Endoscopic surgery of the thyroid gland can be offered if there is a desire to be scar-free in the visible neck area. After the facelift approach in the hairline (EndoCATS) developed in 2008, the first publication on an almost scarless transfer of the incision into the oral mucosa (TOETVA) followed in 2016. The latest development is a combination of these two procedures, resulting in an optimized scar-free surgical outcome – a breakthrough in thyroid surgery without visible scars.
Thyroid surgery is one of the most common procedures in visceral surgery, with an average of 48 operations in the EU and 39 per 100,000 inhabitants in Switzerland. The Swiss Theodor Emil Kocher (1841-1917) founded modern “physiological surgery” and was the first surgeon in the world to receive the Nobel Prize in Medicine in 1909 for his experimental research on thyroid physiology and thyroid surgery. Kocher is responsible for the current incision between the larynx and the jugulum, which is called Kocher’s collar incision in his honor. Kocher also solved the problem of high perioperative mortality in thyroid surgery. Today, thyroid surgery is among the safest operations with low perioperative mortality and morbidity. Complication rates are comparatively low at 0.8% for permanent recurrent paresis, 0-3% for permanent parathyroid hypofunction, and 1.7% for postoperative hemorrhage requiring revision, although further improvements can be expected here with the use of modern technology.
Treatment goal freedom from scars
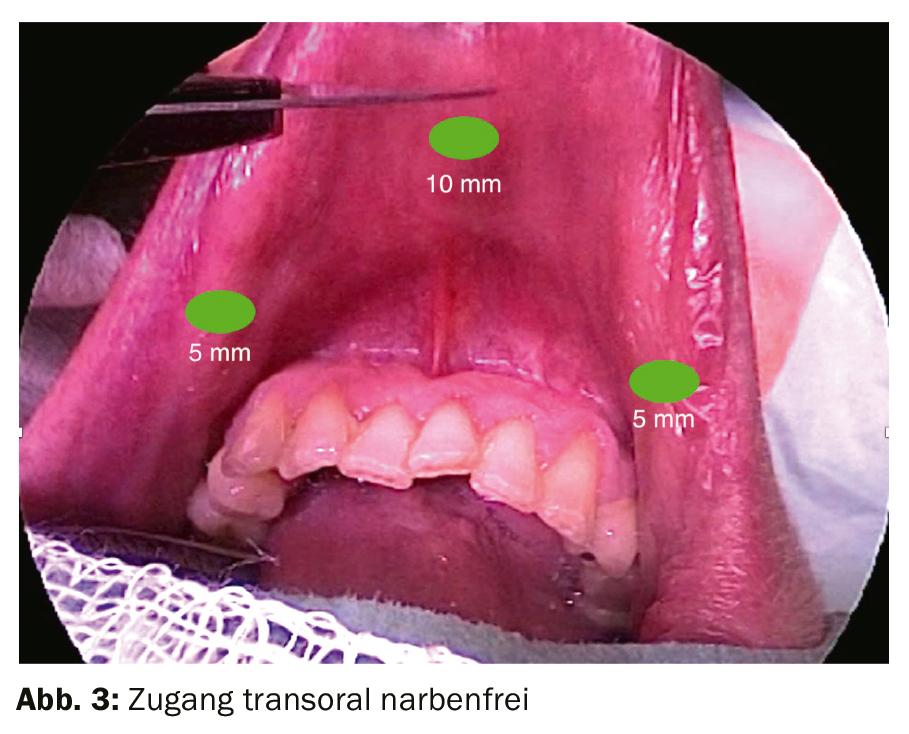
The next step in the development of thyroid surgery at the very low risks is the aesthetic integrity – the absence of scars in the décolleté [1]. By using modern videoendoscopy, Paolo Miccoli – one of the three pioneers [2] of videoendoscopic thyroid surgery – already succeeded in reducing the size of Kocher’s collar incision in 1998. Given the background of unsightly scarring in 4.5-16% [3] especially in young women with moreover mostly benign disease, the development was probably overdue. The so-called MIVAT method was and still is widely used. It is easy to learn and inexpensive. However, the reduction of the scar also has disadvantages. The stretching of the skin required to achieve this results in bulging scars much more frequently [4]. Moreover, the scar is smaller but still exposed (Fig. 1). The solution of relocating the incision to less exposed skin areas was therefore not long in coming. This is the birth of thyroid surgery without visible scars. Ikeda’s first access via the axilla in 2003 is now controversial. More interesting is the facelift approach in the hairline (EndoCATS) by Schardey and Schopf from 2008 (Fig. 2). A particularly promising approach today is the virtually scarless transfer of the incision into the oral mucosa (TOETVA), first published by Anuwong in 2016 and now offered in more than 50 centers (Fig.3).

Optimization through combined methodology
In the still very new transoral technique (TOETVA), three trocars are inserted in the area of the inner side of the lower lip in the so-called vestibulum oris. As a result, the operation can be performed completely endoscopically and ultimately minimally invasively. However, there is a limit at 30 ml flap volume in soft thyroid. Even larger lumps or a very solid organ drastically reduce the volume that can be removed. This is caused by the difficulty of retrieving the gland through the eye of the needle at the tip of the chin. While in the Asian region obviously a different physiognomy limits the salvage less, it is mainly the prominent chin of the Caucasians with simultaneously larger thyroid gland which is responsible for the disproportion in our latitudes. The Karakas, Klein and Schopf team managed to solve this problem in January 2018 when they discussed a recent case. A young patient with a 65 ml thyroid lobe desired surgery without a visible scar due to her occupation. All common methods for thyroid surgery without visible scar were discussed with the patient.
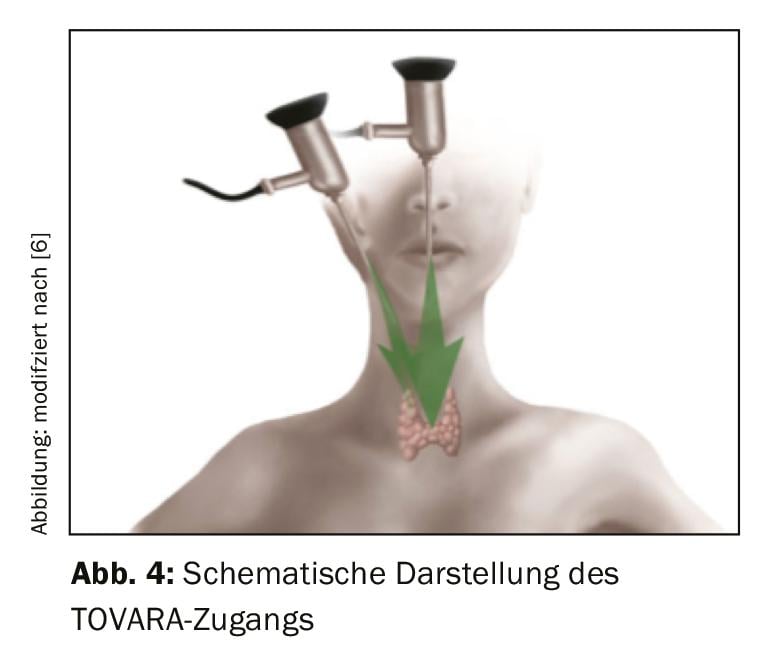
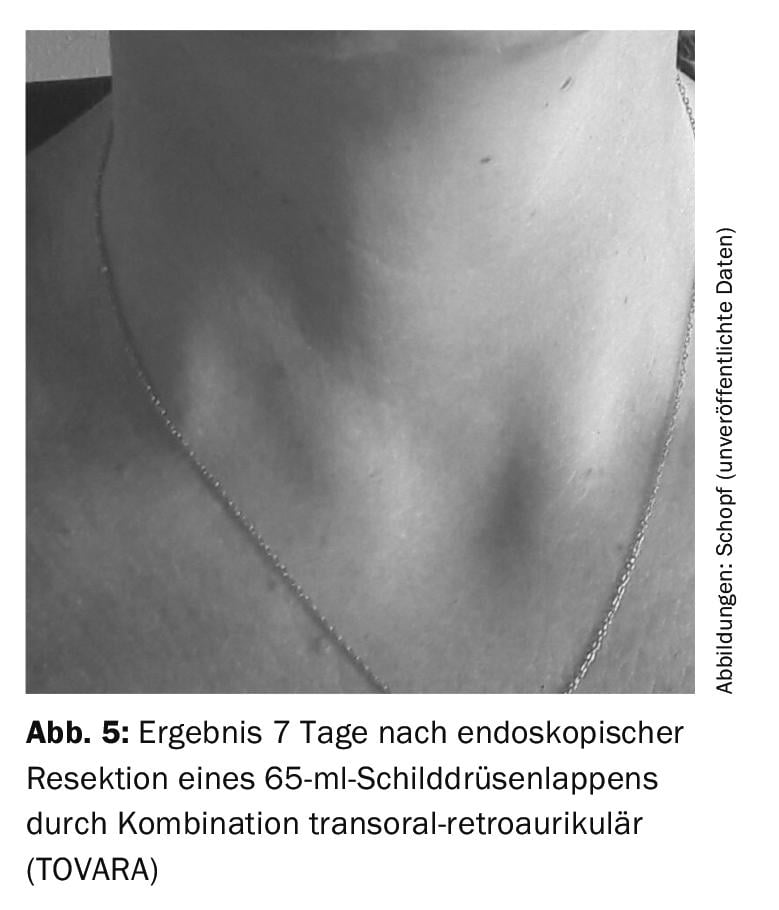
The so-called ABBA operation, over the armpit and breast, was rejected by the patient in principle. Here, both salvage and surgery on the thyroid gland itself would be possible up to about 100 ml. However, the method has recently been discredited by the use of robots in the USA with disastrous results. Moreover, patients shy away from the necessary auxiliary accesses via the breast. Endoscopic surgery via the retroauricular hairline (facelift approach, EndoCATS), on the other hand, allows salvage of even particularly large thyroid glands with excellent visibility of the structures at risk during surgery. Unfortunately, however, the space at surgery is too small to allow uncomplicated dissection of these thyroid lobes. Therefore, the limit is 45 ml per thyroid lobe. The TOETVA transoral surgery, on the other hand, allows the operation of even large thyroid glands, does not require access through the chest and the instruments are at a good angle to each other, which makes the surgeon’s work much easier. (Fig. 4). The disadvantage is that only very small thyroid lobes can be recovered through the eye of the needle on the chin. The innovative idea to solve the patient’s problem was obvious – to combine the ideal procedure for resection (TOETVA) with the best procedure for salvage of even large specimens (EndoCATS). The thyroid lobe could thus be resected transorally and recovered retroauricularly. The combination of the two procedures made the difference, representing a breakthrough in thyroid surgery without visible scars (Fig. 5).
Promising approach
Generally, endoscopic thyroid surgery is offered when there is a desire to be scar-free in the visible neck area. Moreover, there are increasing reports of other potential benefits of endoscopic surgery. In addition to higher patient satisfaction, patients operated on endoscopically complain significantly less of discomfort immediately after surgery [5]. In particular, patients who have undergone endoscopic surgery have fewer swallowing problems in the first year. The reason for this could be the lack of adhesion of the laryngotracheal unit to the platysma, which does not need to be transected during endoscopic surgery. That complete resection is more successful in the removal of differentiated thyroid carcinomas than in classical surgery has only recently been demonstrated on the basis of postoperative thyroglobulin levels. However, the result of the study certainly needs to be corroborated by further studies in other centers. However, long-term results in thyroid malignancy are still lacking.
In the meantime, an international working group has been established and the operation results have been collected centrally. The maximum flap size of 105 ml for TOVARA access to date probably does not represent the limit of the method and it seems that at least one third of all thyroid patients are eligible for such an endoscopic procedure. The combination of transoral surgery and salvage incision appears particularly promising. However, only time will tell if exactly the combination with incision in the hairline or axillary salvage will prevail. Thyroid surgery without visible scars is quite safe nowadays and common all over the world. Although they are not yet part of the standard repertoire of every thyroid center, in the hands of specialized surgeons they are definitely an excellent alternative to the conventional Kocher’s collar incision for many patients.
Literature:
- Arora A, et al: The perception of scar cosmesis following thyroid and parathyroid surgery: A prospective cohort study. International Journal of Surgery 2016; 25: 38-43.
- Miccoli P, et al: Minimally invasive surgery for thyroid small nodules: preliminary report. J Endocrinol Invest 1999; 22(11): 849-851.
- Baker R, Urso-Baiarda F, Linge C, Grobbelaar A: Cutaneous scarring: a clinical review. Dermatol Res Pract 2009: 1-7.
- Dordea M, Aspinall SR: Short and long-term cosmesis of cervical thyroidectomy scars. Ann R Coll Surg Engl 2016; 98(1): 11-7. doi: 10.1308/rcsann.2016.0022. Review.
- Ikeda Y, et al: Clinical Benefits in Endoscopic Thyroidectomy by the Axillary Approach. J Am Coll Surg 2003: 196(2): 189-195.
- Dionigi G, Chai YJ, Tufano RP, et al: Transoral endoscopic thyroidectomy via a vestibular approach: why and how? Endocrine. 2018 Feb;59(2): 275-279.
FAMILY PRACTICE 2019, 14(10): 36-37