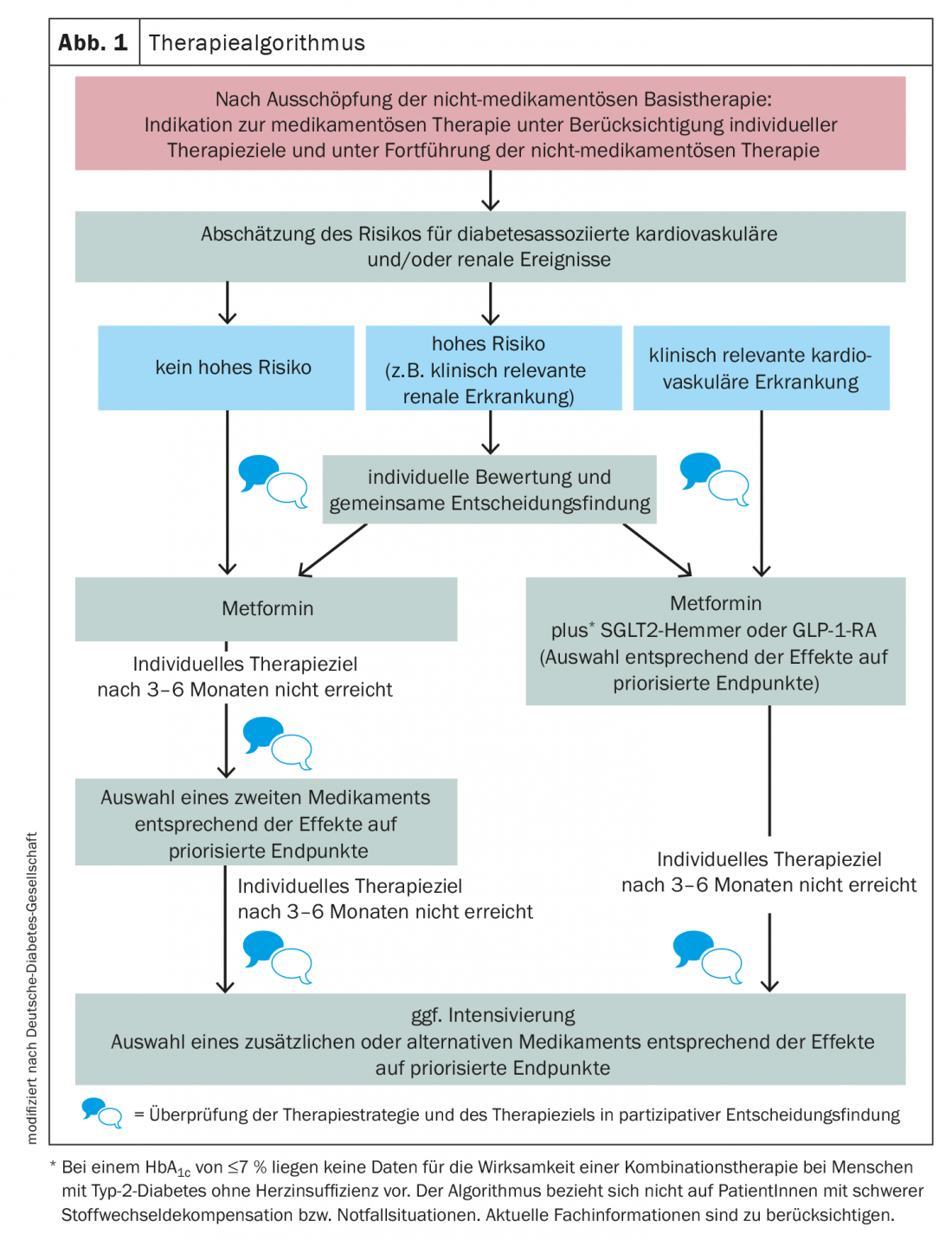
Diabetes mellitus is a serious disease that is a high risk factor for comorbid diseases, especially cardiovascular disease. It is estimated that around 500,000 people in Switzerland are affected. However, about half of those affected are still unaware of their disease. On average, it takes seven years for the diagnosis to be made. Valuable time that could already be used effectively for treatment. The sooner blood glucose levels can be adjusted through sufficient exercise, a balanced diet and adequate drug therapy, the sooner acute symptoms and late effects can be avoided. Current guidelines recommend lifestyle modification and the use of metformin as first-line treatment for type 2 diabetes mellitus (Fig. 1) . The HbA1c value is still considered the glycemic standard for long-term therapy management. However, there has now been a shift from a rigid target value to a target corridor. This is between 6.5 and 7.5% (48-58 mmol/mol Hb), but should be determined on an individual basis. Therapy goals depend on patient preference, comorbidity, age and life expectancy, quality of life, cultural conditions, psychosocial circumstances and opportunities, and abilities of the affected person.
Supplementary GLP1 administration
Already in addition to first-line therapy, a GLP1 analogue can be added if the risk of a diabetes-related cardiovascular and/or renal event is high or if clinically relevant cardiovascular disease is already present. GLP1 analogues are preparations that mimic the action of the natural incretin hormone. Incretins are formed in the intestine and regulate blood glucose by stimulating insulin secretion in the pancreas. GLP1 receptor agonists promote insulin secretion from pancreatic beta cells in a glucose-dependent manner, decrease glucagon secretion from alpha cells resulting in decreased glucose release by the liver, increase insulin sensitivity, and slow gastric emptying, thereby reducing the rate at which glucose enters the bloodstream. Another advantage: there is no risk of hypoglycemia.
In addition, GLP1 administration has been shown to lead to weight reduction and, with regard to cardiovascular events, a reduction in morbidity and mortality rates has been observed.
Usually, GLP1 analogues are administered subcutaneously – often once a week is sufficient. In Switzerland, for example, exenatide, liraglutide, lixisenatide and dulaglutide are currently approved. Semaglutide is the first GLP1 analog to be newly available as a tablet for oral administration in addition to subcutaneous administration.
Further reading:
- www.diabetesschweiz.ch/ueber-diabetes.html (last accessed 17.01.2021)
- www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/gesundheitszustand/krankheiten/diabetes.html (last accessed on 17.01.2021)
- www.deutsche-diabetes-gesellschaft.de/behandlung/leitlinien (last accessed on 17.01.2021)
CARDIOVASC 2021; 20(1): 30











