The term venous thromboembolism covers thromboses of the pelvic and leg veins as well as pulmonary artery embolisms. The diagnosis and treatment of these diseases is well studied and extensively covered in guidelines. Less common and far less noticed are venous thromboses of other localizations.
Venous thromboembolism (VTE) is the term used to describe thrombosis of the iliac and leg veins (TBVT) and pulmonary artery embolism . The diagnosis and treatment of these diseases is well studied and extensively covered in guidelines. Less common and far less noticed are venous thromboses of other localizations.
Sinus vein thrombosis
The clinical symptoms of sinus vein thrombosis are varied and unfortunately nonspecific. Headache, vigilance disorder, epileptic seizures, and psychosis may occur. Therapeutically, anticoagulation at therapeutic doses, usually with unfractionated or low-molecular-weight heparin, is recommended.
Mesenteric vein/portal vein thrombosis
Mesenteric vein thrombosis often remains asymptomatic. As the disease progresses, nonspecific abdominal complaints often develop due to venous congestion with consecutive organ enlargement. If esophageal or rectal varices are present, variceal bleeding may occur in parallel with thrombosis. Therapeutically, there is an indication for full anticoagulation if there is no variceal bleeding. Triggering diseases (e.g. pancreatitis or pancreatic tumor) should be searched for.
Deep vein thrombosis of the upper extremity
Deep vein thrombosis (Fig. 1) of the upper extremity usually occurs secondarily and – due to the increased use of central venous catheters and implantation of pacemakers and defibrillators – is often iatrogenic. Primary thromboses are referred to as Paget-von-Schrötter syndrome. Paget-von-Schrötter syndrome was defined as activity-induced thrombosis of the brachial vein, axillary vein, and/or subclavian vein (“thrombosis par effort”); today, idiopathic thromboses of the aforementioned veins are often so designated. Patients with upper extremity deep vein thrombosis are younger and leaner on average than patients with TBVT and are more likely to have malignancies [1]. Probably not least for this reason, according to data from the RIETE registry (Registry of Patients with Venous Thromboembolism), there is no significant difference in death, recurrence, and major bleeding compared with TBVT [2], so deep vein thrombosis of the upper extremity is not harmless.
Clinically, there is arm swelling, arm pain, superficial collaterals, and possibly arm weakness and impaired sensory function. However, many patients also remain asymptomatic.
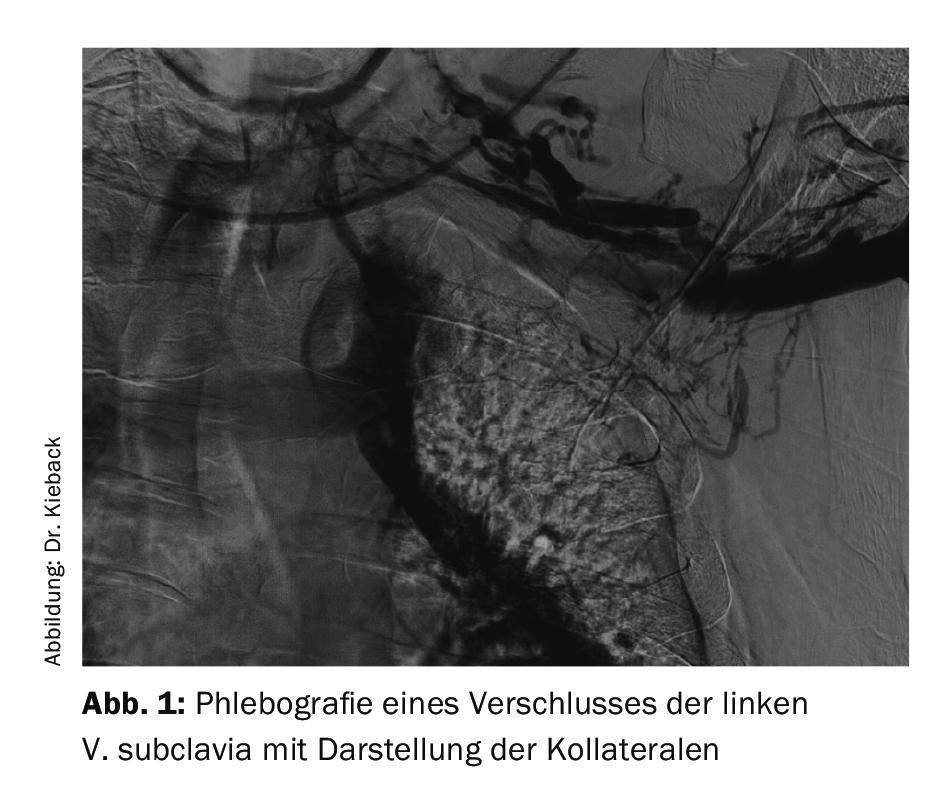
Diagnostically, clinical symptoms are indicative; sonographic evidence of thrombus is conclusive. While the diagnostic value of sonography is undisputed, there is no well-established clinical score to date, and it remains questionable whether and, if so, when D-dimer determination is helpful. In a study of 406 patients (25% upper extremity deep vein thrombosis, 13% superficial arm vein thrombosis), the use of a negative “Constans Clinical Decision Score” in combination with a normal D-dimer was able to exclude upper extremity deep vein thrombosis in only 21% of patients [3]. If sonography does not provide a clear result, the alternative option is to perform conventional, MR or CT phlebography. Similar to TBVT, thrombophilia diagnostics should only be performed if the result has immediate consequences for further therapy. In idiopathic deep vein thrombosis of the upper extremity, tumor diagnosis should be considered in elderly patients, in case of insufficient therapeutic success and other clinical indications.
As treatment – without a good data basis – anticoagulation in therapeutic dosage is recommended for three months, possibly longer if a central venous catheter is in place. Central venous catheters should be removed if this can be done without replacement. Contralateral reattachment is not recommended because of the risk of resulting bilateral thrombosis. There are no sufficient data on compression therapy, but in case of pronounced arm swelling we use it regularly. If symptoms are very pronounced, pharmacomechanical local lysis may be considered; here, the potentially much faster symptom relief must be weighed against the risk of bleeding. The only recommendation for acute deep vein thrombosis of the upper extremity in the ACCP (American College of Chest Physicians) guidelines advocates exclusive anticoagulation without lysis (2C recommendation) [4]. In venous thoracic outlet syndrome (VTOS), which pathophysiologically should be called thoracic inlet syndrome, with postthrombotic syndrome or recurrence, surgical decompression, possibly combined with intervention, should be considered.
Drug prophylaxis of deep vein thrombosis of the upper extremity is not generally recommended when a central venous catheter is placed. If both alternatives are possible, a port should be preferred to a large-lumen catheter because of the lower risk of thrombosis.
Summary
Both sinus vein thrombosis and mesenteric vein thrombosis can be easily overlooked because of nonspecific or absent clinical symptoms. Deep vein thrombosis of the upper extremity is often iatrogenic from introduced foreign material; generally, anticoagulation at therapeutic doses for three months is recommended, and data are weak.
Take-Home Messages
- Deep vein thrombosis of the upper extremity is often iatrogenic.
- In terms of death, recurrence, and major bleeding, there is no significant difference from thrombosis of the iliac and leg veins. Diagnosis is based on clinical symptoms, and sonographic evidence of thrombus is conclusive. Anticoagulation at therapeutic doses is recommended as treatment.
- Sinus vein thrombosis manifests clinically in a variety of nonspecific ways.
- Thrombosis of the mesenteric veins often remains asymptomatic at first.
Literature:
- Kucher N: Clinical practice. Deep-vein thrombosis of the upper extremities. N Engl J Med 2011; 364: 861-869.
- Cote LP, et al: Comparisons Between Upper and Lower Extremity Deep Vein Thrombosis: A Review of the RIETE Registry. Clin Appl Thromb Hemost 2017; 23: 748-754.
- Kleinjan A, et al: Safety and feasibility of a diagnostic algorithm combining clinical probability, d-dimer testing, and ultrasonography for suspected upper extremity deep venous thrombosis: a prospective management study. Ann Intern Med 2014; 160: 451-457.
- Kearon C, et al: Antithrombotic Therapy for VTE Disease: CHEST Guideline and Expert Panel Report. Chest 2016; 149: 315-352.
CARDIOVASC 2017; 16(6): 25-26











