Case report: The 56-year-old patient had been suffering from headache and nausea and increasing psychomotor slowing for three months. Clinically, he presented with left facial nerve mouth branch weakness, left arm mild hemiparesis, and left neglect. Singultus was seen as a sign of increased intracranial pressure. An imaging workup was initiated by the primary care physician, which revealed a large right temporal space mass.
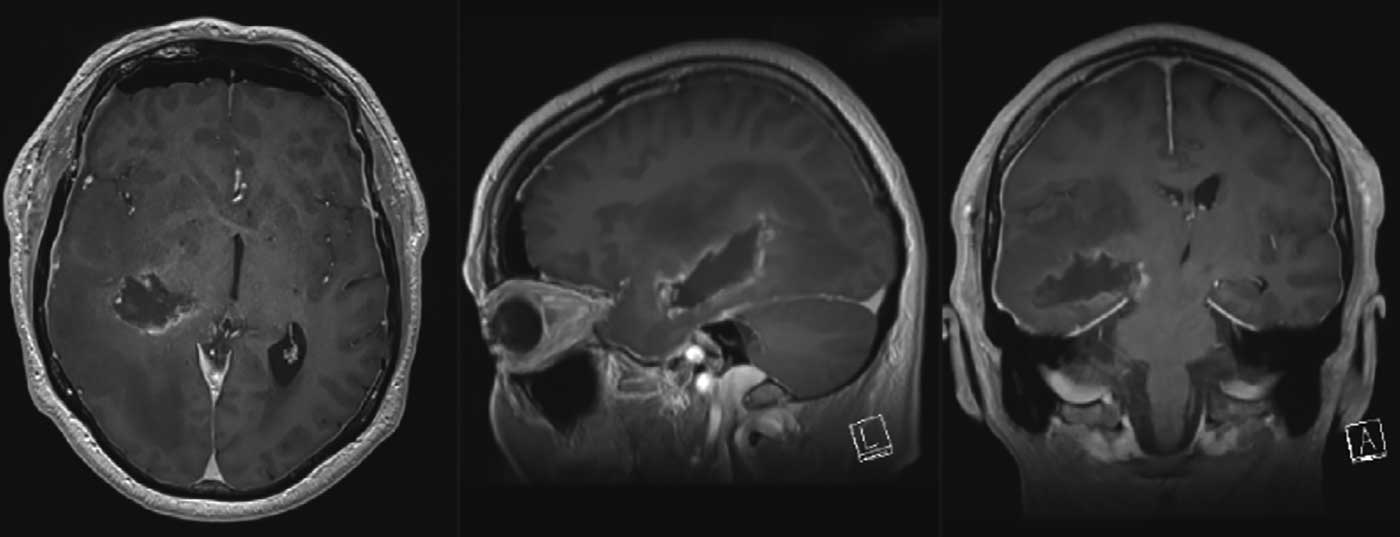
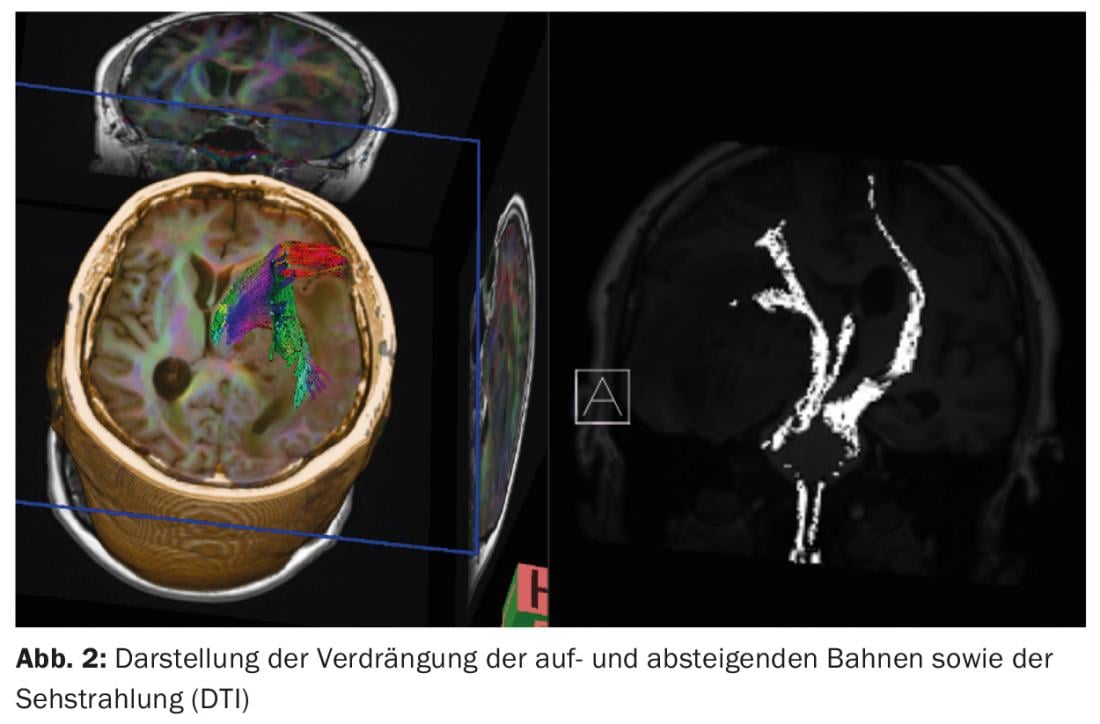
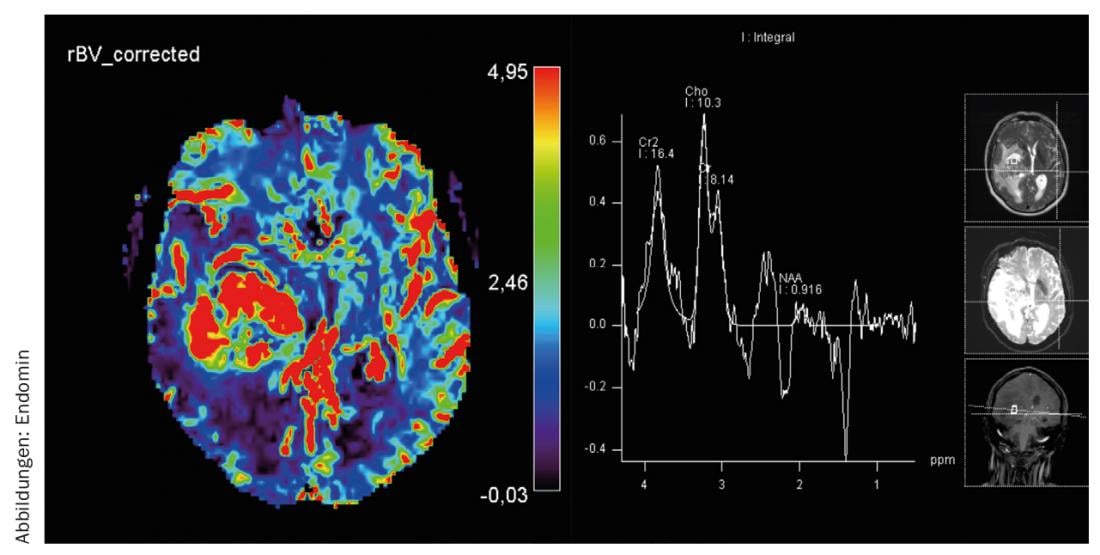
MRI diagnosis: a 60×45×40 mm inhomogeneous mass with solid and cystic portions receiving contrast at the margins is seen. Additionally, a large perifocal edema is seen. According to the centerline shift of 12 mm, the pyramid trajectory is strongly shifted to the left. The tumor reaches the thalamus and midbrain, which are also compressed and displaced. 1H spectroscopy and MR perfusion support the presence of malignant glioma (Figs. 1-3).

Surgery: anti-edematous therapy with dexamethasone 16 mg/d was started at hospitalization. The patient is positioned on the back, the head is fixed rotated to the left, and an intraoperative MRI is obtained (Fig. 4) .

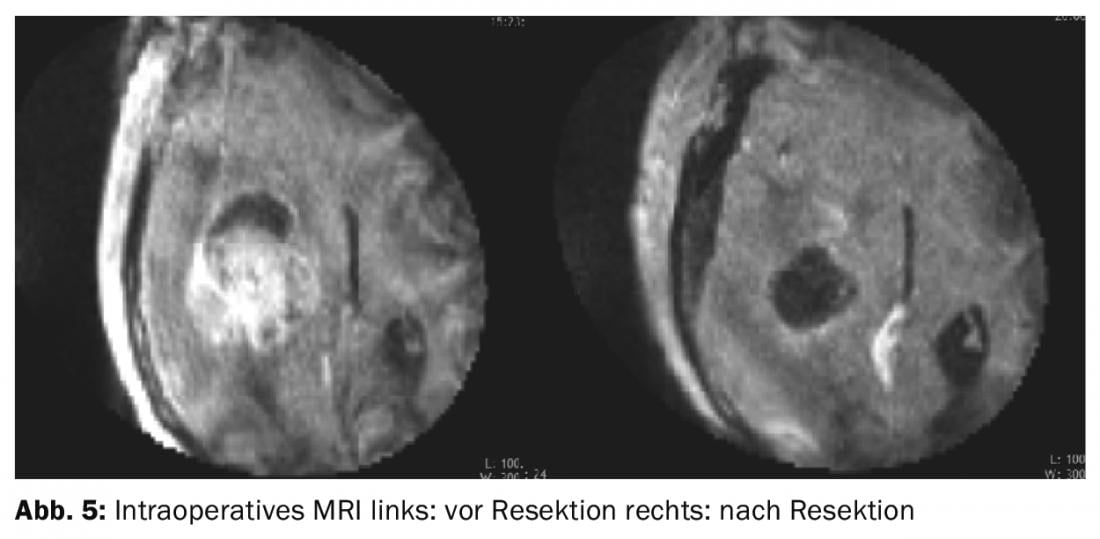
Multimodal intraoperative neuromonitoring with SEP, EEG, and transcortical motor stimulation is established to monitor the descending and ascending pathways. A small, 2×2 cm temporobasal craniotomy is intentionally created to prevent herniation of brain tissue through the skull opening. The surgical microscope is now used to dissect transcortically in the direction of the tumor. After relieving multiple tumor cysts, sufficient space can be obtained to identify the boundary between tumor and healthy brain tissue and perform resection along it. Areas of the resection cavity not visible through the microscope are not visualized by retraction of healthy brain tissue, but are inspected with the endoscope and pathologic tissue is removed in an endoscopically controlled manner. Contrast-enhanced intraoperative MRI demonstrates complete resection of all contrast-absorbing tumor at the end of surgery (Fig. 5).
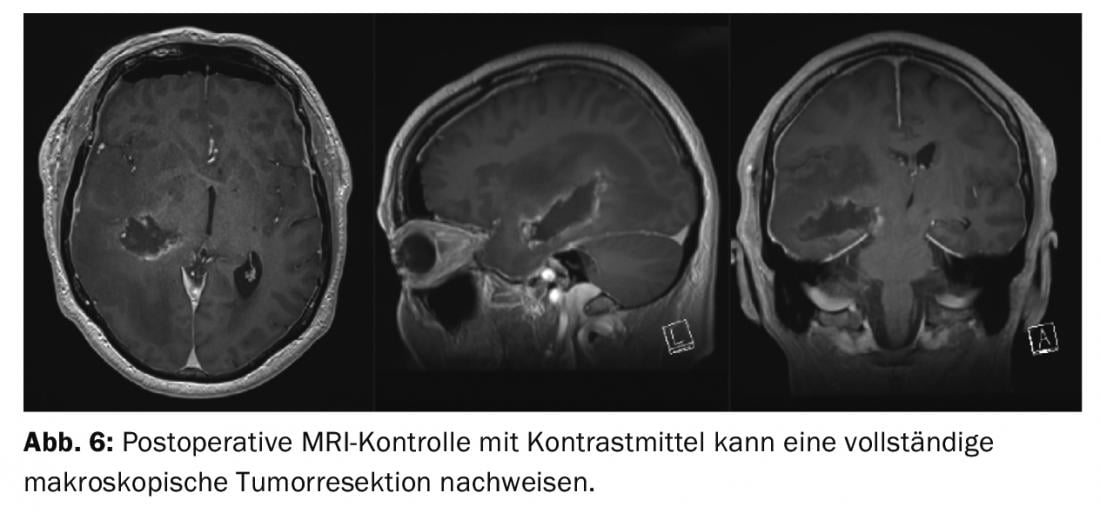
Postoperative course: The patient was extubated without problems and showed no new focal neurological deficits. As the patient progressed, psychomotor slowing and hemiparesis improved significantly. Neuropathologic workup revealed a WHO IV° glioblastoma. The patient was able to discharge home after four days and is receiving combined radio-chemotherapy with Temodal as an outpatient (Fig. 6).
CONCLUSION: Large space-occupying lesions are frequently resected via extended craniotomies, with corresponding access-related injury to healthy tissue. However, deep-seated tumors are predestined for a minimally invasive surgical approach (Fig. 7) .
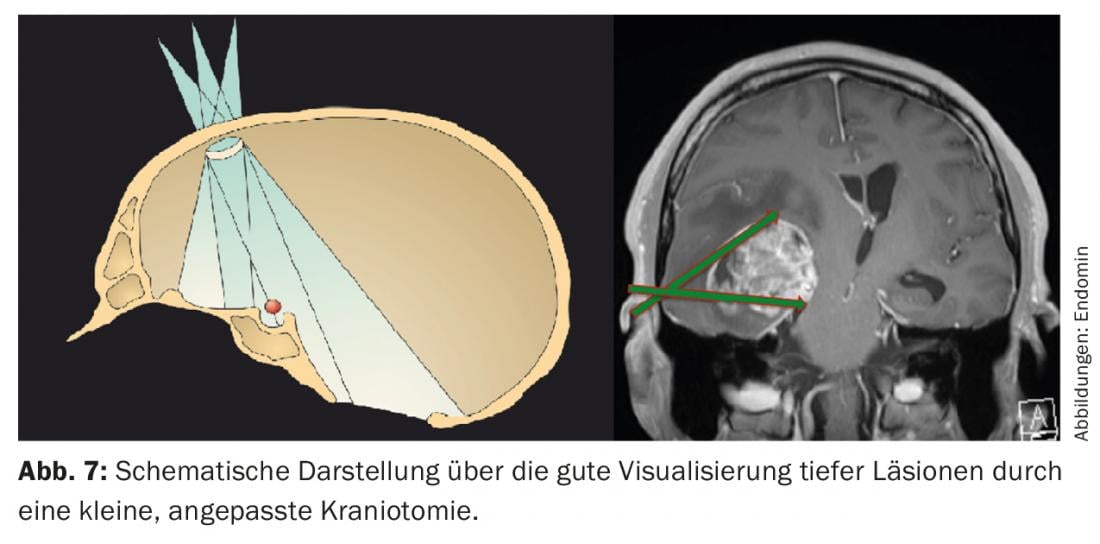
Consistent use of neuronavigation, intraoperative endoscopy, neurophysiologic monitoring, and intraoperative MRI allow for maximum surgical radicality while minimizing surgical trauma through a small keyhole craniotomy. Thus, functionally intact brain tissue in the area of the access and around the lesion is spared and not affected.
InFo NEUROLOGY & PSYCHIATRY 2017; 15(1): 30-31.