Rosacea is a common inflammatory dermatosis primarily affecting the face. Primary symptoms are redness and telangiectases in the cheek and nose area, the treatment of which should be included in the overall therapy concept from the outset. Lasers can be used for this purpose.
Rosacea is a common, inflammatory dermatosis that primarily affects the face and usually begins in middle adulthood. A chronic and relapsing course is typical [1]. While the first symptoms represent fleeting redness on the face that already greatly disturbs patients, these increasingly persist over time. Most often, telangiectasias form in the cheek and nose area. These are a common reason for sufferers to visit the dermatologist with a request for laser treatment (Fig. 1).

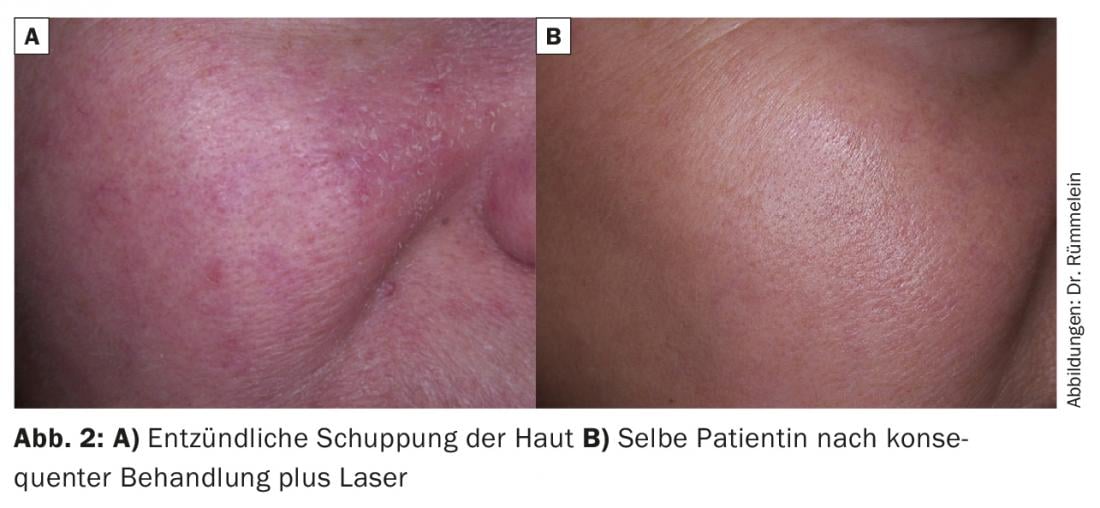
As it progresses, papules and papulopustules are added (grade II). Lymphedema and diffuse hyperplasia of the connective tissue and sebaceous glands are another characteristic, although not obligatory. In their most severe form, rhinophyma, these can cause a sometimes grotesque proliferation of the nose. Such severe manifestations are rare, but coarsening of the skin appearance and inflammatory scaling are more common (Fig. 2).
Although rosacea may look like acne at first glance, comedones are completely absent as a diagnostic criterion.
Epidemiology
The prevalence of rosacea varies considerably from country to country: in Germany, a cohort study of 90,880 individuals found a prevalence of 2.3% [2], whereas a study conducted in Sweden found a value of 10% [3].
In 80% of cases, the diagnosis of rosacea is made at the age of 30 years or later [4].
The Celtic fair-skinned type (Fitzpatrick I-II) is more commonly affected compared with the southern dark-skinned type, although the disease can also occur in patients with skin type IV-V [5].
Ocular involvement is observed in approximately 20% of patients (3-58%, depending on the study) [6].
Pathogenesis
The causes of this presumably multifactorial clinical picture are still not conclusively clarified. Genetics, immunological, neurological and inflammatory causes, UV radiation, dysregulation of blood vessels and possibly lymphatic vessels seem to play a role [7,8]. Demodex mites are seen as a cofactor and are therefore also included in the treatment.
Cathelicidins are antimicrobial peptides produced in the skin. Human cathelicidin peptide LL-37 has antibiotic activity, immunomodulatory and angiogenic effects. In rosacea, the production and activation of cathelicidin peptides is impaired [9].
Toll-like receptor-2 (TLR2) is expressed at increased levels in rosacea patients [10].
Demodex mites are thought to be a possible triggering factor of the inflammatory response in rosacea. Therapeutic reduction of Demodex mites in the skin in rosacea also reduces inflammation [11].
The special forms such as gram-negative rosacea, steroid rosacea, lupoid rosacea and Morbihan’s disease will not be discussed here.
Therapy
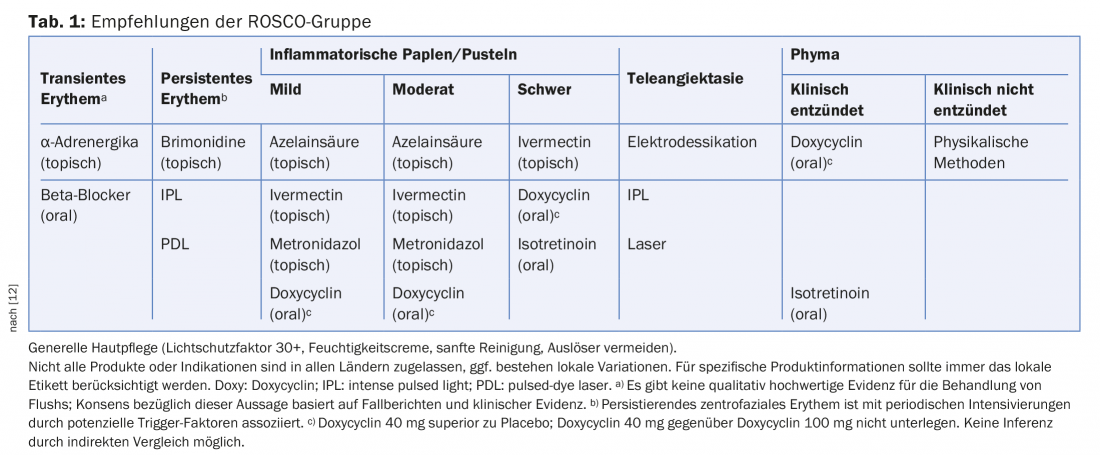
As far as therapy is concerned, the results of the ROSCO group (Global Rosacea Consensus) published in 2017 [12] should be brought into focus. In my opinion, they provide a helpful orientation for every dermatologist (Tab. 1).
The goal for the therapy of rosacea is – as with any therapy – to gain the patient’s compliance.
We all know how distressing the symptom of redness is for many patients. This should therefore always be included in the treatment. The following measures are available for this purpose:
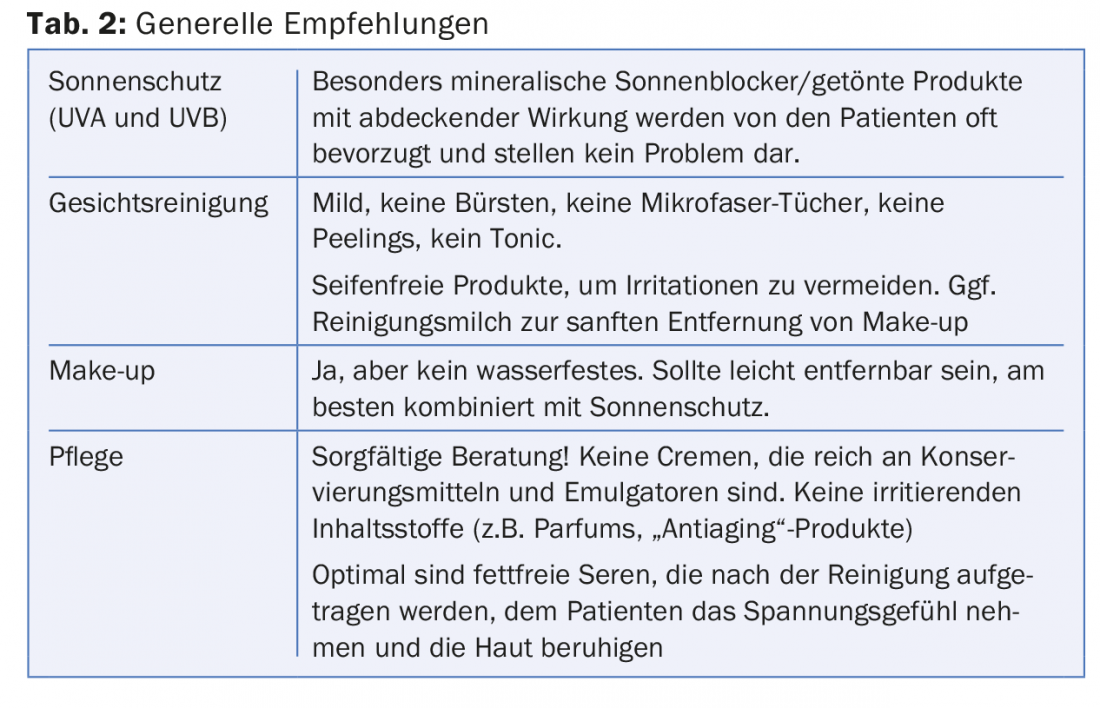
- Covering with suitable make-up (Tab. 2): Men and women have fundamentally different needs here. While female patients with rosacea should switch to non-waterproof products with sunscreen, most men do not want makeup but are grateful for sunscreen products with greenish pigments that can also conceal redness via the principle of complementary colors.
- Brimonidine-containing creams are a good idea in theory, but are unfortunately very difficult to use in a cosmetically pleasing way because blotchy results due to uneven application or unnaturally light skin patterns do not produce an aesthetically satisfactory result. I have also been able to observe paradoxical effects in my patient collective (Fig. 3).
- Efficient and desired by many patients are laser and IPL treatments. A distinction must be made here as to whether individual telangiectasias or diffuse redness is to be removed. For single telangiectasias, a KTP laser (532 nm, green light) or a diode laser (800-980 nm) is suitable, which are usually offered with fine pen-like probes and make a very simple treatment possible. Less elegant, significantly more painful and associated with a risk of scarring, this treatment can also be performed with an electrocautery. However, from my point of view, this belongs to medical history. Also suitable are long-pulsed alexandrite and Nd:YAG lasers. With the Nd:YAG laser, caution is advised, especially in the nasal region, as non-specific tissue heating can lead to permanent dent formation (Fig. 4).
- In case of diffuse redness, the entire affected area is treated. Various systems can also be used here. It is important to ensure strict UV abstinence before treatment, as vascular lasers are also absorbed into melanin (Fig. 5) and this effect, which is not desired here, can lead to burns and possibly scarring (Fig. 6). The use of IPL devices with handpieces covering a broad spectrum can be recommended. Ideally, they cover the two hemoglobin peaks (500-670 nm and 870-1200 nm) (Fig. 5).

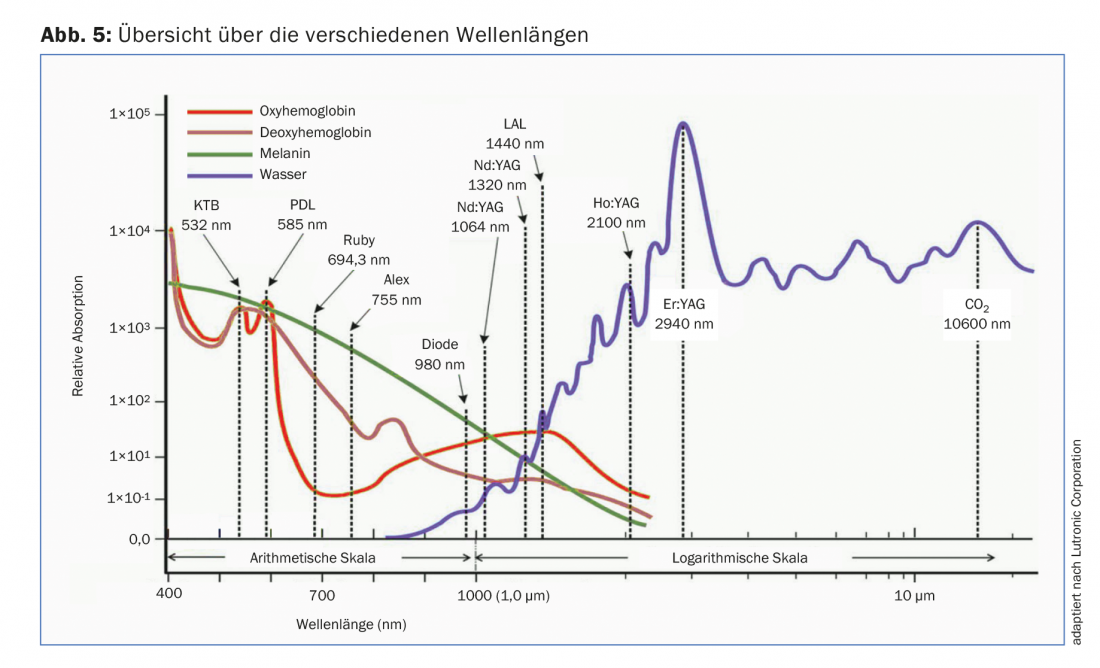

The penetration depth of the selected laser is also important in the selection process. While a KTP (532 nm) can only reach superficial vessels, a diode laser (800-980 nm) penetrates deeper.
Dye lasers (PDL, 585 to 595 nm, red light) are gentle to the surrounding skin on the one hand, but leave the typical, livid bruises shown in Figure 7 for a few days, which are caused by the rupture of the fine vessels.

Oral therapy
The main focus of oral therapy with doxycycline 40 mg is its anti-inflammatory effect, and plasma levels are below the antimicrobially active threshold for most germs. Doxycycline 40 mg is not inferior to doxycycline 100 mg, so the higher dosage should no longer be administered.
It is basically a long-term treatment of three to six months or longer. Caution should be exercised in patients with hepatic impairment or concomitant use of potentially hepatotoxic drugs. Because of the risk of esophageal irritation/ulceration, the preparation should be taken with plenty of water and in an upright position. Since the absorption of doxycycline is inhibited by the simultaneous ingestion of bivalent or trivalent ions such as aluminum, zinc, calcium, and magnesium, as well as some drugs, these should be ingested no earlier than 2-3 hours after taking doxycycline. Thus, the medication history should be carefully taken. The patient must be advised to avoid milk and milk-containing foods as well as calcium-containing fruit juices in connection with the intake.
Summary
The ROSCO consensus provides a good, scientifically based overview of treatment options. Selection should be made according to the symptoms experienced by the individual patient. The accompanying skin care should not be underestimated. Here, too, medical expertise is in demand. For good patient compliance, the patient’s esthetic desires must be respected. An important measure is the treatment of redness and telangiectasia. This should be treated in a timely manner with laser and IPL techniques by specialized practitioners. The necessary knowledge can be acquired, if applicable, with the Type IV Skin Laser Capability Credential Training Program for Vascular Lesions (www.laserkommission.ch; www.smartaging-swiss.academy).
Take-Home Messages
- Rosacea is a chronic inflammatory skin disease with typical manifestation around the age of 30.
- Primary symptoms are redness and telangiectases in the cheek and nose area.
- Presumably, the development of rosacea has multifactorial reasons.
- The exact pathogenesis is not yet clear.
- Sun protection and appropriate skin care form the basis of the therapy. The treatment of redness and telangiectases should be included in the overall concept from the outset. Lasers can be used for this purpose.
Literature:
- Reinholz M, et al: S1 Guideline: Rosacea. AWMF online. Guideline of the German Dermatological Society www.awmf.org/leitlinien/detail/II/o13-065.html
- Augustin M, et al: Prevalence of skin lesions and need for treatment in a cohort of 90 880 workers. Br J Dermatol 2011; 165: 865-873.
- Berg M, Liden S: An epidemiological study of rosacea. Acta Derm Venereol 1989; 69: 419-423.
- Spoendlin J, Voegel JJ, et al: A study on the epidemiology of rosacea in the UK. Br J Dermatol 2012; 167: 598-605.
- Alexis AF: Rosacea in patients with skin of color: uncommon but not rare. Cutis 2010; 86: 60-62.
- Akpek EK, et al: Ocular rosacea: patient characteristics and follow-up. Ophthalmology 1997; 104: 1863-1867.
- Cribier B: Pathophysiology of rosacea: redness, telangiectasia, and rosacea. Ann Dermatol Venereol 2011; 138 Suppl 3: S184-91.
- Schwab VD, et al: Neurovascular and neuroimmune aspects in the pathophysiology of rosacea. J Investig Dermatol Symp Proc 2011; 15: 53-62.
- Yamasaki K, Gallo RL: The molecular pathology of rosacea. J Dermatol Sci 2009; 55: 77-81.
- Yamasaki K, et al: TLR2 expression is increased in rosacea and stimulates enhanced serine protease production by keratinocytes. J Invest Dermatol 2011; 131: 688-697.
- Kocak M, et al: Permethrin 5% cream versus metronidazole 0.75% gel for the treatment of papulopustular rosacea. A randomized double-blind placebo-controlled study. Dermatology 2002; 205: 265-270.
- Schaller M, et al: Rosacea treatment update: recommendations from the global ROSacea COnsensus (ROSCO) Panel. Br J Dermatol 2017; 176(2): 465-471.
DERMATOLOGIE PRAXIS 2018; 28(1): 28-32











