Ergometry remains an important test for diagnosis and risk stratification in the CHD work-up. For ergometry to be meaningful, normal exercise capacity and a resting ECG with normal ST segment are required. In interpretation, one must be aware of the low sensitivity of ergometry and, depending on the clinical context, follow up with further noninvasive investigations or proceed to invasive coronary angiography. As a diagnostic test, ergometry is most appropriate for patients with a pretest probability of %–65% for CHD. Ergometry provides important prognostic information in both intermediate (%–85%) and high (>85%) pretest probability of CHD.
The work-up process for coronary artery disease (CAD) and, in particular, the role of ergometry have changed dramatically in recent years with the availability of new imaging modalities. Nevertheless, as a readily available, inexpensive, and low-risk test, ergometry remains important in everyday practice for the diagnostic and prognostic evaluation of patients with possible CHD, which is outlined in the present review.
Tests for the detection of CHD
The non-invasive tests aim to answer two primary questions:
- Is CHD present or not?
- Can the patient be treated with optimal drug therapy (aspirin, statins, ACE inhibitors, possibly anti-ischemic therapy) or is revascularization additionally indicated for prognostic reasons? [1]
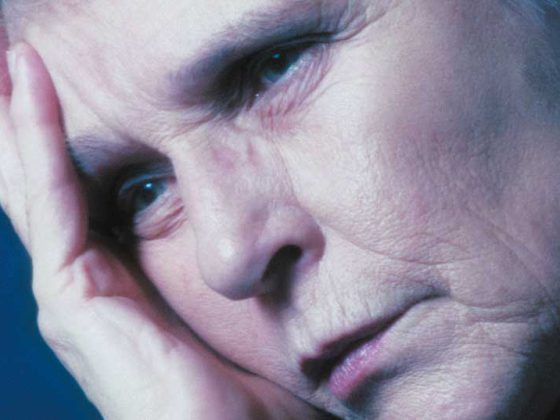
Two main principles of testing can be distinguished: Tests that visualize the substrate of myocardial ischemia, coronary stenosis (invasive coronary angiography, noninvasive computed tomography coronary angiography [Koronar-CT]), and tests that measure its effect, ischemia. Myocardial perfusion scintigraphy and cardiac stress MRI measure perfusion and inferior perfusion, respectively, stress echocardiography (and stress MRI with dobutamine) measures ischemia-induced left ventricular dysfunction, and ergometry measures ischemia-induced ST change (Fig. 1).
The anatomic tests and the different ischemia tests are based on different principles and may therefore give different results in the same patient. Thus, a patient with a 50% stenosis in the middle portion of the ramus circumflexus will not show ST changes on the exercise ECG because the stenosis does not yet provoke ischemia. However, the stenosis will be visible on coronary angiography or coronary CT. More severe stenosis will present as inferior perfusion on myocardial perfusion scintigraphy, but may not be extensive enough to provoke significant ST-segment depression on ergometry [1,2].
Ergometry for the diagnosis of CHD in patients with chest pain.
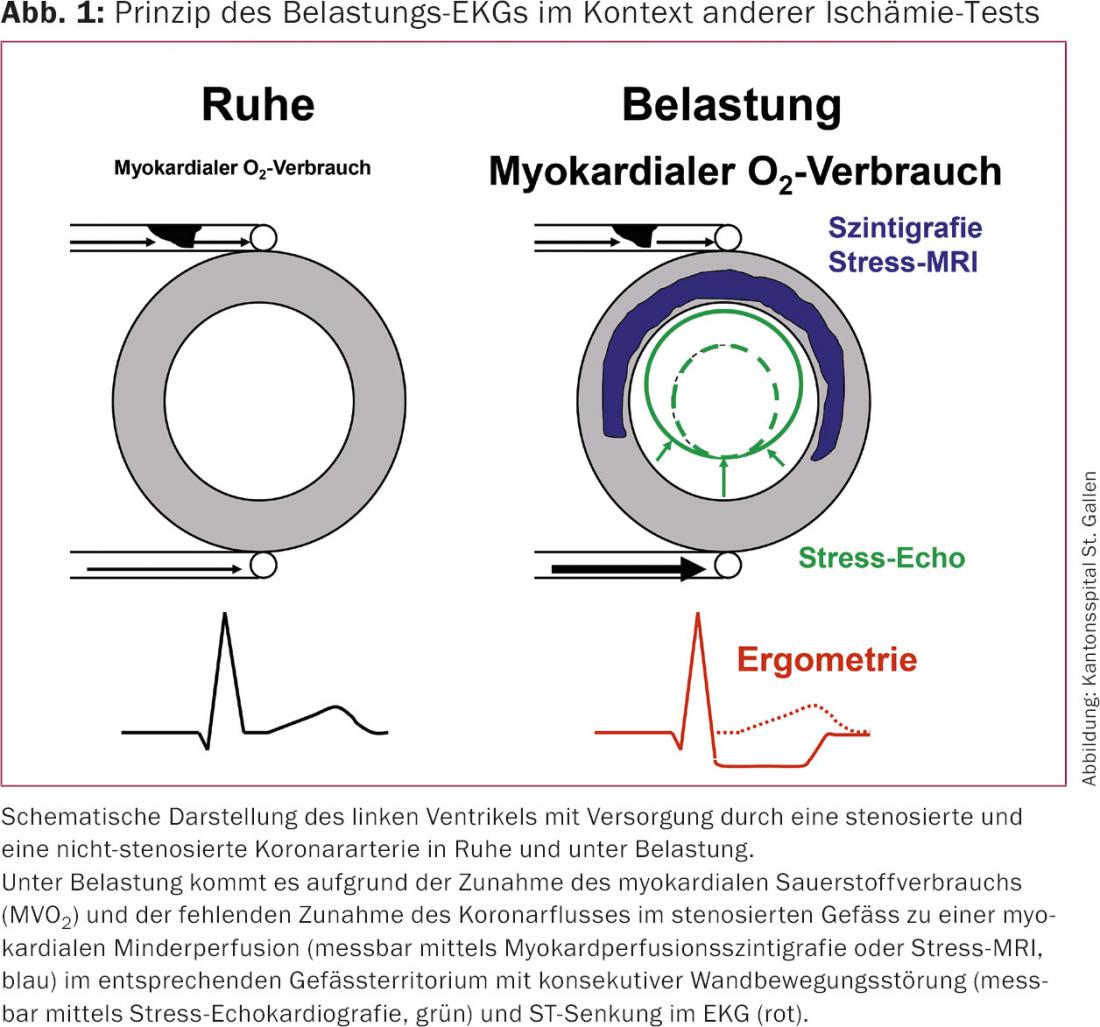
Ergometry must be used in such a way that we can expect a clinically relevant statement from the findings. Therefore, the use of ergometry first requires consideration of pre-test probability (PTP) and post-test probability – this according to Bayes’ theorem, which states that the post-test probability is directly proportional to the PTP as well as to the sensitivity of the test and indirectly proportional to the specificity of the test. Based on age, sex, and symptoms, a PTP results for the presence of relevant CHD (Table 1).
When using diagnostic tests, their sensitivity and specificity) must be considered in the context of PTP. In a man older than 70 years with typical angina, the diagnosis of CHD is already very likely based on the clinical constellation alone (PTP >85%), whereas in a woman younger than 50 years with atypical chest pain, CHD is very unlikely (PTP <15%). If a test provides more incorrect results than correct ones, this can lead to patient uncertainty and unnecessary follow-up tests.
Imaging ischemia tests (myocardial perfusion scintigraphy, stress echocardiography, stress MRI) have sensitivities and specificities around 85%, which means that 15% of all tests give a false result, so that in patients with a PTP of >85% or <15%, no test gives less false results than one test. Therefore, it is recommended that patients in these PTP categories not undergo testing for diagnostic purposes: PTP of >85% is assumed to be CHD, and PTP <15% is assumed not to be CHD.
On the other hand, there are many patients with a PTP of %–85% where a sufficiently good conclusion cannot be made by history alone and diagnostic tests are useful. Since ergometry has a low sensitivity of only about 50% even with correct patient selection (specificity is high at %–90%), the number of wrong tests becomes higher than the number of correct tests when PTP is higher than about 65%. It is therefore recommended that ergometry be used for diagnostic purposes in patients with a PTP of %–65% if a meaningful test can be expected. At a PTP of %–85%, imaging ischemia tests should be used if they are available and can be performed with good expertise. Otherwise, ergometry is also an option.
If ergometry is performed in patients with PTP %–85% and is negative, one must be aware of the low sensitivity of ergometry and possibly perform relatively low-threshold invasive coronary angiography, which can then provide evidence of ischemia by measuring fractional flow reserve.
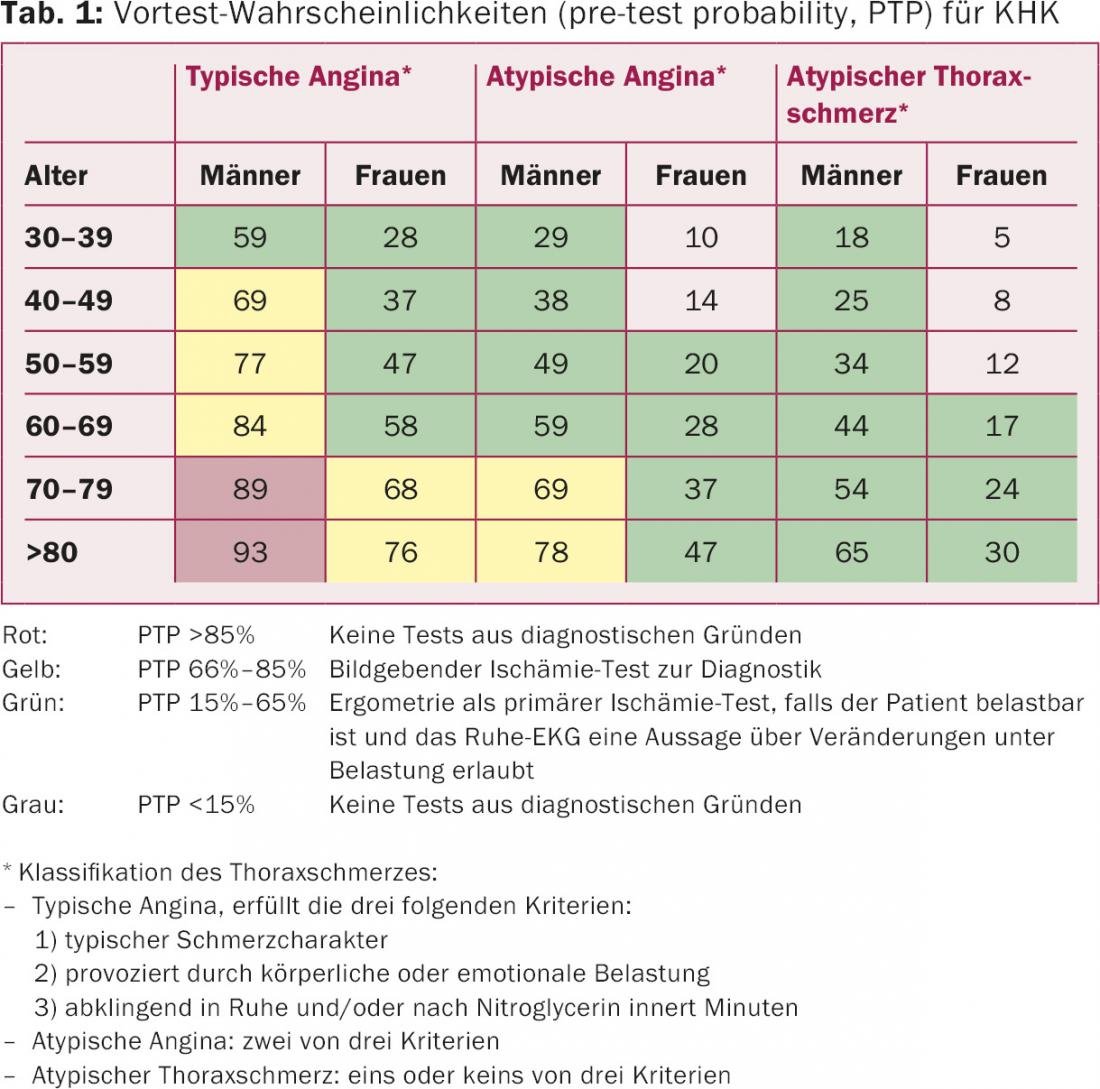
Figure 2 shows the primary choice of test for patients with chest pain and PTP %–85% for CHD according to the current European Society of Cardiology guidelines. When viewed in conjunction with Table 1, it is clear that ergometry may be considered as the primary ischemia test for many patients, this depending on the availability of other modalities such as coronary CT and imaging ischemia tests. Depending on the result of the primary test, further non-invasive or invasive examinations must be followed up.
Ergometry for risk stratification in CHD
Ergometry can be used for risk stratification in both intermediate (%–85%) and high (>85%) PTP, provided that no false conclusions regarding diagnosis are derived.
Ergometry in asymptomatic patients
Screening with instrumental methods regarding subclinical CHD is still not recommended. A detailed discussion of this topic is beyond the scope of this article.
Principle and accuracy of ergometry
Under physical stress, myocardial oxygen consumption increases with increases in heart rate and contractility, leading to provocation of ischemia due to the limited increase in blood flow through a stenosis, which manifests clinically with angina and/or ECG changes (Fig. 1). It is becoming clear that tests measuring inferior perfusion or ischemia-associated LV dysfunction are more sensitive than ergometry. We assume a sensitivity of about 50%, but a specificity of %–90% (for women rather lower).
When can a conclusion be expected from an ergometry?
In order to make conclusive statements about the presence of ischemia based on ergometry, several conditions must be met. First, a patient must be able to exercise circulatory effort on a bicycle ergometer or treadmill, i.e., provoke a maximal increase in heart rate (increase in myocardial oxygen demand) and systolic blood pressure (also markers of an increase in myocardial oxygen demand due to increased contractility).
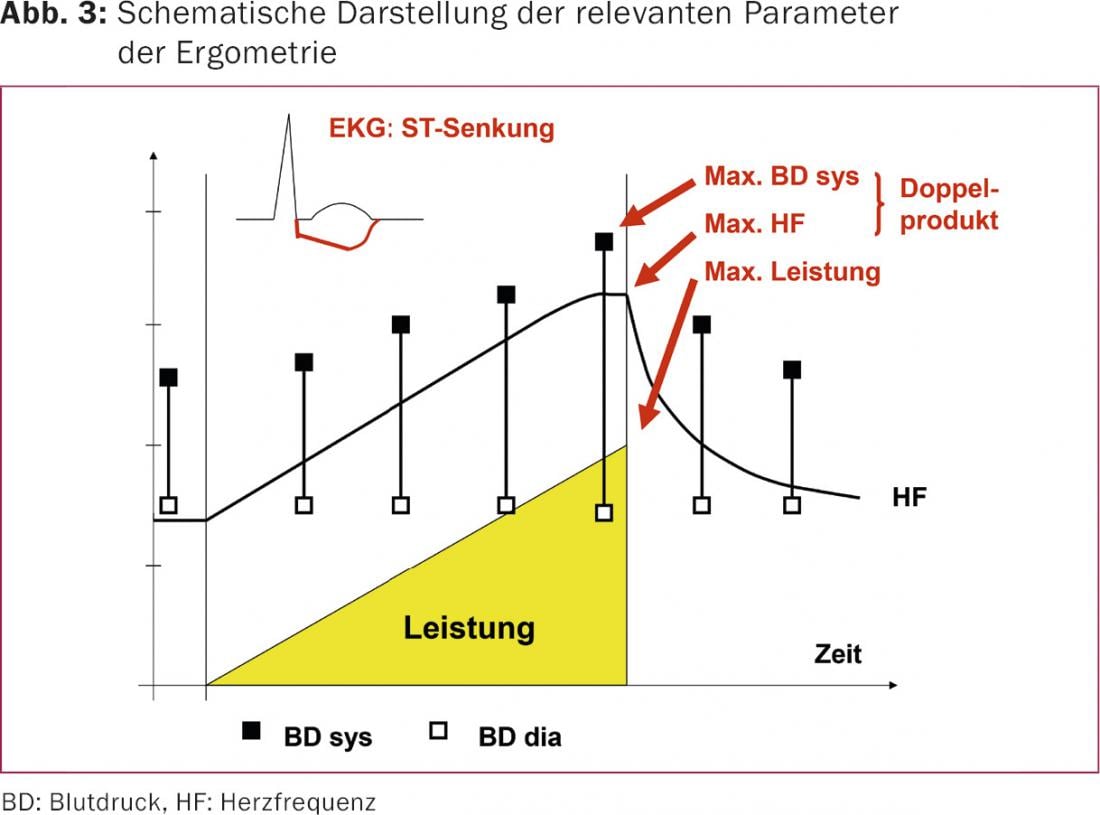
For a conclusive test, an increase in heart rate to at least 85% of the age-adapted heart rate (rule of thumb: 220 minus age in years) or a maximum double product (heart rate × systolic blood pressure; fig. 3) of at least 25 000 mmHg*min-1 is required. If this is not the case, pharmacologic stress with imaging ischemia testing (myocardial perfusion scintigraphy, stress echocardiography, stress MRI) is mandatory. Secondly, the ECG must be usable. In the presence of preexisting ST-segment changes (ST decreases >0.1 mV, typically in the context of left ventricular hypertrophy), left bundle branch block, pacemaker, under digitalis, or in the presence of preexcitation, the ST-segment under stress is not usable, which is why ergometry for diagnostic purposes is not useful or contraindicated in this situation (class III indication). Instead, it is imperative to choose an imaging modality in this case to clarify whether CHD is present.
The practical performance of ergometry cannot be discussed here. In this regard, reference is made to the relevant literature [4].
Interpretation
Ergometry assesses performance, circulatory behavior, symptoms, and ECG. For the diagnosis of CHD, symptoms and ECG are analyzed. Provocation of the symptoms felt in everyday life and leading to clarification under stress supports the diagnosis of CHD. A horizontal or descending ST-segment depression of at least 0.1 mV with ST-segment isoelectric at rest is considered “positive” in the sense of load-dependent myocardial ischemia. Ascending ST depressions are less specific and are usually considered positive only if they are slow ascending depressions of at least 0.15 mV. Ischemia develops slowly, typically does not show up on the ECG until near the end of exercise or even in recovery, and persists over a period of time. Formally, at least three consecutive beats and a stable isoelectric pathway are required; transient ECG changes are suspicious for false positive. In contrast to ST elevation, the localization of ST depression on ECG does not allow any conclusions about the localization of ischemia or coronary stenosis. ST depression is usually most apparent in the chest wall leads V5 and V6, regardless of the location of ischemia.
From a prognostic point of view, performance, circulatory behavior (including heart rate recovery) and ECG response are important (Fig. 4). The better the performance, the better the prognosis. A drop in blood pressure under stress (i.e., a drop in systolic blood pressure under stress below baseline) is an expression of a drop in stroke volume and, therefore, severe ischemia.
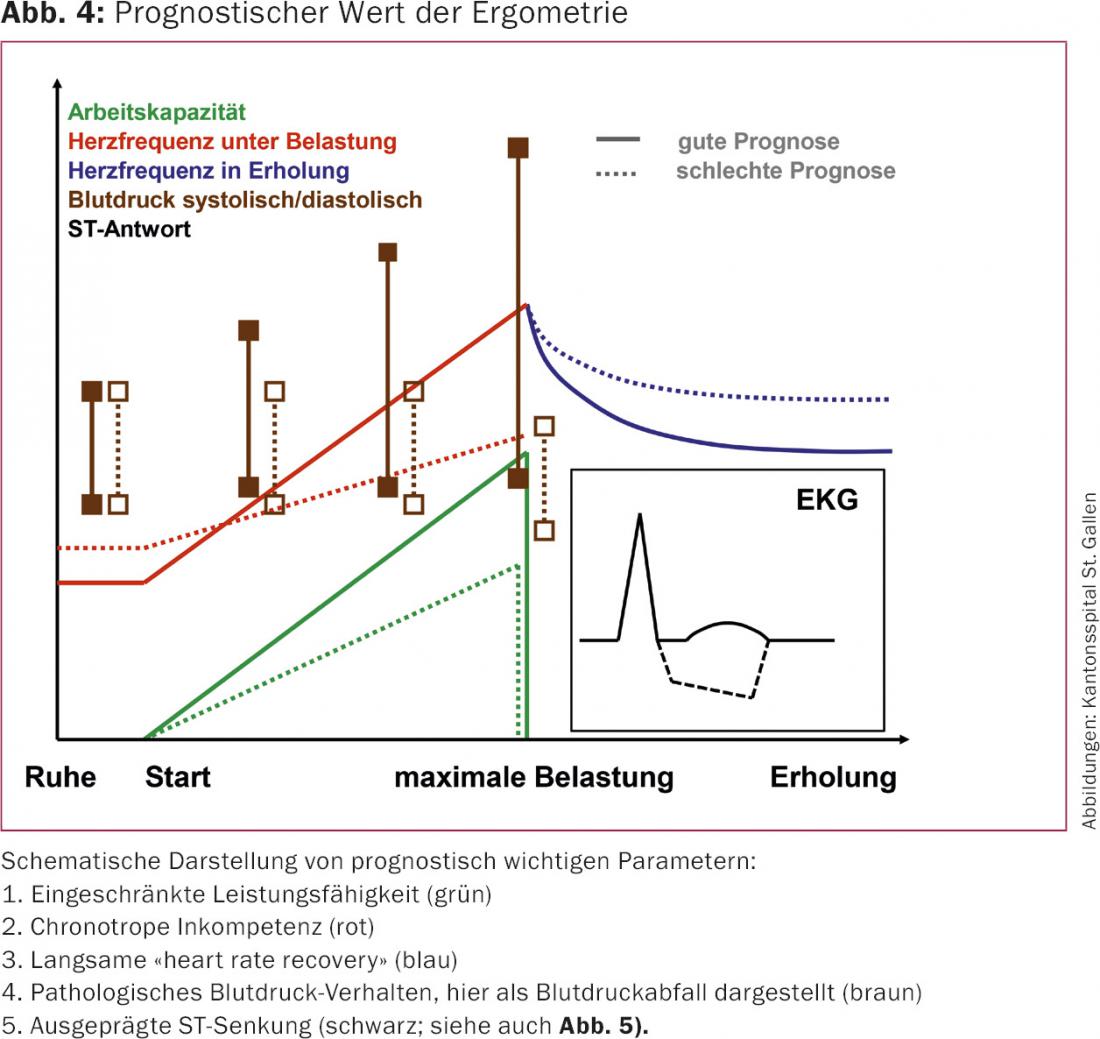
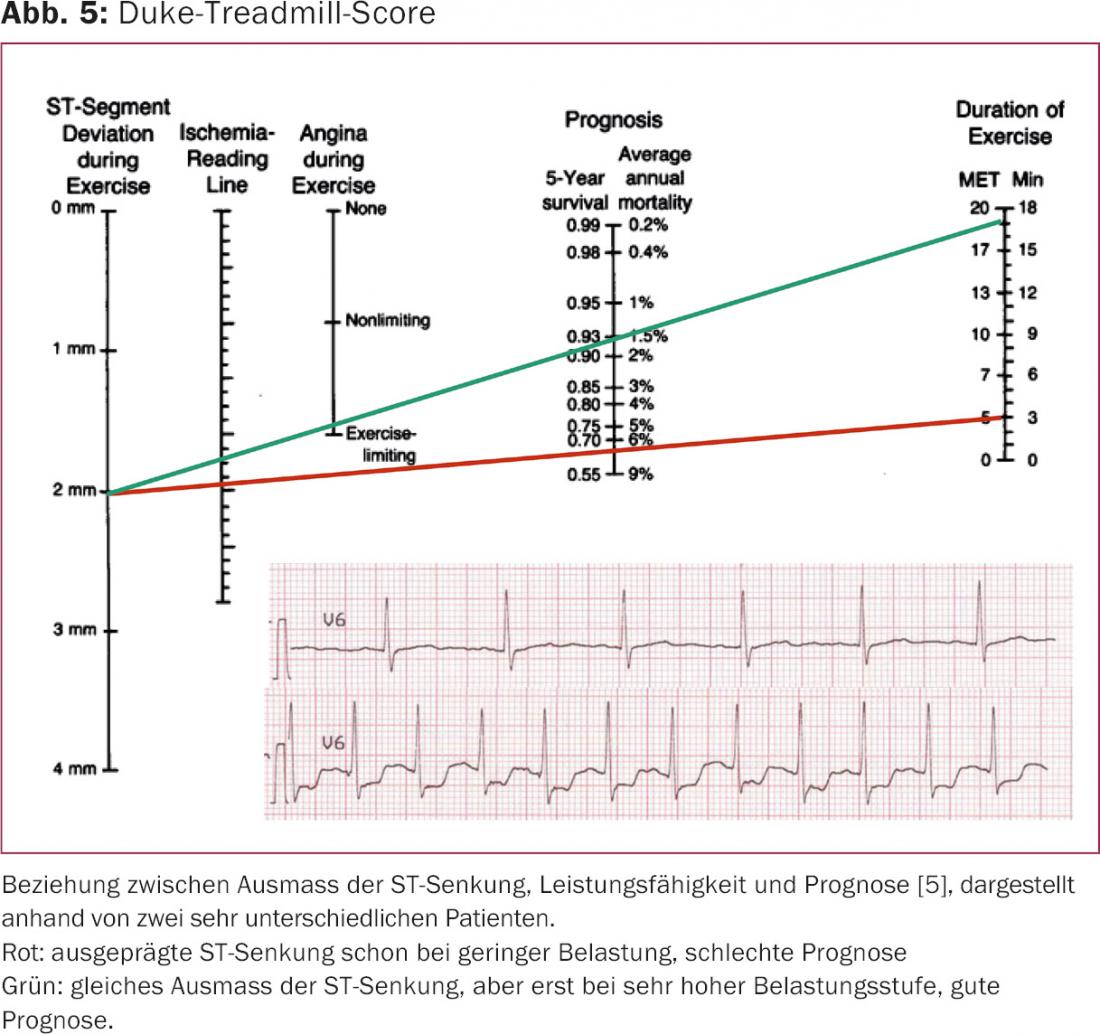
There is also a relationship between timing of onset (even at low exercise and correspondingly poor performance vs. at maximal exercise and good performance), extent of ST depression, and extent of ischemia. This relationship can be quantified by the Duke-Treadmill score, which can also be used semiquantitatively for bicycle ergometry, which is more commonly used in Switzerland (Fig. 5) . Patients at high risk for an event (>3% mortality per year according to Duke-Treadmill-Score, analogous to >10% ischemic myocardium on myocardial perfusion scintigraphy) should be angiographed with a view to revascularization for prognostic reasons.
Literature:
- Maeder MT, Zellweger MJ: [Diagnosis of coronary artery disease – part 1: general approach]. Praxis 2009; 98: 1059-1066.
- Maeder MT, Zellweger MJ: [Diagnosis of coronary artery disease – part 2: exercise electrocardiogram and myocardial perfusion scintigraphy]. Praxis 2009; 98: 1067-1074.
- Montalescot G, Sechtem U, Achenbach S, et al: ESC guidelines on the management of stable coronary artery disease. Eur Heart J 2013; 34: 2949-3003.
- Fletcher GF, Ades PA, Kligfield P, et al: Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation 2013; 128: 873-934.
- Mark DB, Shaw L, Harrell JF Jr, et al: Prognostic value of treadmill exercise score in outpatients with suspected coronary artery disease. N Engl J Med 1991; 325: 849-853.
CARDIOVASC 2016; 15(1): 4-7