Human papilloma viruses have long been known to be the main cause of cervical cancer. They are among the most common sexually transmitted pathogens. But there is protection against it: The HPV vaccination. It is effective against the most common cancer-causing HP viruses and should ideally be done before the first sexual contact. In the meantime, a significant decrease in cervical carcinomas has been demonstrated.
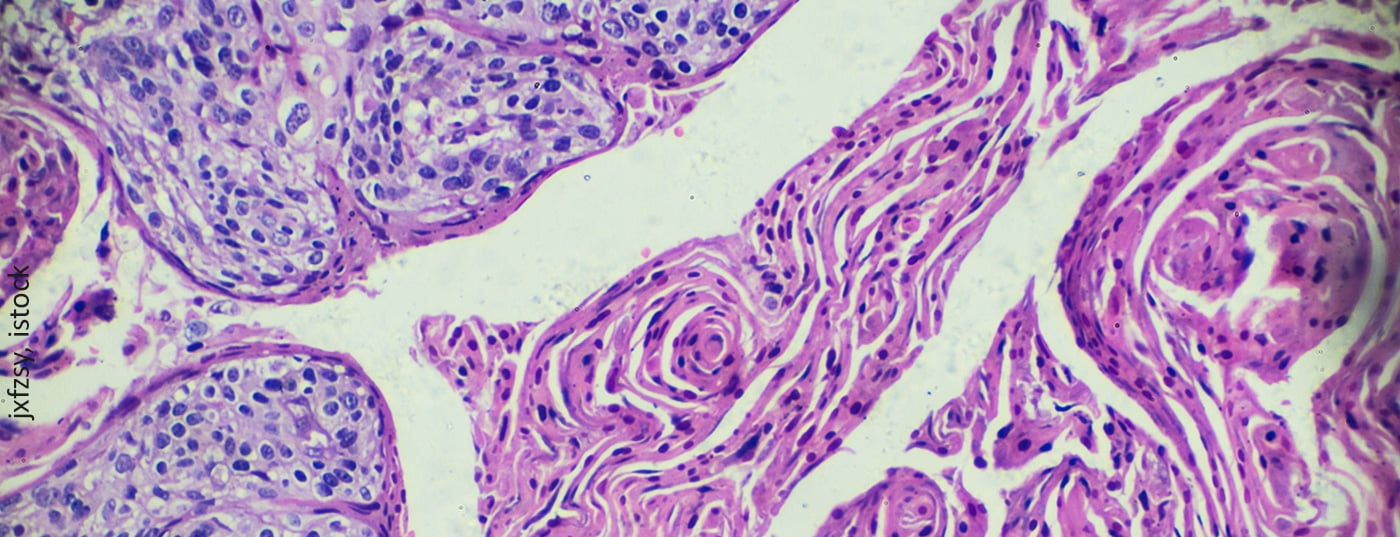
Most sexually active people become infected with human papillomavirus (HPV) at least once in their lifetime. To date, more than 200 different types of HP viruses are known. Some can trigger the formation of papillomas, and about 40 HPV types result in infections of skin and mucosal cells in the genital area. The viruses penetrate via micro-injuries of the skin or mucosa and infect the epithelial cells of the basal cell layer. In most cases, this infection runs without symptoms. What’s more, these are transient infections that are no longer detectable after two years at the latest. However, not always. HPV infections can also persist and lead to squamous cell carcinoma in the anogential region, oral cavity, or pharynx via precancerous lesions. Cervical carcinoma often develops in women. About 10% of HPV infections at the cervix result in higher grade precancerous lesions. If these are not treated, cervical cancers can develop in approximately 30-50% of cases within 30 years.
Vaccination reduces cancer rate
The first HPV vaccines were approved in the mid-2000s. Large-scale vaccination campaigns for young girls in Australia and the United Kingdom soon followed. Therefore, after a short period of time, it could be demonstrated that the rate of condyloma decreased significantly. However, since cervical carcinoma does not manifest itself until later in life, evidence for the cancer rate has been lacking to date. This evidence has now been taken up by British scientists. They wanted to know whether the HPV vaccination campaign established since 2008 among 12-13-year-old girls in England has had an effect on the risk of early-onset and invasive cervical cancer. More specifically, whether rates of carcinoma and its precursors, grade 3 cervical intraepithelial neoplasia (CIN), have decreased. For this purpose, data from the Cancer Registry on cervical cancer and CIN3 in women aged 20 to 64 years were analyzed. Three cohorts accounted for differences in national coverage and school year. A total of 13.7 million years of follow-up were evaluated. The estimated relative reduction in cervical cancer rates by age with vaccination was 34% for 16-18 year olds (school year 12-13), 62% for 14-16 year olds (school year 10-11), and 87% for 12-13 year olds (school year 8), compared with the unvaccinated reference cohort. The corresponding risk reductions for CIN3 were 39%, 75%, and 97%. By June 30, 2019, there were an estimated 448 fewer than expected cervical cancer cases and 17,235 fewer than expected cases of CIN3 in the vaccinated cohorts. These figures indicate a significant decrease in cervical cancers – especially among women who were vaccinated at age 12-13. The HPV vaccination program has nearly eliminated cervical cancer in young women born after September 1, 1995. .
In Switzerland, vaccination is recommended by the FOPH and EKIF for all adolescents between the ages of 11 and 14. Since HPV-associated diseases are more common in women than in men, vaccination is recommended for girls as a basic vaccination and for boys as a supplementary vaccination. It is estimated that HPV vaccination in Switzerland could prevent 80 to 180 new cases of cancer in men and about 300 cases of cancer in women each year. In addition, the two available vaccines are characterized by extremely good tolerability. So far, only skin reactions at the injection site have been observed.
Further reading:
- www.rki.de/SharedDocs/FAQ/Impfen/HPV/FAQ-Liste_HPV_Impfen.html
- www.gesundheitsinformation.de/hpv-impfung-gegen-gebaermutterhalskrebs.html
- www.gelbe-liste.de/gynaekologie/hpv-impfung-schutz-zervixkarzinom
- www.infovac.ch/de/impfunge/nach-krankheiten-geordnet/hpv
- www.bag.admin.ch/bag/de/home/krankheiten/krankheiten-im-ueberblick/hpv.html
InFo ONCOLOGY & HEMATOLOGY 2022; 10(2): 26.