For the 16th time, the traditional State-of-the-Art Symposium of the Swiss Multiple Sclerosis Society took place in Lucerne in January 2014. This time, the presentations by national and international MS specialists focused on the topic of progressive multiple sclerosis. As it turned out, many questions are still open in this form of the disease. In particular, there is a lack of a good animal model that could be used to shed more light on the issue.
In her welcoming remarks, Patricia Monin, Director of the Swiss Multiple Sclerosis Society, emphasized the great importance of progressive multiple sclerosis (MS): “Many of the questions that reach us every day are related to this form of the disease. Affected people are desperate and ask us if there is any hope for them and if there will be a treatment option for them in the future.” She therefore encouraged the researchers present to focus their work on this area in the coming years. The MS Society supports several projects throughout Switzerland that also address progressive MS.
Not a good animal model
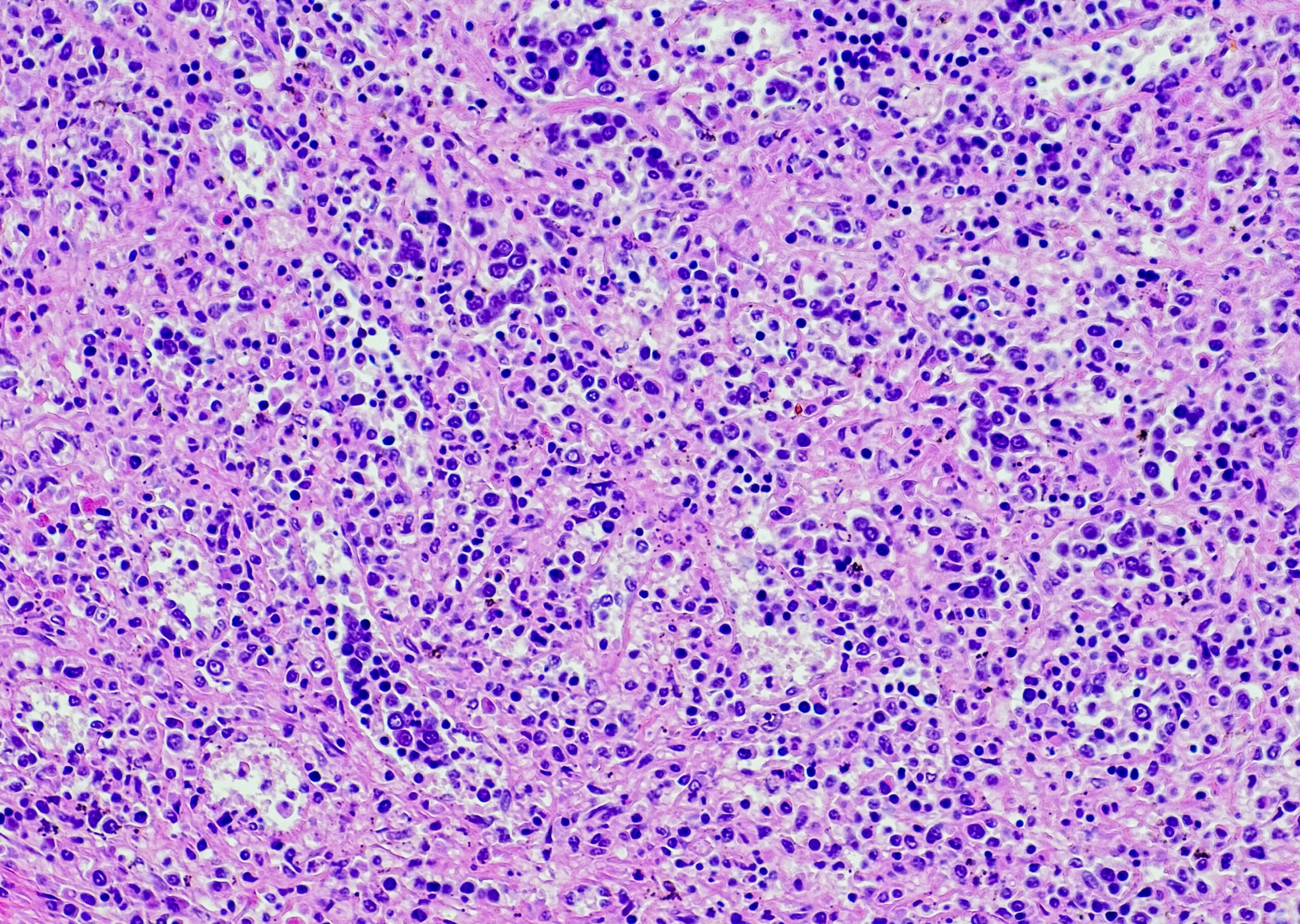
The first speaker at the symposium, pathologist Prof. Christine Stadelmann-Nessler, MD, Göttingen, Germany, addressed why research on progressive MS is so difficult: “While we know that the progressive phase of MS is pathologically characterized by a predominance of inactive or chronically active smoldering lesions, extensive cortical demyelination, increasing axonal loss, and neuronal dysfunction, we have not yet been able to identify the pathology of progressive MS. Recently, significant meningeal lymphocyte infiltration associated with this phase of the disease has also been reported.” Nevertheless, however, knowledge of the pathogenesis of progressive MS remains limited. “Unfortunately, there is no suitable animal model that would be really good for studying chronic demyelination, whether of the white or gray matter,” she indicated. Recent efforts here have focused particularly on the toxic demyelination model [1]. “This model will be used to study the effect of protracted or recurrent demyelination on axonal function,” Prof. Stadelmann-Nessler explained. Genetic models – mice with targeted deletion of relevant myelin genes – could also provide important insights in the future.
Further advances in imaging techniques
Due to its very high sensitivity for MS-related changes, MRI is an established method to diagnose this disease or to monitor its progression. “However, MRI parameters have limited ability to explain clinical status and disability progression in patients with established MS,” said the next speaker, Maria A. Rocca, MD, Milan. This has led to increased use of magnetic resonance-based technologies to better assess the disease burden of patients at different stages of disease, he said. “The application of these techniques allowed graduation of heterogeneous pathologic MS lesions in vivo, not only for focal lesions but also for normal-appearing white and gray matter,” Dr. Rocca explained. Recently, other aspects of MS pathology have also become quantifiable, including macrophage infiltration and pathological iron depots. “Further, functional MRI data provided significant insights into cortical reorganization and its potentially important role in limiting the clinical consequences of structural damage,” the speaker continued. The increasing availability of scanners with ultra-high magnetic fields (7 Tesla or more, instead of 1.5 Tesla) allows important insights into the pathogenesis of MS. The advantages of this technique include better visualization of white matter lesions and their morphologic characteristics, improved ability to visualize and localize gray matter lesions, and quantification of specific metabolites that may play a role in axonal degeneration [2]. “All of these advances are helping us to continually improve our understanding of multiple sclerosis – including the factors associated with progression,” Dr. Rocca concluded.
Optical coherence tomography for objective detection of progression?
The eye is a unique, direct “window” to the brain, as the retina is the only way to see neurons and axons directly. Optical coherence tomography (OCT) technology allows the different layers of the retina to be assessed. Axel Petzold, MD, Amsterdam, explained: “We use this technique to measure the thickness of the different retinal layers. So there are three possibilities with this: Either a layer is normal, too thick or too thin.” The accuracy of the method has proven to be exceptionally high [3]. “OCT represents the most accurate technique I have encountered during my scientific career,” the speaker emphasized.
The use of OCT has, among other things, allowed the increase in macular volume to be detected with fingolimod therapy [4]. Gelfand et al. found microcystic macular edema (MMO) by OCT in 15 of 318 (4.7%) patients with MS, while no changes were detected in 52 healthy controls [5]. The MMO mainly affected the inner nuclear layer (INL) of the retina. MS patients with MMO were more disabled (median EDSS 4) than patients without (median EDSS 2) (p=0.0002). In addition, patients with MMO had a higher MSSS (“Multiple Sclerosis Severity Score”), a measure of disease progression. Finally, retinal changes occurred more frequently in eyes with previous optic neuritis (50 vs. 27%). “However, the results of the work by Saidha et al. seem most important to me,” Dr. Petzold continued. “This group was able to show by OCT that there was a correlation between the increase in thickness of the INL and disease activity” [6]. If this finding is further confirmed, INL thickness could be used as a useful predictor of disease progression. However, it is also important to remember that microcystic macular edema is not specific to MS; it can occur in a number of other conditions.
Several papers in recent years have also investigated whether retinal changes found by OCT differ in different MS subtypes. The results of these investigations have been largely negative. Only two recent studies have shown that retinal changes are more pronounced in progressive forms of MS or in more advanced stages of the disease [7, 8]. In addition, a correlation between previous optic neuritis and the severity of the changes could be established. Gelfand et al. found that retinal axon loss begins early in the course of MS [8]. A paper just published online concludes that the innermost retinal layers (nerve fiber and ganglion cell layer) are better preserved in primary progressive and benign MS compared to RRMS [9]. The authors interpret this observation as possibly limiting the sensitivity of the retina to neurodegeneration and emphasize that this may be important for future studies of neurodegeneration in patients with primary progressive MS.

Joining forces to research
Also emphasizing the importance of the progressive form of the disease, Prof. Alan Thompson, MD, London, opined in the introduction to his presentation: “There are few challenges in the field of multiple sclerosis that have such an enormous effect on patients as progression.” All the more surprising, then, that this form of MS has received rather little scientific or clinical interest until recently. “There have been some important developments in our understanding regarding the pathology of progression, yet many fundamental questions remain unanswered.” Therefore, in the future, it will be important to turn less to immunosuppression, for example, and more to the field of neuroprotection and repair mechanisms. “But this also means that we need new, innovative study designs to get to the target in a shorter time and with smaller numbers of patients,” Prof. Thompson indicated. In this context, the Multiple Sclerosis Outcome Assessments Consortium (MSOAC) has also recently been established [10]. The goal of this organization is to advance research into new therapies by developing new ways to capture treatment effects in clinical trials. Finally, Prof. Thompson also reported on the establishment of the international task force “Progressive MS Alliance” (www.endprogressivems.org). This alliance of various organizations, including the Multiple Sclerosis International Federation and several national MS societies, is working to link resources and experts worldwide to develop new solutions to combat progressive MS. The identification of experimental models and pathological mechanisms is also among the top priorities.
Source:16th State of the Art Symposium, Swiss Multiple Sclerosis Society, January 11, 2014, Lucerne.
Literature:
- Skripuletz T, et al: Cortical demyelination is prominent in the murine cuprizone model and is strain-dependent. Am J Pathol 2008; 172: 1053-1061.
- Filippi M, et al: Ultra-high-field MR imaging in multiple sclerosis. J Neurol Neurosurg Psychiatry 2014; 85: 60-66.
- Balk LJ, Petzold A: Influence of the eye-tracking-based follow-up function in retinal nerve fiber layer thickness using fourier-domain optical coherence tomography. Invest Ophthalmol Vis Sci 2013; 54: 3045.
- Nolan R, et al: Fingolimod treatment in multiple sclerosis leads to increased macular volume. Neurology 2013; 80: 139-144.
- Gelfand JM, et al: Microcystic macular oedema in multiple sclerosis is associated with disease severity. Brain 2012; 135: 1786-1793.
- Saidha S, et al: Microcystic macular oedema, thickness of the inner nuclear layer of the retina, and disease characteristics in multiple sclerosis: a retrospective study. Lancet Neurol 2012; 11: 963-972.
- Oberwahrenbrock T, et al: Retinal damage in multiple sclerosis disease subtypes measured by high-resolution optical coherence tomography. Mult Scler Int 2012; 2012: 530305.
- Gelfand JM, et al: Retinal axonal loss begins early in the course of multiple sclerosis and is similar between progressive phenotypes. PLoS One 2012; 7: e36847.
- Balk L, et al: Disease course heterogeneity and OCT in multiple sclerosis. Mult Scler 2014 Jan 8. [Epub ahead of print].
- Rudick RA, et al: Multiple Sclerosis Outcome Assessments Consortium: genesis and initial project plan. Mult Scler 2014; 20: 12-17.
InFo Neurology & Psychiatry 2014, 12(2): 32-35.