In general, triggering factors should be avoided in all subtypes of rosacea. Metronidazole, azelaic acid (Germany), and brimonidine are approved for local therapy, and doxycycline in subantimicrobial doses (40 mg/d) is approved for systemic therapy. In rosacea erythemato-teleangiectatica and milder forms of rosacea papulopustulosa, topical therapy is usually sufficient. In severe and therapy-resistant milder forms, complementary systemic therapy should be given. In this case, doxycycline 40 mg/d in combination with topical metronidazole is recommended. Surgical procedures are most effective for rhinophyma. In case of therapy resistance, contraindications or side effects, numerous other therapeutic agents are available, but only off-label.
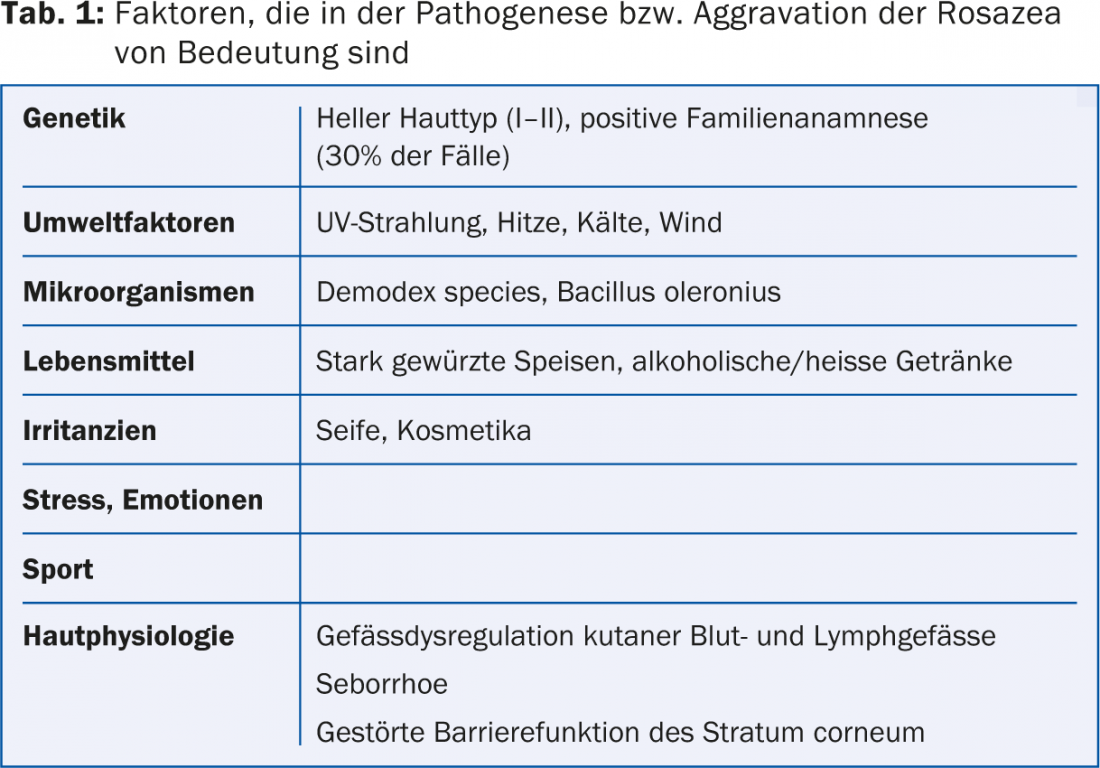
Rosacea is a chronic inflammatory dermatosis common in adults and rare in children, with increased incidence in fair skin types, women and positive family history. An overview of important pathogenetic factors is given in Table 1 [1].
Clinic
Predilection sites are forehead, nose, chin and cheeks, the periorbital region is usually omitted. Less commonly, the chest, neck or capillitium are affected (extrafacial rosacea). Rosacea is divided into several subtypes. In the preliminary stage, there are transient erythema, later telangiectasia and persistent erythema with burning, stinging, itching and dryness (rosacea erythemato-teleangiectatica = subtype I). (Fig. 1). In rosacea papulopustulosa (subtype II), there are also mostly symmetrically arranged non-follicular inflammatory papulopustules (Fig. 2). Glandular hyperplastic rosacea (subtype III) is characterized by seborrhea, connective tissue and sebaceous gland hyperplasia, which may be diffuse or localized as phyme (Fig. 3). Overlap of subtypes is common. In addition, there are several special forms. Lymphedema is particularly typical in the special form of Morbihan’s disease. Up to 60% of patients have eye involvement (ophthalmorosazea), usually in the form of blepharoconjunctivitis with foreign body sensation and dry eye. Skin and eye involvement do not correlate in terms of severity and occur separately in 20% of patients over years. Inflammatory nodules, plaques and induration are typical for rosacea conglobata, in contrast to acne conglobata usually only on the face – comedones are absent. Rosacea fulminans, characterized by inflammatory papulopustules, fluctuating nodules, fistulas, erythema, edema, and seborrhea, occurs only in young women, clustered in and after pregnancy. Unlike acne fulminans, there is usually no fever or arthritis. Granulomatous (lupoid) rosacea, characterized by disseminated, solid, brownish-red papules and nodules, preferably periocular, perioral and on the cheeks, occurs more frequently in dark-skinned individuals.


Therapy
Therapy depends on the subtype or special form and severity of rosacea. Table 2 gives an overview of the therapy options [2,3].
General measures: Individual provoking factors such as aggressive cleaning substances, UV radiation, spicy or hot food, alcohol and temperature changes should be avoided, as well as fatty as well as waterproof cosmetics, soap and soap-containing cleaning agents. Sufficient and consistent UV protection is essential [1].

Topical therapy
Topical therapy is usually sufficient for rosacea erythemato-teleangiectatica and rosacea papulopustulosa. Approved are 0.75% metronidazole (cream, gel, lotion, emulsion), 15% azelaic acid as gel and 0.33% brimonidine as gel. Other topicals can only be used off-label. In addition to the active ingredients, the various bases are important.
Metronidazole: Among the topical agents, metronidazole has been best evaluated and is usually the first choice. Maintenance therapy over a longer period is recommended. It has anti-inflammatory and immunosuppressive effects in rosacea. Efficacy has been demonstrated in several placebo-controlled trials [2]. A novel water-oil microemulsion is currently under development. Metronidazole is equally effective as azelaic acid. In individual cases, type IV sensitization occurred, but the irritant component is less than with azelaic acid.
Azelaic acid: Azelaic acid has anti-inflammatory effects and normalizes keratinization, possibly via suppression of UV-induced RNA expression and release of cytokines Il-1β, Il-6, and TNF-α. It also increases the expression of the anti-inflammatory signaling molecule PPARγ and inhibits the antimicrobial peptides cathelicidin and kallikrein and the activity of a serine protease. It may be more effective than metronidazole on papulopustules [2].
Brimonidine: A 0.33 percent brimonidine gel (Mirvaso®, Galderma) has been approved since 2014 for the treatment of the underlying erythema, which has so far been difficult to influence. The α2-adrenoreceptor agonist has a strong vasoconstrictor, anti-inflammatory and edema-reducing effect. The effect starts after 30 minutes, reaches a maximum after four to six hours and lasts up to twelve hours [4]. Visible telangiectasias and papulopustules do not respond.
Retinoids: adapalene works better than metronidazole on papulopustules but worse on erythema. However, the data on topical retinoids in rosacea are sparse.
Antiscabiosa: Demodex mite density is markedly increased in rosacea papulopustulosa. Antiparasitic substances such as ivermectin, permethrin or benzyl benzoate could therefore also be effective in rosacea. A 1% ivermectin cream has already shown efficacy on inflammatory lesions in studies, and approval is expected in mid-2015 [5]. Permethrin (5%) was also effective in case reports [6]. 10% benzyl benzoate was able to significantly reduce the density of Demodex folliculorum [7].
Calcineurin inhibitors: Tacrolimus and pimecrolimus have anti-inflammatory effects. They are particularly successful in steroid-induced rosacea and erythema in rosacea papulopustulosa [8]. However, the flushing symptoms that often occur as a side effect can aggravate the appearance of rosacea. This relatively expensive group of drugs is therefore not recommended in the presence of well-performing approved alternatives.
Systemic therapy
In addition to local therapy, systemic therapy should be used, especially for severe and therapy-resistant milder forms. Table 3 shows an overview of common systemic therapeutics [1,3].
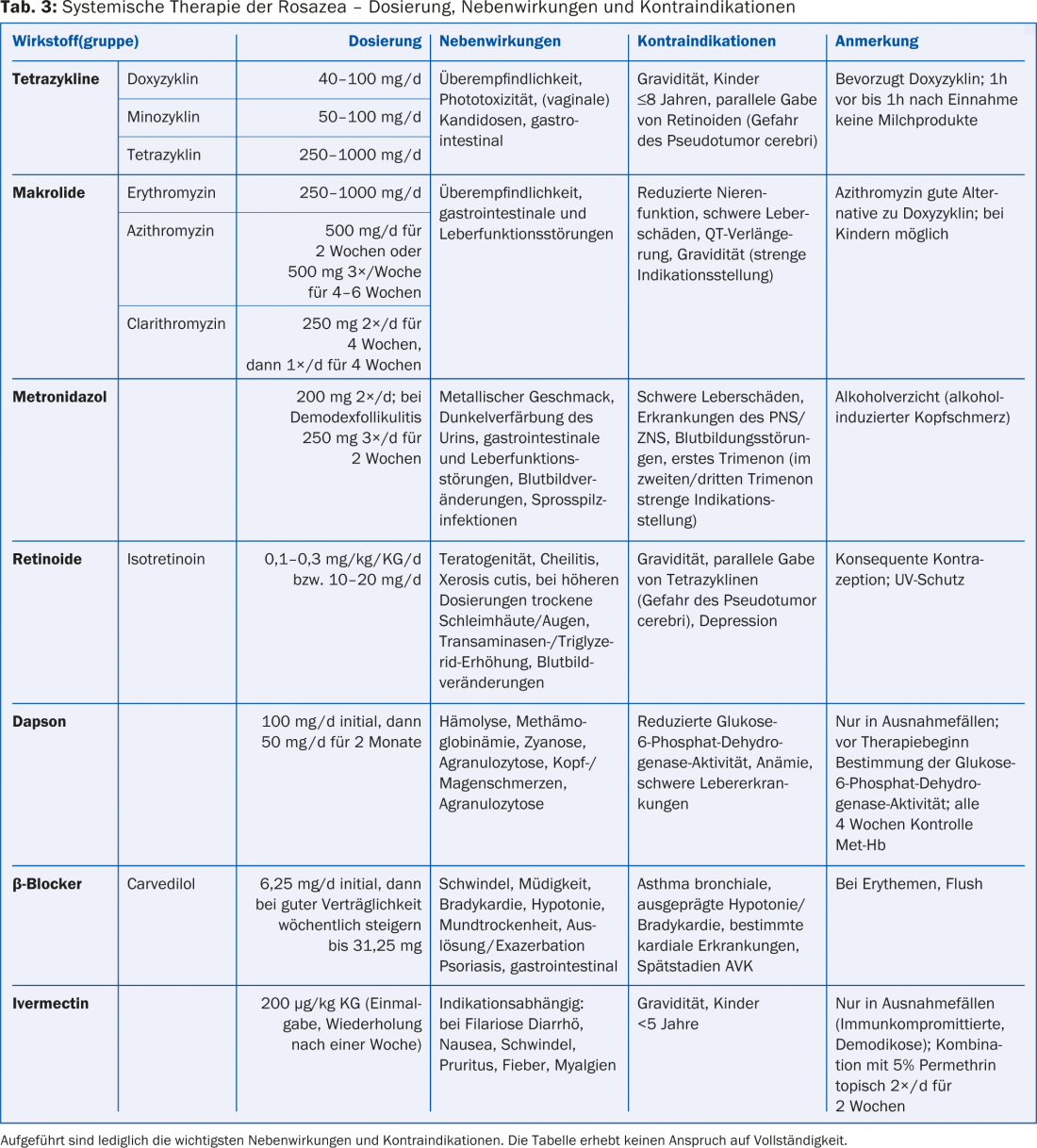
Tetracyclines: First-line systemic therapeutics are usually tetracyclines, particularly doxycycline. To date, the only systemic therapeutic approved is doxycycline in subantimicrobial dosage (40 mg/d) with modified release (Oracea®, Galder-ma), consisting of 30 mg immediate release and 10 mg sustained release components.
Off-label uses include doxycycline at a higher dosage (50-100 mg/d), minocycline (50-100 mg/d), and tetracycline (250-1000 mg/d). Doxycycline and minocycline offer several advantages over the “older” tetracycline, such as longer half-life, better bioavailability, and tolerability, since they must be taken without dairy products but not fasting [9]. Minocycline should no longer be used for first-line therapy of inflammatory dermatoses because of the risk of rare serious side effects [10]. Tetracyclines have an anti-inflammatory effect even at subantimicrobial doses, independent of their antibiotic effect [11], presumably by inhibiting angiogenesis, neutrophil chemotaxis, metalloproteinases, and proinflammatory cytokines [9]. Doxycycline also inhibits the formation of reactive oxygen species and nitric oxide. As a result, connective tissue damage and vasodilation are reduced. These mechanisms may explain the good efficacy of doxycycline at low subantimicrobial doses. Thus, doxycycline is equally effective in rosacea papulopustulosa at low doses (40 mg/d) as at conventional doses (100 mg/d) [11]. Doxycycline (40 mg/d) also works very well in ophthalmorosazea but is not approved [11]. Side effects such as phototoxicity and gastrointestinal discomfort as well as bacterial resistance are significantly lower with subantimicrobial dosing than with conventional [2].
Macrolides: erythromycin, azithromycin, and clarithromycin may be used off-label in contraindications to tetracyclines such as pregnancy, age ≤8 years, or intolerance, and resistance to therapy [12]. Azithromycin and clarithromycin are preferred because of their more favorable side effect profile. Azithromycin and clarithromycin have a similar effect on inflammatory lesions as doxycycline [12]. Ophthalmorosazea also responds rapidly to azithromycin. The usual dose is 500 mg three times a week for four to six weeks.
Metronidazole: met ronidazole 200 mg 2×/d is similarly effective to oxytetracycline 250 mg 2×/d. In particular, demodex folliculitis responds well to metronidazole (250 mg 3×/d for two weeks).
Retinoids: Isotretinoin has anti-inflammatory and immunomodulatory effects, it also reduces the size of sebaceous glands and sebum production. It significantly reduces papulopustules, erythema and telangiectasia and also works well on rhinophyma as well as extrafacial rosacea. A low dosage (0.3 mg/kgKG) is effective and well tolerated [13]. Good own experience exists under therapy with 10 mg isotretinoin daily.
Steroids: glucocorticoids can induce and worsen rosacea. Exacerbation often occurs, especially after steroid discontinuation. They are therefore contraindicated in most cases. Oral steroids in combination with low-dose isotretinoin are useful only in rosacea fulminans and rosacea conglobata [1].
Dapsone: Dapsone may be effective in rosacea granulomatosa and rosacea fulminans. So far, however, there are mainly individual case reports, so it should only be used as an exception.
Beta blockers: beta blockers such as carvedilol cause vasoconstriction and reduce tachycardia and anxiety. Flushing symptoms can also be reduced with carvedilol in gradual dosing up to 25 mg/d. Carvedilol also has antioxidant and anti-inflammatory effects [14]. However, the data are insufficient to make a clear recommendation for beta-blockers.
Ivermectin: In therapy resistance or immunocompromised patients, ivermectin may be considered in exceptional cases.
Physical and surgical therapy
Various types of lasers (pulsed dye laser, copper vapor laser, krypton laser, pulsed neodymium YAG laser, argon laser) as well as the intense pulsed light source are used for rosacea. They work very well on telangiectasias, but less so on areal erythema. CO2 lasers and erbium YAG lasers are suitable for phyme.
For rhinophyma, surgical procedures (dermabrasion, dermashaving) are most effective.
Literature:
- Gauwerky K, et al: J Dtsch Dermatol Ges 2009; 7(11): 996-1003.
- van Zuuren EJ, et al: Br J Dermatol 2011; 165(4):760-781.
- Red List 2014.
- Fowler J, et al: Br J Dermatol 2012; 166(3): 633-641.
- Stein L, et al: J Drugs Dermatol 2014; 13(3): 316-323.
- Kocak M, et al: Dermatology 2002; 205(3): 265-270.
- Pelle MT, Crawford GH, James WD: J Am Acad Dermatol 2004; 51(4): 499-512, quiz 513-514.
- Goldman D: J Am Acad Dermatol 2001; 44(6): 995-998.
- Korting HC, Schollmann C: J Eur Acad Dermatol Venereol 2009; 23(8): 876-882.
- Lebrun-Vignes B, et al: Br J Dermatol 2012; 166(6): 1333-1341.
- Pfeffer I, et al: J Dtsch Dermatol Ges 2011; 9(11):904-907.
- Torresani C, Pavesi A, Manara GC: Int J Dermatol 1997; 36(12): 942-946.
- Gollnick H, et al: J Dtsch Dermatol Ges 2010; 8(7):505-515.
- Hsu CC, Lee JY: J Am Acad Dermatol 2012; 67(3):491-493.
DERMATOLOGIE PRAXIS 2015; 25(1): 18-23











