In 2013, the European Society of Cardiology (ESC) published new guidelines on various cardiovascular diseases. These were presented in a Main Session at the Annual Meeting of the Swiss Society of Cardiology on June 12, 2014. The focus was on the management of patients with arterial hypertension, stable coronary artery disease (CAD) and diabetes resp. Pre-diabetes.
(ee) The guidelines on hypertension were presented by PD Gregoire Würzner, MD, CHUV Lausanne. In particular, there were some changes in the diagnosis of hypertension compared with older guidelines. Conventional blood pressure (BP) measurement in the office remains the gold standard for screening, diagnosis, and management of hypertension. Hypertension is diagnosed when at least two BP measurements over the course of at least two consultations show values ≥140/≥90 mmHg.
Management of arterial hypertension
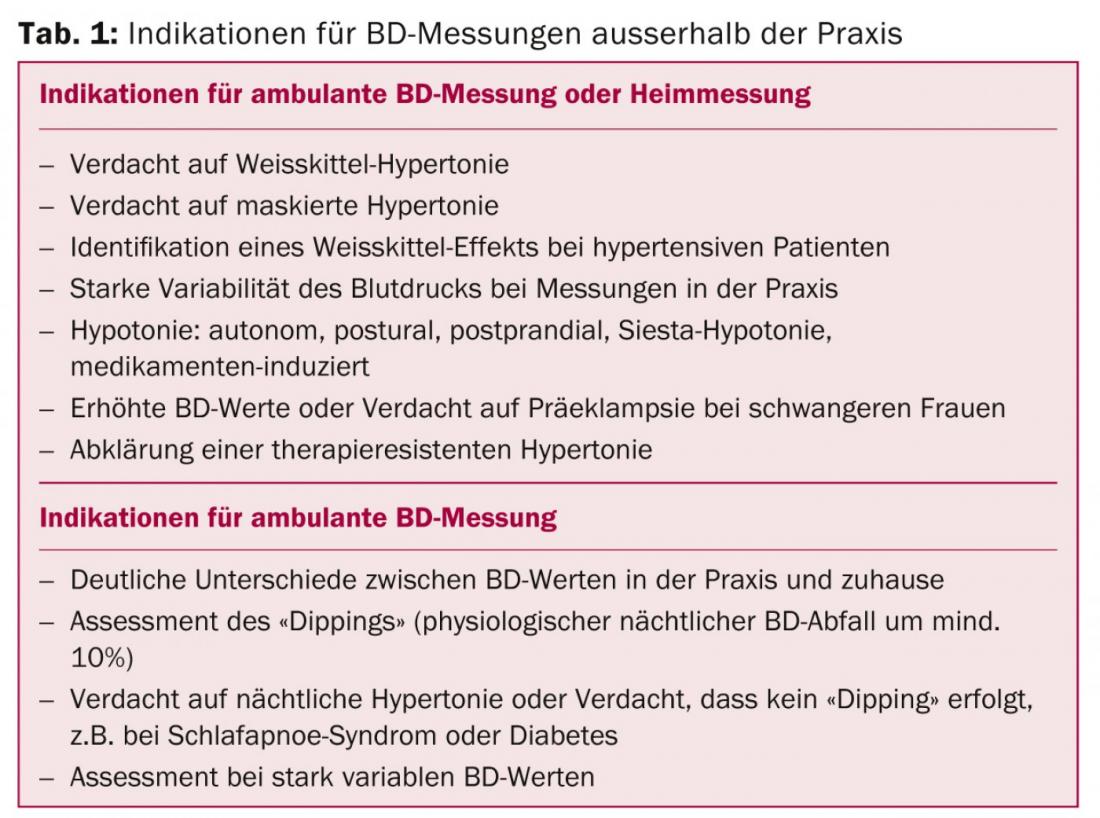
BP measurements outside the office, either as ambulatory measurements or BP measurements at home (home measurements by the patient himself), are important complements to office measurements because they can detect masked hypertension. The incidence of cardiovascular events is twice as high in subjects with masked hypertension as in normotensive subjects. The cut-off values for hypertension in ambulatory measurement are:
- 130/80 mmHg at 24-hour measurement
- 135/85 mmHg for outpatient measurement or home measurement during the day resp. in awake state
- 120/70 mmHg for a nocturnal measurement resp. Asleep
The indications for ambulatory BP measurements or home measurements are listed in Table 1. “Upgrading outpatient measurements is a change from the past,” the speaker emphasized, “because as a physician, you can no longer ‘rest’ on your office measurements.”
In each patient, cardiovascular risk must be determined in relation to hypertension and depending on other risk factors. Further therapy depends on the risk. The goal is BP values below 140/90 mmHg – this applies to almost all patients. The former motto “the lower the better” is passé. Exceptions are diabetics (diastolic BP ≥85 mmHg) and elderly patients (systolic BP 140-150 mmHG). In the UK NICE guidelines, the target BP values are somewhat lower still.
Management of stable CHD
Prof. Michael Zellweger, MD, University Hospital Basel, spoke about the latest ESC guidelines for stable CHD (sCAD). Compared with previous guidelines, there is a greater emphasis on separating risk stratification from the diagnostic process. Diagnostic measures should depend on the pretest probability that the patient really has sCAD. The guidelines include a table that can be used to estimate the likelihood of coronary stenosis based on the patient’s age, sex, and symptoms (typical angina, atypical angina, no angina pain). The older the patient, the greater the likelihood, and men are significantly more likely than women.
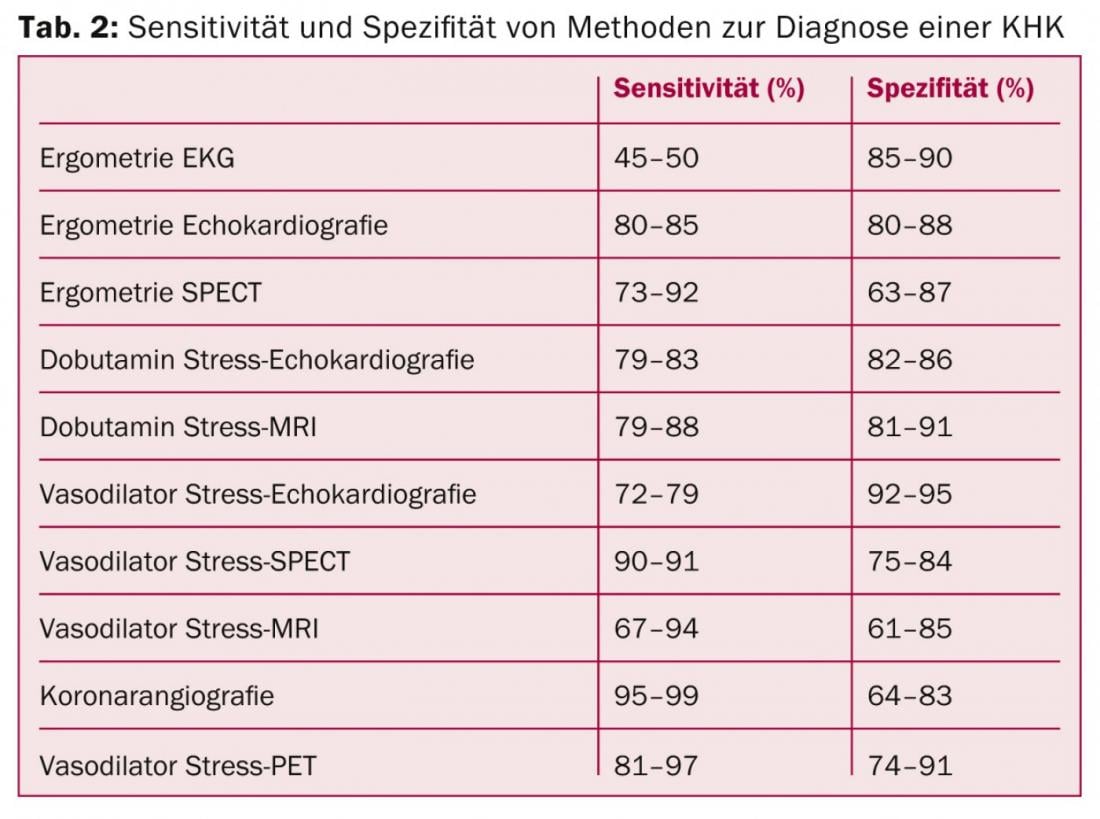
In patients with a low pretest probability of coronary stenosis (less than 15%), no further diagnostics other than the usual diagnostics (ECG, laboratory) are recommended because the risk of harm to the patient is higher than the potential benefit. In patients with a high pretest probability (above 85%), angiography should be performed directly, at least as far as the diagnostic aspect is concerned. The situation is quite complex in patients with an “intermediate” risk (15-85%): Here, primarily an ischemia search should be performed, whereas the pure stress test without imaging has lost importance. In patients with a probability of 15-50%, CT coronary angiography may be considered if the patient is suitable and the appropriate infrastructure and expertise are available. Modern imaging techniques have more weight in the new guidelines (Table 2).
Prognosis can be estimated with a nomogram based on the results of ergometry. In imaging ischemia diagnosis, the extent of ischemia is critical. The further management depends on the risk resp. the prognosis; either the patient is revascularized or optimally treated with drugs. A handy diagram is also provided in the guidelines to facilitate the decision whether to perform a percutaneous intervention or bypass surgery. In conclusion, Prof. Zellweger again mentioned the points that should not be forgotten in the management of patients with sCAD: Risk evaluation, lifestyle changes, optimal use of medications, and attention to the patient’s quality of life and side effects of the medications.
Management of CHD in diabetes
The ESC guidelines on diabetes were presented by Prof. Marco Roffi, MD, University Hospital of Geneva. The diagnostic criteria have changed in recent years. Regarding cardiovascular risk, there are only two risk categories for diabetics: very high risk (diabetes and at least one cardiovascular event) and high risk (all diabetics). Screening for silent myocardial ischemia is generally not necessary and should be considered only in high-risk patients in special situations. For microvascular prevention, the therapeutic goal is clear: HbA1c should be below 7% (6-6.5% in young patients, 7.5-8% in older patients with long or complicated disease). Hypoglycemia must be avoided at all costs. Regarding therapeutic targets for the prevention of macrovascular complications, the evidence is unclear. Not all diabetics benefit equally from aggressive glucose management. It is therefore important to individualize treatment goals and adapt them to factors such as personal motivation, disease duration, comorbidities, life expectancy, and preexisting vascular complications. With regard to blood pressure reduction, the following now applies: “The lower may not be the better”; values below 130/80 mmHg are no longer targeted. Aspirin is used only in secondary prevention.
- The new guidelines are available for download on the ESC website: www.escardio.org/guidelines











