Most hand injuries can be evaluated and treated by the primary care provider. It is important to identify injuries that require surgical management.For the common distal radius fracture, an anatomic position is sought in patients younger than 65 years; in patients older than
70 years, the tolerance of the malposition is greater. Most finger joint distortions and dislocations can be treated conservatively.
According to UVG statistics, 724,991 accidents were reported in 2014; 17% of non-occupational accidents and 32% of occupational accidents involved the hand. Open wounds (45%), contusions (15-20%), distortions (15%), and fractures (10%) accounted for the largest proportion of injuries. Significantly less frequent were tendon injuries (3%) and nerve injuries (0.3%). The majority of these lesions, such as contusions and distortions, can be evaluated and treated by the primary care provider. It is necessary to identify the injuries that require surgical treatment. Many injuries can be treated conservatively, but often require splinting and functional follow-up under occupational therapy supervision.
Open injuries
In the case of lacerations, cuts or puncture wounds, the first priority is to avoid infection and to identify lesions of deeper structures. Clinical examination is performed prior to wound exploration, any tendon that may be involved should be selectively tested, and sensitivity should be assessed with two-point discrimination ulnar and radial on the fingertip. Wound cleansing (irrigation, debridement, disinfection, tetanus prophylaxis) and wound inspection may already reveal injury to deeper structures. Local anesthesia and an upper arm tourniquet (blood pressure cuff 250 mmHg) are helpful. Extensor tendon lesions of up to 50% of the cross-section can be left, but flexor tendon lesions, especially in the digital canal region, should be explored by a specialist.
If there is an injury to a deeper structure (or a suspected injury), it can be treated immediately or even early secondarily (tendon and nerve lesions) within seven to ten days. In the meantime, the skin should be closed with a suture. If the wound is contaminated, a drain is inserted, older wounds should be debrided according to the contamination and open post-treatment. The same applies to contaminated puncture and bite wounds.
Wrist injuries
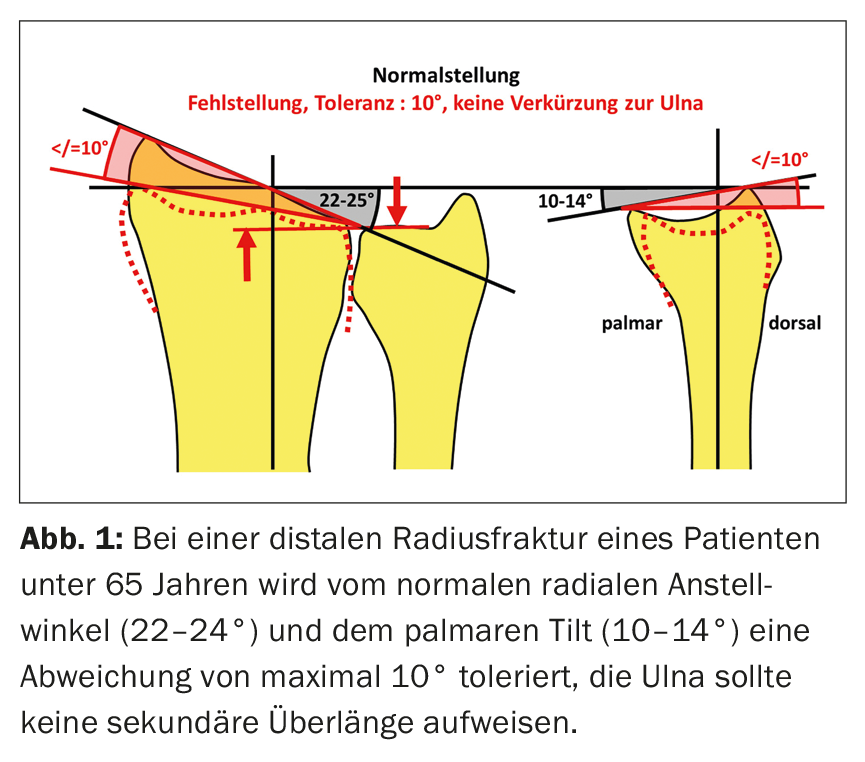
For the most common distal radius fracture, an anatomic position is aimed for in patients under 65 years of age: no shortening of the radius toward the ulna, no steps in the joint, and no more than a 10° dorsal and/or radial tilt (Fig. 1). An x-ray position check is performed after seven to ten days, and a CT is performed for intra-articular fractures. In patients over 65 years of age, the tolerance of malocclusion is much greater. Dorsal tilt up to 40° as well as intra-articular fractures can be treated conservatively without reduction with good results (six weeks forearm cast). The only unstable fractures are the rare palmar angulated, dislocation or forearm fractures (indication for surgery). Vitamin C administration reduces the incidence of complex regional pain syndrome (CRPS 1).
Scaphoid fracture is one of the most commonly missed fractures. In case of pressure pain in the tabatière, dorsal and palmar thereof, as well as provocation pain in wrist extension and radial adduction, a CT is indicated to rule out a scaphoid fracture with certainty. Only the non-displaced fractures in the middle and distal thirds can be treated conservatively (scaphoid plaster for two months, CT control); in all other scaphoid fractures, screw fixation is recommended due to the high rate of pseudarthrosis.
Wrist sprains in which the pain does not improve significantly within two to three weeks should be further clarified with regard to a ligament injury (arthro-MRI). A large proportion of patients are not seen for months, often already with late damage. Repeated clinical examination regarding pain localization and intensity during the course is important. Prior to MRI examination, a conventional radiograph of the wrist ap/lateral is still informative to assess the carpal alignment (Fig. 2).

Finger joint injuries
Finger joint distortions can be treated conservatively, with some exceptions, as long as timely and adequate care is provided (splints, occupational therapy).
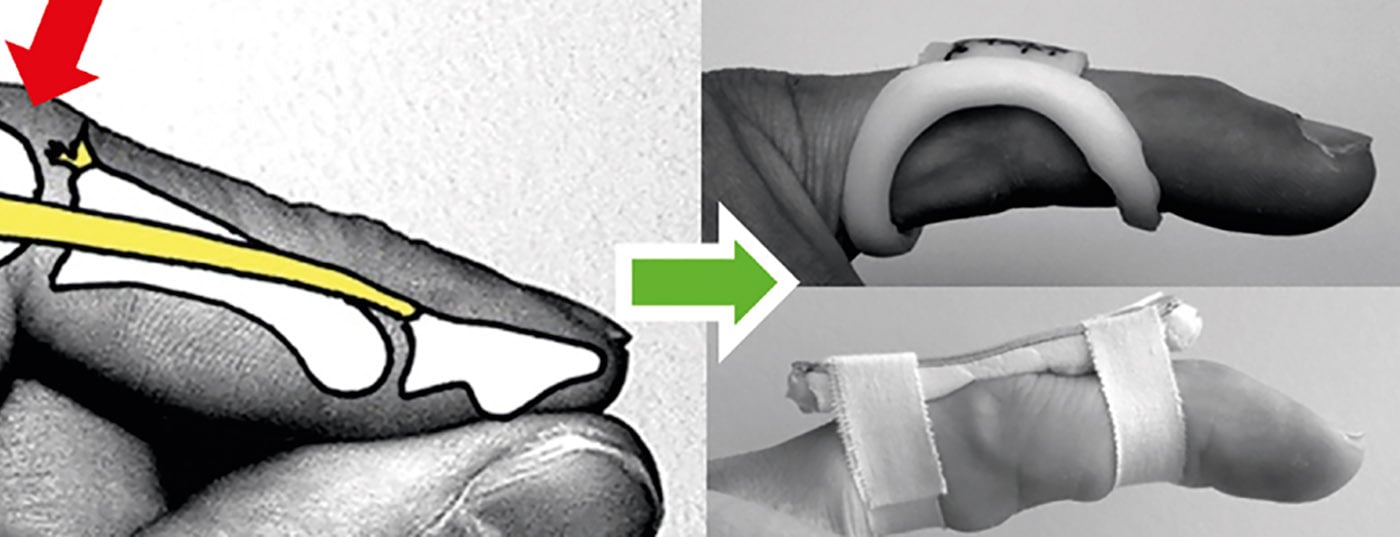
At the DIP joint, the Mallet lesion (closed extensor tendon rupture) is probably the most common injury with clinically impressive hanging distal phalanx (active extensor failure). Treatment is with a dorsal aluminum or a stack splint (occupational therapy) for consistently eight to ten weeks (Fig. 3). An osseous extensor tendon avulsion (X-ray) is treated identically. There is an indication for surgery if the joint is involved by more than one third (relative) or if there is subluxation (absolute).

At the PIP joint, ruptures of the collateral ligaments (clinical testing of stability in 10° flexion) or avulsion of the palmar plate (clinical hyperextensibility) are most common. These injuries are treated conservatively. Radiological clarification includes an exact ap and lateral image to rule out an impression fracture, which is an indication for surgery (CT in case of doubt). The injured finger is splinted to the neighboring finger (taping, figure-8 loop) and the joint is mobilized immediately. Follow-up treatment is under occupational therapy supervision, often months of swelling are normal. The much rarer extensor tendon injury at the PIP joint, which can lead to buttonhole deformity if left untreated, is initially difficult to diagnose clinically (see a specialist if in doubt). Treatment is with a PIP stretch splint for six weeks consistently (occupational therapy).
Luxations: Dislocations in the DIP joint are reduced under traction; with normal extension, flexion, and x-ray, follow-up is functional. PIP joint dislocation to the dorsal (rupture of the palmar plate and collateral ligament) is reduced under local anesthesia and followed up with a stretch-stop splint and/or taping under occupational therapy supervision. The less common palmar dislocation of the PIP joint (rupture of the extensor tendon) is treated with a PIP extension brace and occupational therapy. This is always provided that no fracture is visible after reduction and the joint is centered.
A special situation exists with ulnar collateral ligament injury at the MP joint of the thumb (ski thumb). If the ligament is torn distally, the adductor aponeurosis can slip under it and fold it over proximally, so that healing is not possible conservatively (Stener lesion). If there is ulnar instability in the MP joint (unfolding in 20° flexion laterally different or >35°), this lesion must be ruled out with ultrasound/MRI, otherwise there is an indication for surgery. Otherwise, the injury can be treated conservatively with a short thumb sleeve for six weeks.
Fresh lateral ligament ruptures of the MP joints of the long fingers can be treated conservatively. During the clinical examination, care must be taken to ensure that the stability test is performed in flexion (80°). In cases of instability, i.e., increased opening compared to the opposite side, treatment is with a figure-8 loop or taping to the adjacent finger for six weeks. Apart from short-term immobilization due to pain, immediate movement, controlled by occupational therapy, is indicated.
Finger fractures
Nail ring fractures are usually treated conservatively with a short DIP finger splint, and weight-bearing can be increased if pressure is insensitive. Radiological consolidation usually takes a long time. Dislocated end-member fractures with nail dislocation or subungual hematoma >50% must be reduced, the nail bed sutured and splinted (surgical indication).
Intra-articular fractures of all finger joints are treated conservatively only if they are not dislocated. They must be monitored closely radiologically (after five and ten days) and, if unclear, clarified by CT with regard to a possible impression fracture.
Midlimb and proximal limb fractures are often unstable and also require close follow-up. A malposition in the extension/flexion plane of 10° is permissible. Axis deviations in all other planes should not be tolerated. A rotation defect can usually only be assessed clinically with different flexion positions of the interphalangeal joints (note the plane of the fingernails).
Metacarpal fractures: shaft fractures of metacarpal IV or V with a flexion position up to a maximum of 20° can be treated conservatively. On the index and middle finger, significantly less malposition is tolerated and stabilization is preferred. In subcapital metacarpal V fracture (Boxer fracture), malalignment up to 50° in flexion may be allowed; in manual work or for cosmetic reasons (hump formation over the dorsum of the hand), the upper limit should be set at 20-30°. A special situation exists with fractures of the base of metacarpal I, as these are almost always unstable and dislocate due to the pull of the abductor pollicis longus muscle. Bennett (partial articular), Rolando (multiple fragment complete articular) and Winterstein (extraarticular) fractures should therefore practically always be treated surgically.
Carpal fractures are often not assessable on conventional radiographs (not visible, dislocation not assessable) and should be ruled out with CT or MRI if suspected.
Further reading:
- Juon BH, et al: Treatment of open hand injuries: does timing of surgery matter? A single-center prospective analysis. J Plast Surg Hand Surg 2014; 48(5): 330-333.
- Arora R, et al: A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am 2011; 93(23): 2146-2153.
- Malay S, Chung KC: Testing the validity of preventing complex regional pain syndrome with vitamin C after distal radius fracture. J Hand Surg Am 2014; 39(11): 2251-2257.
- Weber P, Segmüller H: Non-surgical treatment of mallet finger fractures involving more than one third of the joint surface: 10 cases. Handchir Microchir Plast Chir 2008; 40(3): 145-148.
HAUSARZT PRAXIS 2015; 10(8): 10-13