Introduction: The clinical distinction between a stroke and an epileptic seizure is not always easy in the emergency situation. However, for the indication of thrombolytic therapy, the distinction between these two clinical pictures is very important. So-called. Early signs of ischemia can often be detected by CT within the first hours after a stroke. However, when these are absent and clinical symptoms are equivocal, perfusion CT can provide additional information. This examination serves to differentiate irreversibly damaged brain tissue, the so-called “infarct core”, from potentially still salvageable, low-perfusion brain tissue, the so-called “penumbra”.
Case report: The 79-year-old patient was referred to our emergency department with an acute onset of consciousness and global aphasia. On admission, the patient appeared alert but unresponsive to prompts or questions. Spontaneous speech was markedly reduced, with the patient expressing only “yes” and “no.” Smacking chewing movements appeared for a short time. All extremities were moved spontaneously. There was a suspected diagnosis of ischemic cerebral infarction or intracerebral hemorrhage. Because of the chewing and smacking movements, which seemed to be orofacial automatisms, we thought of an epileptic event in the sense of a dyscognitive seizure or a focal status epilepticus with persistent symptoms. A metabolic syndrome and hereditary hemochromatosis with phlebotomies last performed in 2008 are worth mentioning from the past medical history.
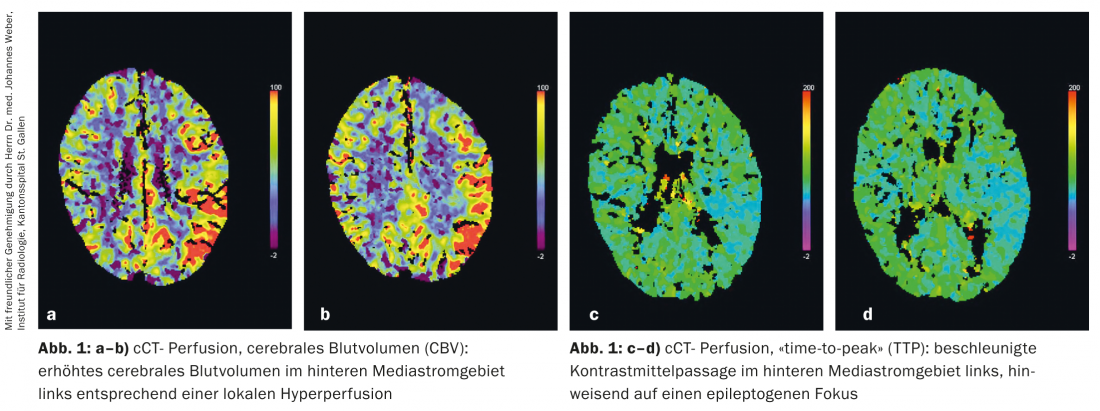
Imaging: We performed cranial computed tomography with CT angiography of the extracranial and intracranial vessels, which showed no hemorrhage, no demarcating ischemia, and no vessel occlusion or occlusion. -stenosis showed. Since systemic thrombolysis was considered due to the clearly identifiable onset of symptoms and in the absence of contraindications, we performed a perfusion CT scan for further differentiation in case of a suspected epileptic seizure event, which showed a focal hyperperfusion of the posterior third of the left mediastinal stroma and could be interpreted in terms of an epileptogenic focus. (Fig. 1).
Course: We then administered 2 mg lorazepam i.v. and a short infusion with a total of 2000 mg levetiracetam. The simultaneously derived electroencephalography confirmed the suspicion of an epileptic event with evidence of a moderately severe general change and rhythmic (2-3/s) “sharp slow waves” with intercalated “spike waves” over the left hemisphere in the sense of status epilepticus (Fig. 2) .

Already on the following day the patient showed clear consciousness with still present but regressing mixed aphasia. Cranial MRI showed signal changes in the left hippocampus, well compatible with cellular edema in the setting of status epilepticus. During the course of the inpatient stay, anticonvulsant therapy with levetiracetam 2×500 mg/day showed no recurrence of epileptic seizures, and the mixed aphasia resolved completely.
Discussion: Computed tomographic brain perfusion measurement can quantitatively measure cerebral blood flow (CBF), cerebral blood volume (CBV), and transit time of the contrast agent in the brain (MTT, “mean-transit-time” or TTP, “time-to-peak”). Patients with stroke usually show reduced cerebral blood flow (CBF) and prolonged contrast rise (TTP). The infarct core also shows reduced cerebral blood volume (CBV), whereas the tissue that has not yet been irreversibly damaged, the penumbra, shows increased cerebral blood volume.
Patients with an epileptic seizure, on the other hand, show hyperperfusion on perfusion CT with increased CBV or increased CBF and shortened TTP.
In cases where it is not possible to distinguish clinically with certainty between a stroke and an epileptic seizure or status epilepticus, perfusion CT provides additional information, especially when it comes to the indication of thrombolytic therapy.
In the present case, a so-called stroke mimic could be detected and the patient could be quickly treated adequately.
Jessica Müller-Westermann, MD
Anita Prochnicki
Johannes Weber, MD
Literature:
- Hedna VS, et al: Seizure Mimicking Stroke: Role of CT Perfusion. J Clin Imging Sci 2012; 2: 32.
- Rother J, et al: CT and MRI in the diagnosis of acute stroke and their role in thrombolysis. Thromb Res 2001; 103; 125-133.
- Reith J, et al: Seizures in acute stroke: Predictors and prognostic significance. The Copenhagen Stroke Study. Stroke 1997; 28: 1585-1589.
InFo Neurology & Psychiatry 2013; 11(6): 42-43.