Case report: In 2009, the then 32-year-old patient underwent her first brain tumor surgery (glioblastoma WHO °IV, DD: anaplastic astrocytoma WHO °III, Mib-1 10%). The recommended adjuvant treatment [1] was rejected due to an existing pregnancy. In 2011, recurrent surgery with adjuvant radiation (total dose 60 Gy) was performed. Histologically, the classification of the tumor remained equivocal. The indication for chemotherapy was discussed and recommended on an interdisciplinary basis, but was not performed at the patient’s request. Another surgery was performed for recurrence in December 2014 (secondary glioblastoma WHO °IV, IDH1 positive, MGMT methylated, Mib-1 70%). Adjuvant radio-chemotherapy with adapted radiation volume was planned but discontinued after three irradiations (total dose 6 Gy) at the patient’s request, and chemotherapy was again rejected.
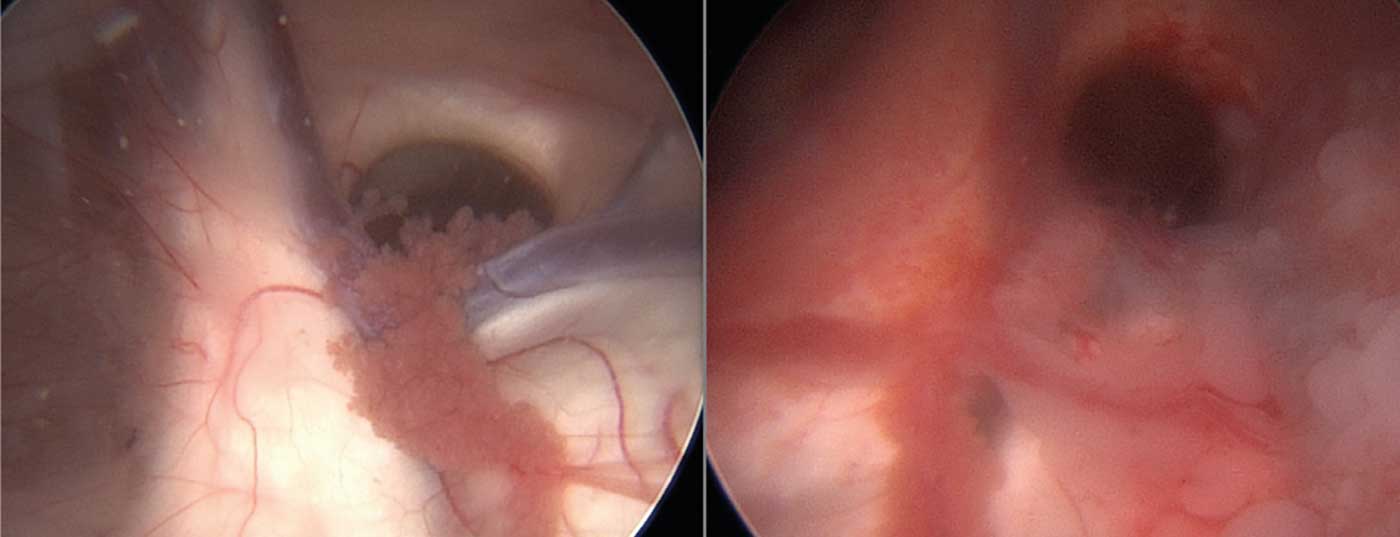
In May 2015, the somnolent patient with a clear tumor progression and intraventricular tumor manifestation with consecutive hydrocephalus occlusus (Fig. 1) was admitted as an emergency case.
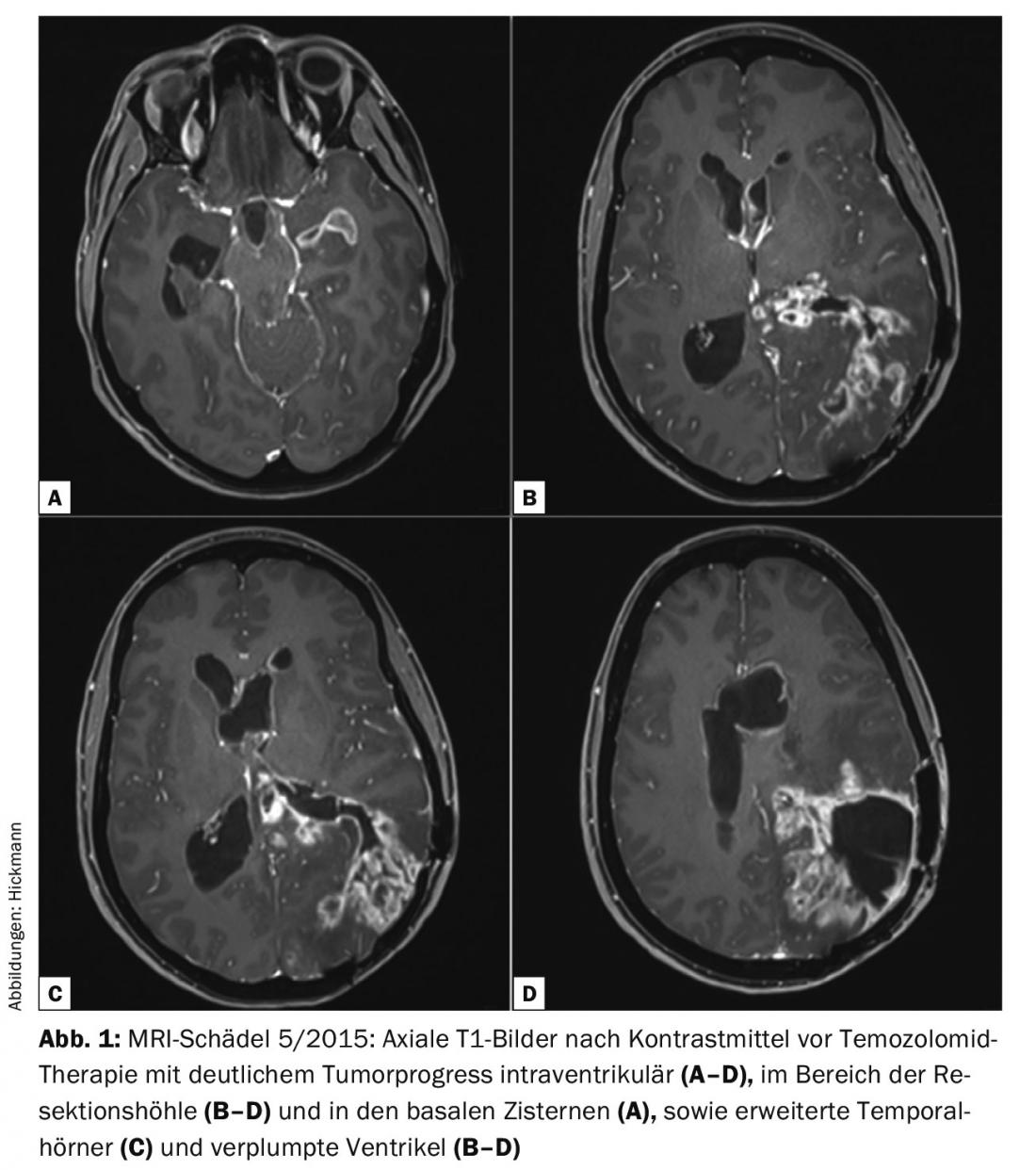
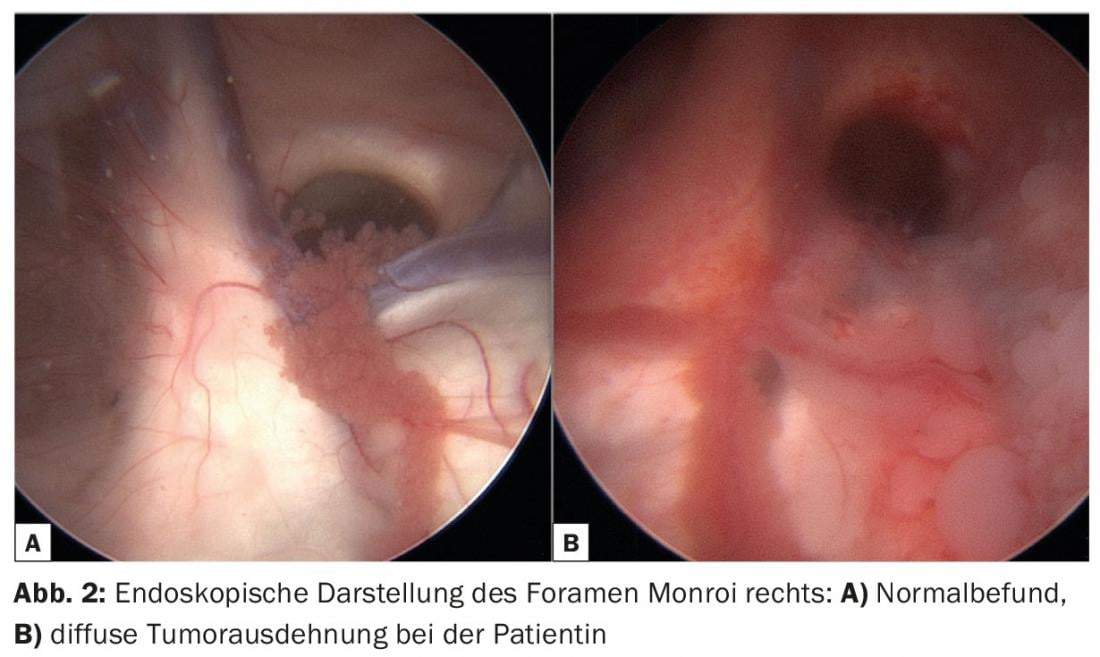
In cases of progressive intracranial pressure symptoms, palliative ventriculo-cisternostomy was performed to relieve hydrocephalus (Fig. 2). In this procedure, the floor of the third ventricle was opened using an endoscopic technique and a free cerebrospinal fluid passage to the subarachnoid spaces was achieved. After surgery, the patient showed rapid clinical recovery, so it was assumed that the preoperative symptomatology was not due to tumor progression alone.
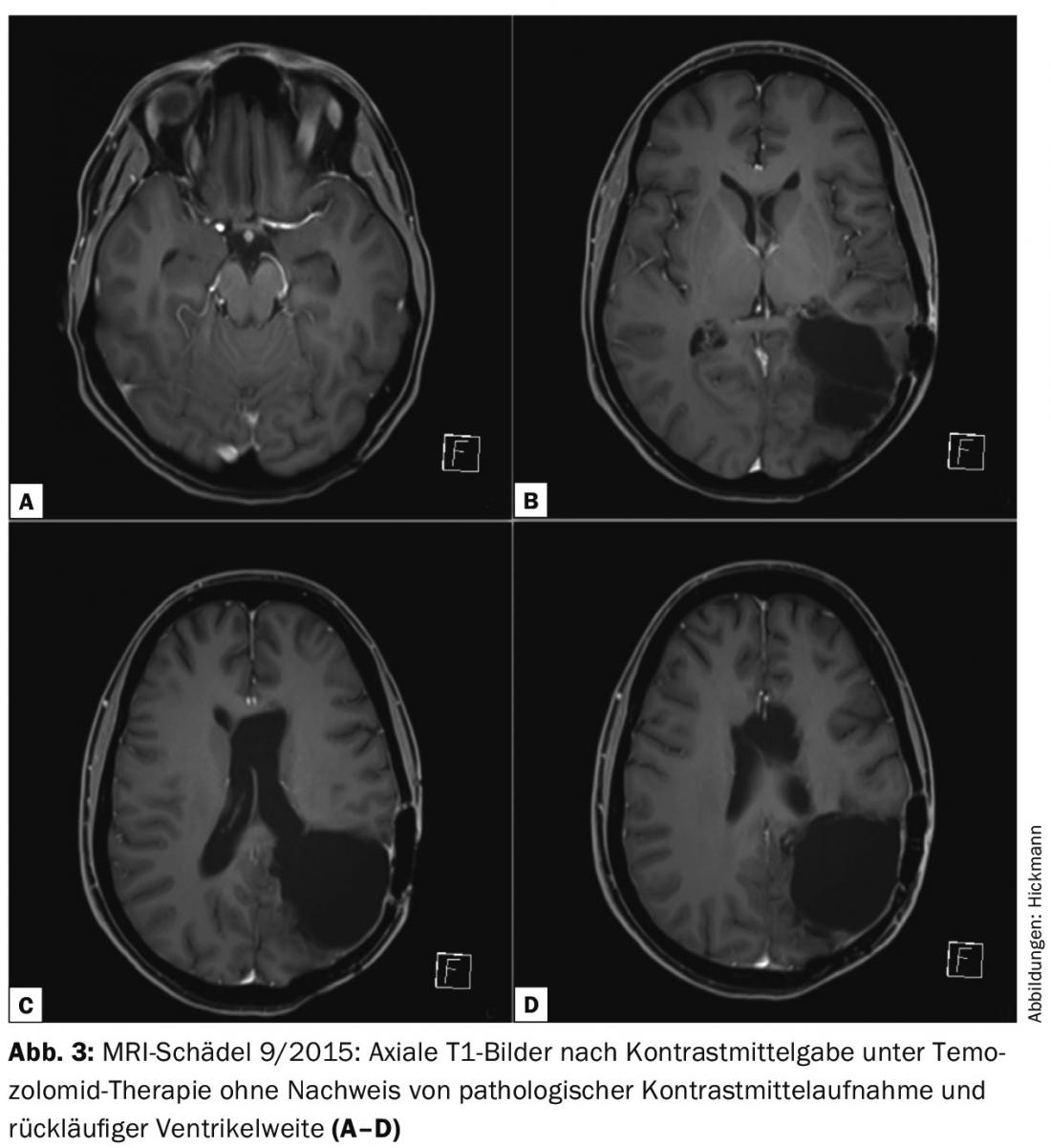
Therefore, despite the infaust overall situation, chemotherapy with temozolomide (6 cycles, regimen 5/28) was started. Under therapy, the patient’s clinical condition continued to improve. Without new neurological deficits, the Karnofsky Performance Score is 90%. Image morphology showed impressive tumor regression without evidence of contrast-enhancing tumor tissue in the last follow-up in September 2015, after four cycles of temozolomide (Fig. 3).
Discussion: The clinical course and histological findings of 2014 suggest the presence of a secondary malignant glioblastoma WHO °IV in this case, which was rather a grade III tumor in 2009. Overall, the tumor has prognostically and therapeutically favorable molecular genetic markers (IDH1 positive [sekundäre Malignisierung], MGMT methylated) [2,3]. Cases with sometimes difficult-to-interpret histological findings and remarkable clinical courses are possible due to the inhomogeneity of the tumors.
The special feature of this case, however, is the course since May 2015. Such a good response to chemotherapy was not expected. In patients with intraventricular tumor progression and deterioration in terms of acute hydrocephalus (visible temporal horns, Fig. 1C) , acute congestion therapy should be considered. In this way, it is possible to assess the extent to which the symptoms are due to tumor progression or congestion, especially if – as in this case – not all adjuvant therapy options have been exhausted and the tumor has a predictively favorable molecular genetic profile. The very good response of the recurrent tumor to chemotherapy is probably due to temozolomide naivety in addition to molecular genetic factors (MGMT-methylated) [2]. In addition, the blood-brain barrier was extensively disrupted, so that there may additionally have been particularly good CNS permeability to temozolomide. Even though this is an impressive individual case, this course confirms our idea that in patients with malignant brain tumors who have not been fully treated, more controversial therapeutic approaches should also be considered.
Literature:
- Stupp R, et al: Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 2005; 352(10): 987-996.
- Stupp R, et al: High-grade glioma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2014; 25(Suppl 3): iii93-101.
- Wen PY, Kesari S: Malignant gliomas in adults. N Engl J Med 2008; 359(5): 492-507.
InFo NEUROLOGY & PSYCHIATRY 2015; 13(6): 34-35.