An update on modern heart failure therapy was given at the DGK Congress in Mannheim. Where are the ARNIs currently located? What is the procedure for special patient requests? There was also news on the problem of hyperkalemia in heart failure treatment.
The study of all heart failure trials was based on the concept of blocking the action of angiotensin 2 via an AT1 antagonist while inhibiting neprilysin, the degrading enzyme of natriuretic peptides produced in the body. The latter relieve the heart and additionally increase renal blood flow. The large PARADIGM-HF trial had shown that therapy with the angiotensin receptor neprilysin inhibitor (ARNI) sacubitril/valsartan significantly reduced clinically relevant endpoints such as cardiovascular death and hospitalization rates due to decompensated heart failure, as well as all-cause mortality, compared to standard intensive therapy.
With the revision of the guidelines for the treatment of chronic heart failure, the combination therapy of sacubitril and valsartan has become the new standard of care for symptomatic systolic heart failure (“heart failure with reduced ejection fraction” or HFrEF). The effects of ARNI therapy begin early, within the first two weeks of therapy initiation, reported Prof. Michael Böhm, MD, of Saarland University Hospital, Homburg, Germany. He gave an update on current heart failure therapy and insights into new (practical) aspects.
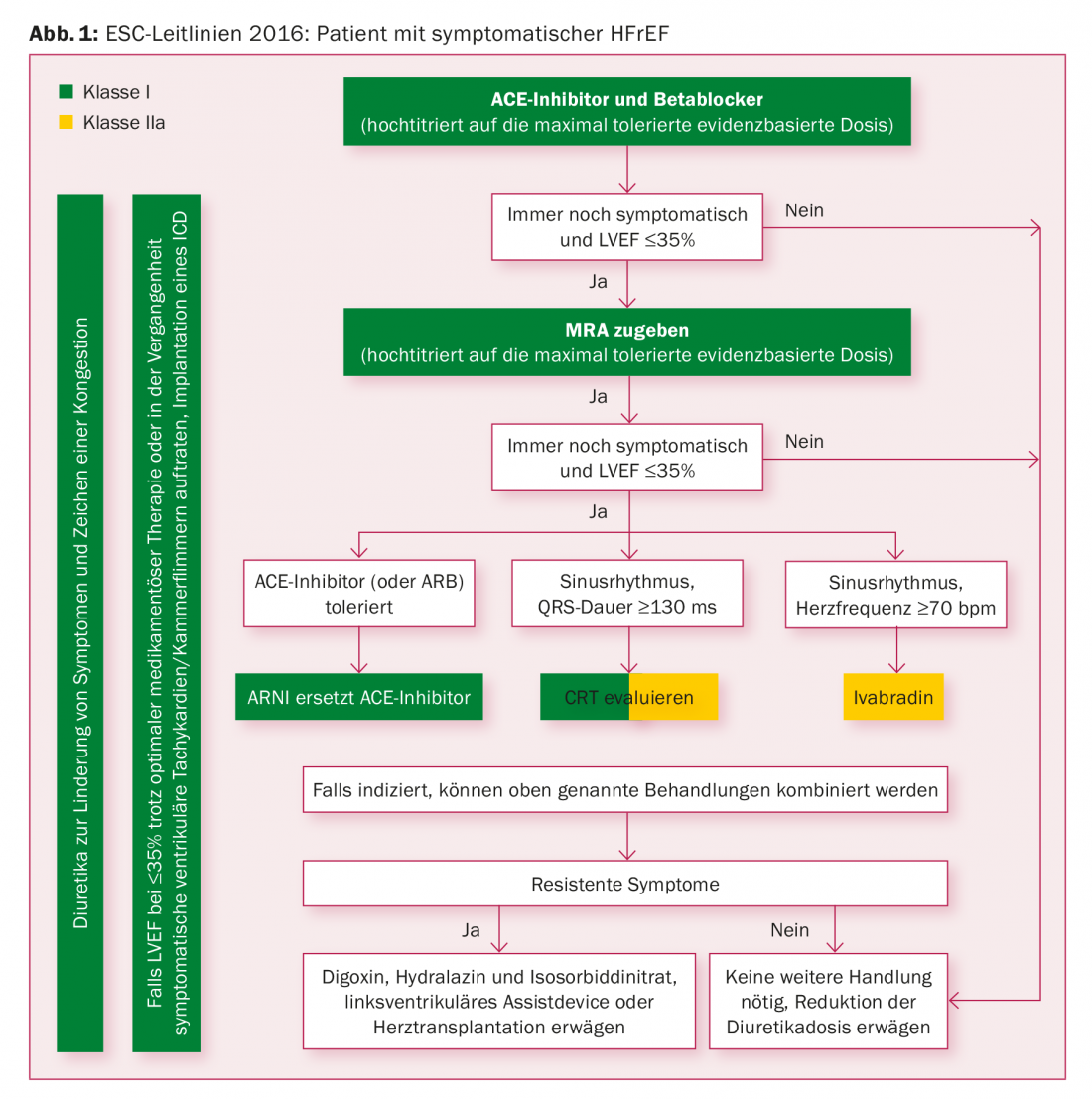
ESC Guidelines 2016
The cornerstones of pharmacotherapy in HFrEF remain ACE inhibitors (AT1 receptor blockers in case of intolerance) and beta-blockers, according to ESC guidelines. If symptoms persist, a mineral corticoid receptor antagonist (MRA) such as spironolactone or eplerenone follows as a third neurohumoral agent in the therapeutic regimen. In the treatment algorithm of the ESC guidelines, the combination of sacubitril/valsartan should replace the ACE inhibitor or AT1 antagonist, provided that the heart failure remains symptomatic – and provided that these substances are tolerated (Fig. 1).
The better equal?
“The principle of ARNI is better than that of (sole) RAAS inhibition,” Prof. Böhm said. ARNI not only inhibits the renin-angiotensin-aldosterone system, but also enhances the activity of vasoactive natriuretic peptides, resulting in a pronounced antihypertensive effect. “Paying attention to blood pressure and the usual exclusion criteria, such as a glomerular filtration rate (GFR) below 30%, all patients with significant heart failure should be switched to sacubitril/valsartan.”
The question of how to deal with the informed patient who develops symptomatic heart failure and desires first-line ARNI therapy, or with special constellations such as hypotension or impaired renal function, has recently been taken up by a published consensus paper, Prof. Böhm reported. In response to the first question, there were specific practical tips on how to treat ACE-naive patients with an ARNI (namely, starting with the lowest dose). In other constellations, the goal is to identify barriers to optimal implementation of heart failure therapy (low blood pressure and/or impaired renal function). Many patients with chronic heart failure and reduced ejection fraction also have low blood pressure. Studies have repeatedly shown that low blood pressure levels in heart failure are associated with increased mortality. However, low blood pressure values in patients with systolic heart failure are not a reason to discontinue sacubitril/valsartan therapy if tolerated. The relative efficacy of sacubitril/valsartan was highest even in the group of patients with the lowest systolic blood pressure values (<110 mmHg). These patients also benefit from a reduction in the risk of death, as suggested by results of an analysis of the PARADIGM-HF trial.
“Enabling therapies”: potassium binders
In practice, the fear of hyperkalemia represents another barrier to optimal therapy, Prof. Böhm said. The substances would not be administered in the recommended dose – with the consequence that their beneficial effect on morbidity and mortality would not or only insufficiently come into effect. New to heart failure therapy is the use of patiromer. The nonabsorbable potassium binder, which binds potassium in exchange for calcium during intestinal transit, is expected to improve the therapeutic breadth of RAAS inhibitors and may be useful for the treatment/prevention of hyperkalemia. Hyperkalemia is a common problem in the management of patients with heart failure, especially in the presence of impaired renal function. Agents that may increase serum potassium include inhibitors of the renin-angiotensin-aldosterone system, AT1 receptor blockers, potassium-sparing diuretics, and mineral corticoid receptor antagonists. With the new potassium binder, it is hoped to help prevent hyperkalemia in the longer term, thus enabling patients with a tendency to elevated potassium levels to receive guideline-based therapy.
Myosin activator Omecamtiv
A therapy with the myosin activator omecamtiv mecarbil is still a dream of the future. As an important motor protein in muscle fibers, myosin is involved in the conversion of chemical energy into force and movement. Together with actin, it forms the contractile unit of the muscle. Omecamtiv mecarbil prolongs the cycle-dependent interaction of myosin with actin, thus also causing a prolongation of systolic duration and an improvement in pumping performance. In a first large international study, the use of myosin activators seemed promising, Prof. Böhm said.
Borrowed from diabetologists:New heart failure drugs?
SGLT2 inhibitors represent a class of agents with favorable effects on cardiovascular event rates and hospitalizations for decompensated heart failure. First there were data on canagliflozin: the substance reduced the likelihood of hospitalization for heart failure in diabetics with cardiovascular risk factors. In the CANVAS trial program, a significant risk reduction for cardiovascular complications (cardiovascular death, myocardial infarction, stroke) of 14% was demonstrated. The relative risk of being hospitalized for heart failure decreased by 33%. A significant risk reduction was achieved especially in patients who already had heart failure.
In 2018, cardiologists are interested in the following questions: Can SGLT2 inhibitors be used in the treatment of heart failure – instead of (as before) in prevention? More importantly, will SGLT2 inhibitors serve as heart failure medications in non-diabetic patients in the future?
Practical tips: Use NT-proBNP for therapy monitoring
BNP and the cleavage product NT-proBNP are biomarkers of heart failure and are used for diagnostics and especially for the assessment of the clinical course. BNP is substrate for neprilysin, which is inhibited by sacubitril during ARNI therapy. Accordingly, the concentration of circulating BNP increases. Under ARNI therapy, only NT-proBNP, but not BNP, is suitable as a follow-up parameter. NT-proBNP is not affected by neprilysin and reflects unchanged severity and progression of heart failure.
Source: Annual Meeting of the DGK, April 4-7, 2018, Mannheim (D).
Further reading:
- Ponikowski P, et al: 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). European Heart Journal 2016 Jul 14; 37(27): 2129-2200.
- Yancy CW, et al: 2017 ACC Expert Consensus Decision Pathway for Optimization of Heart Failure Treatment: Answers to 10 Pivotal Issues About Heart Failure With Reduced Ejection Fraction: A Report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol 2018 Jan 16; 71(2): 201-230.
- Cowie MR, et al: New medicinal products for chronic heart failure: advances in clinical trial design and efficacy assessment. European Journal of Heart Failure 2017; 19: 718-727.
- Packer M: Love of angiotensin-converting enzyme inhibitors in the time of cholera. JACC Heart Fail 2016 Apr 12. pii: S2213-1779(16)30045-2.
- Böhm M, et al: Primum non nocere: the dangers of deferring heart failure therapy. Eur J Heart Fail 2017 Nov; 19(11): 1410-1411.
- Böhm M, et al: Blood Pressure Risk Associations in Heart Failure: True Effects or Inverse Causality? JACC Heart Fail 2017 Nov; 5(11): 820-822.
- Radholm K, et al: Effects of sodium-glucose cotransporter-2 inhibitors on cardiovascular disease, death and safety outcomes in type 2 diabetes – a systematic review. Diabetes Res Clin Pract 2018 Mar 28. pii: S0168-8227(17)31784-9.
- Verma S: The Metabolodiuretic Promise of Sodium-Dependent Glucose Cotransporter 2 Inhibition: The Search for the Sweet Spot in Heart Failure. JAMA Cardiol 2017 Sep 1; 2(9): 939-940.
CARDIOVASC 2018; 17(3): 29-32











