Worldwide, strokes are among the leading causes of mortality and morbidity. In a new edition of the S2e guideline on acute therapy of ischemic insults, recommendations are given on the correct procedure also in special situations. New features include aspects of post-stroke delirium or cardiovascular diagnostics and a chapter on gender differences.
The completely revised guideline was published under the auspices of the German Society of Neurology (DGN) e.V. and the German Stroke Society (DSG) [1]. The spokespersons of the guideline steering group, Prof. Dr. med. Martin Köhrmann, Essen, and Prof. Dr. med. Peter A. Ringleb, Heidelberg (D), explain: “Many recommendations have changed since 2012/2015 due to new study data; in addition, various aspects have been newly included. The guidelines now reflect the current state of knowledge” [2].
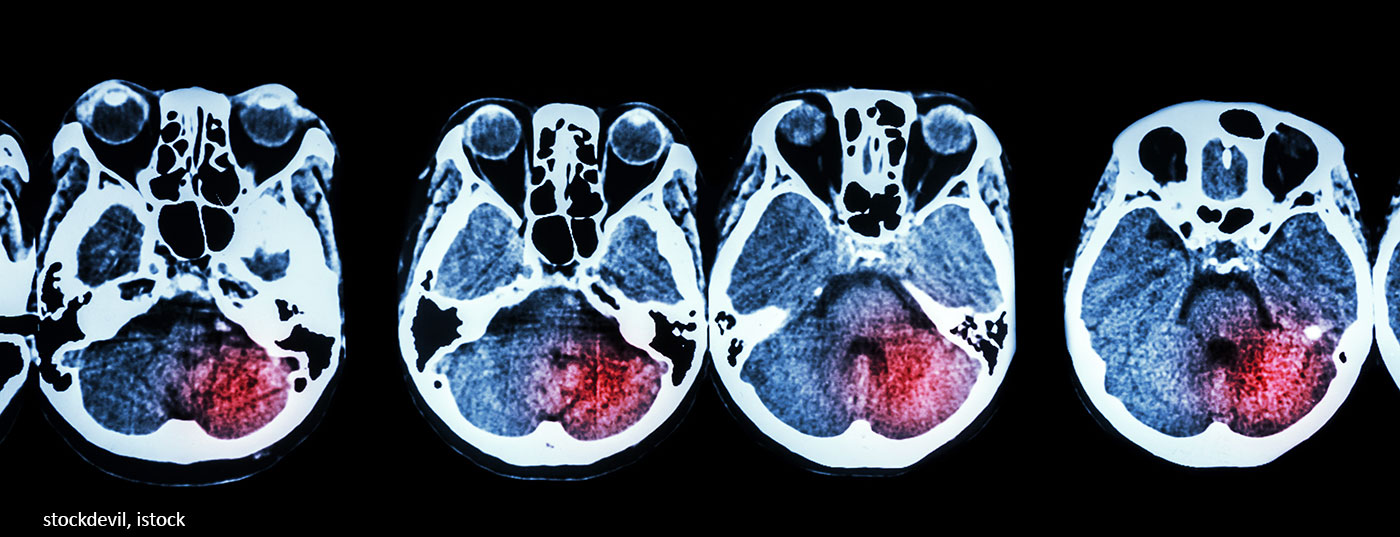
Is it an ischemic or a hemorrhagic insult?
Around 85% of strokes are ischemic in nature – that is, they result from the occlusion or high-grade narrowing of an artery supplying the brain by a blood clot (thrombus or embolism). The less common hemorrhagic strokes are due to cerebral hemorrhage.
In the case of cerebral ischemia, the region of the brain belonging to the blocked vessel is no longer supplied with blood or is supplied with too little blood – there is a lack of oxygen in the brain cells. Therefore, a quick start of treatment is crucial: To avoid brain cell death and permanent damage, perfusion must be restored as soon as possible (recanalization therapy). Treatment is either by drug dissolution of the clot (intravenous thrombolysis) or, in the case of large-vessel occlusions, with a vascular catheter intervention to mechanically remove the clot (interventional thrombectomy) at an appropriate center.
Important adjustments to the guideline at a glance
All patients with an ischemic insult should be treated in a stroke unit.
Immediate cerebral diagnosis with CT or MRI is performed to distinguish between ischemia and hemorrhage and thus to determine the therapeutic procedure. If mechanical thrombectomy is considered, vascular diagnostics (from the aortic arch up) should always be performed as well. If the time interval of 4.5 hours is exceeded on arrival at the hospital, advanced imaging should be performed (e.g., perfusion examination with MRI or CT), as therapeutic steps for reperfusion are still possible even then, depending on the findings.
The standard therapy for systemic thrombolysis is with alteplase (also rt-PA “recombinant tissue-type plasminogen activator”). Tenecteplase could have even better efficacy as a modified molecule. In the EU, this substance has so far only been approved for the treatment of myocardial infarction; the study situation in stroke is not yet uniform. According to the new guideline, tenecteplase should be used outside clinical trials only in individual cases.
So-called post-stroke delirium occurs in up to 48% of patients, depending on the study; average, 26%. In this process, fluctuating disturbances of attention, perception and consciousness develop in a short time, which cannot be explained by the stroke alone. Such delirium is associated with a nearly fivefold increase in mortality, longer hospital stays, and more frequent nursing facility admissions. Despite this frequency and potential consequences of poststroke delirium, new research on it is scarce and therapies are hardly standardized. The guidelines recommend targeted screening with established scores. In addition to treatment with specific medications, it is particularly important to stimulate patients’ reorientation at an early stage (communication, mobilization, glasses, hearing aids, day-night rhythm).
Dual antithrombotic secondary prophylaxis (ASA plus clopidogrel or ticagrelor) should not be routinely given. It may have benefits (reduce nonfatal recurrences) in selected patients after TIA or minor stroke over a 21-30-day period, but possibly at the expense of bleeding risk with no overall change in mortality and little impact on permanent disability and quality of life. Dual antiplatelet therapy should not be used if the risk of bleeding is increased.
A systematic search of databases found no evidence that women with stroke should be treated differently from men. However, variable epidemiological differences between the sexes were evident depending on the study, with women underrepresented in many stroke studies because the age cutoff was often 80.
“Overall, the current guideline represents the knowledge currently available in stroke to ensure the best possible care for those affected. The interdisciplinary nature of this guideline is particularly noteworthy: colleagues from numerous medical disciplines were involved in its preparation, which guarantees a comprehensive view and ensures that all aspects of care were taken into account across disciplines,” explains Prof. Peter Berlit, MD, Secretary General of the DGN.
Literature:
- Ringleb P, et al: Acute Therapy of Ischemic Stroke, S2e Guideline, 2021, www.dgn.org/leitlinien (accessed May 21, 2021).
- “New Completely Revised Guideline on Therapy of Ischemic Stroke,” IDW Information Service Science, May 25, 2021.
- Stroke Center Hirslanden, www.hirslanden.ch/content/dam/klinik-hirslanden (last accessed 09.08.21).
HAUSARZT PRAXIS 2021; 16(8): 22
InFo NEUROLOGY & PSYCHIATRY 2022; 20(2): 29.