This year, the German Society of Neurology (DGN) and the German Stroke Society (DSG) published the new S2k guideline ‘Secondary prevention of ischemic stroke and transient ischemic attack’. This contains a broad armamentarium of recommendations to reduce the risk of recurrence after ischemic insult or TIA. For maximum prophylaxis, all measures should be implemented permanently, which requires close collaboration between neurologists, primary care physicians, and affected individuals.
Stroke recurrences are relatively common. Recent analyses show that almost one in five people who have suffered a stroke are likely to have a subsequent stroke within the next five years [1]. After a transient ischemic attack (TIA), the risk of stroke is significantly increased, especially in the days immediately following the attack. Thus, recurrence prophylaxis is of particular importance. “In this context, neurological follow-up should go far beyond the medication of ‘classic’ risk factors such as high blood pressure or high lipid levels,” emphasizes DGN Secretary General Prof. Peter Berlit, MD [4]. While part 1 of the guideline focuses on drug treatment of the ‘classical’ risk factors (anticoagulation, treatment of hypercholesterolemia and hypertension), part 2 addresses the additional risk factors such as lifestyle, diabetes mellitus, hormone replacement therapy and sleep apnea [2–4].
Clarify indication for anticoagulation individually
For stroke prevention, the administration of anticoagulant drugs is necessary in certain situations or for certain diseases. “Platelet aggregation inhibition and the use of oral anticoagulation should be coordinated individually depending on the bleeding tendency, comorbidities and risk factors. The guideline provides a corridor of action within which therapy can be adapted to the individual patient,” explain Prof. Dr. med. Gerhard F. Hamann, Prof. Dr. med Armin Grau, and Prof. Dr. med. Joachim Röther, who are all experts of the German Stroke Society (DSG). [2–4].
For platelet aggregation inhibition, the guideline recommends acetylsalicylic acid (ASA), clopidogrel, and ticagrelor exclusively; other preparations have more side effects or lack evidence of added benefit. If the risk of bleeding is acceptable, early (that is, within 24 hours of symptom onset) and short-term dual antiplatelet therapy with ASA and clopidogrel for 21 days or, alternatively, ASA and ticagrelor for 30 days is possible. Affected individuals with atrial fibrillation should always receive oral anticoagulation, with direct oral anticoagulants.
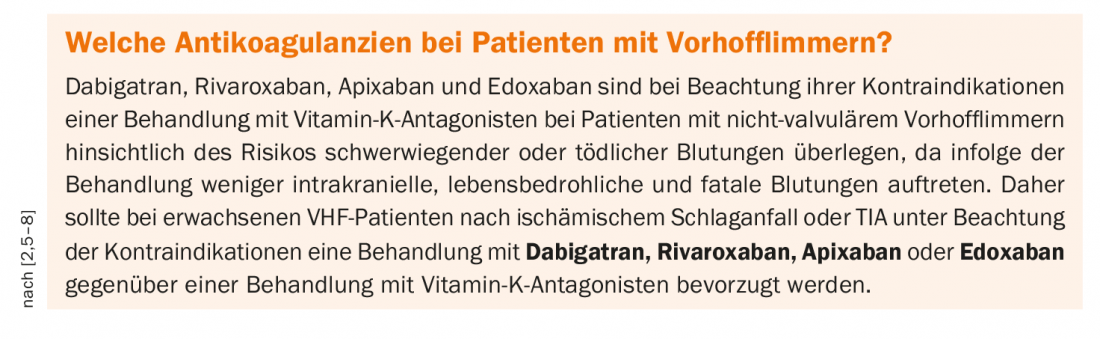
Atrial fibrillation as an indication for oral anticoagulation
Atrial fibrillation (VHF) is a common condition and sufferers have a four- to five-fold increased risk of ischemic stroke. In addition, oral anticoagulation (OAC) is a highly effective therapy to prevent stroke in VHF. Based on the current evidence, the guideline recommends OAK in patients with ischemic stroke or TIA with permanent, persistent, or paroxysmal AF [2]. (Box). Antiplatelet drugs (TFH) should not be used in secondary prevention after ischemic stroke or TIA with atrial fibrillation following the acute phase unless there is an urgent indication for TFH administration elsewhere. In the presence of existing antiplatelet therapy for other indications, interdisciplinary consensus on the need for dual or triple therapy should be sought. In case of contraindication to permanent OAK, an individual treatment attempt with LAA occlusion can be considered. In patients at increased risk of bleeding and those requiring dialysis, implantation of an atrial occluder may be considered if ischemic stroke and VCF have occurred. This is because thrombi that embolize in VCF arise in the vast majority in the left atrial appendage (LAA).
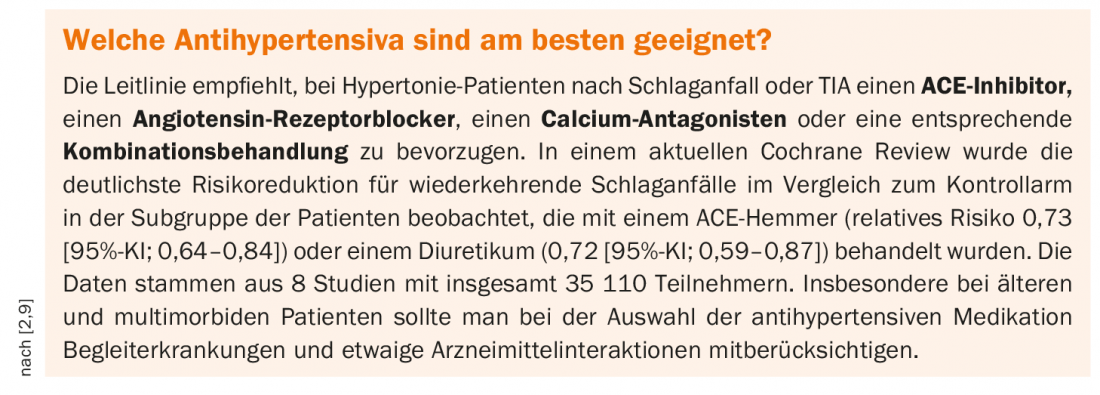
Treat hypertension and dyslipidemia
Blood pressure should be reduced below 140/90 mm Hg long-term after a stroke or TIA. Depending on the age of the patient, tolerance of antihypertensive drugs, and preexisting conditions, even a reduction to systolic 120 to 130 mm Hg should be considered, with the achievement of target blood pressure values having a higher priority than the choice of antihypertensive therapy.
Patients with a history of ischemic stroke or TIA are at high risk of developing further atherosclerotic cardiovascular disease (ASCVD), including stroke recurrence. The target value for cholesterol-lowering therapy is an LDL-C value of less than 70 mg/dl; alternatively, a reduction of >50 percent of the initial value can be achieved.
Do not disregard lifestyle factors
“For those affected, information on lifestyle in particular is highly relevant, as they can influence it themselves,” explains Prof. Tobias Kurth, MD [4]. The long-term change in lifestyle is a challenge for many patients, and physicians have to provide support time and again. Regular consumption of fruits and vegetables or a Mediterranean diet reduces the risk of stroke recurrence and subsequent vascular events. Salt consumption should be reduced. According to the guideline, there is no clear evidence for the use of dietary supplements or routine vitamin substitution. Regular physical activity, a reduction in alcohol consumption and stopping/renouncing smoking are important. Diabetes mellitus as a ‘weighty’ risk factor for stroke must be prevented. Diabetics should pay special attention to good blood glucose control after stroke (<65 years: HbA1c 6.5-7%; >65 years: HbA1c 6.5-7.5%). In addition to lifestyle modification and diabetes mellitus, Part 2 of the guideline also addresses indications for OAK beyond atrial fibrillation, as well as treatment of dissections of the brain-supplying arteries, treatment of intracranial vascular stenoses, hormone replacement therapy, and obstructive sleep apnea syndrome. In strokes associated with oncologic disease and tumor-induced hypercoagulopathy and in heart failure with an ejection fraction <35%, OAK may be considered instead of platelet function inhibition. One should specifically look for sleep apnea as an additional risk factor. Nocturnal positive airway pressure (CPAP) is the treatment of choice for moderate to severe sleep apnea. Stroke patients taking contraceptives should consider other contraceptive methods if possible.
Literature:
- Stahmeyer JT, et al: Frequency and timing of recurrences after incisional stroke. An analysis based on routine health insurance data. The frequency and timing of recurrent stroke – an analysis of routine health insurance data. Dtsch Arztebl Int 2019; 116: 711-717.
- Hamann GF, et al: German Stroke Society and German Society of Neurology. Secondary prevention of ischemic stroke and transient ischemic attack: part 1, S2k guideline, 2022, https://dgn.org/leitlinien/ll-030-133-sekundarprophylaxe-ischamischer-schlaganfall-und-transitorische-ischamische-attacke-teil-1, (last accessed, 11/23/2022).
- Olma MC, et al: Secondary prevention of ischemic stroke and transient ischemic attack-part 2, S2k guideline, 2022, German Society of Neurology (DGN) and German Stroke Society (DSG), https://dgn.org/leitlinien/ll-030-143-sekundarprophylaxe-ischamischer-schlaganfall-und-transitorische-ischamische-attacke-teil-2 (last accessed, Nov. 23, 2022).
- “New DGN and DSG guideline on secondary prevention of stroke,” German Society of Neurology (DGN), July 04, 2022.
- Diener HC, et al: Dabigatran compared with warfarin in patients with atrial fibrillation and previous transient ischaemic attack or stroke: a subgroup analysis of the RE-LY trial. Lancet Neurol 2010; 9(12): 1157-1163.
- Easton JD, et al: Apixaban compared with warfarin in patients with atrial fibrillation and previous stroke or transient ischaemic attack: a subgroup analysis of the ARISTOTLE trial. Lancet Neurol 2012; 11(6): 503-511.
- Hankey GJ, et al: Rivaroxaban compared with warfarin in patients with atrial fibrillation and previous stroke or transient ischaemic attack: a subgroup analysis of ROCKET AF. Lancet Neurol 2012; 11(4): 315-322.
- Rost NS, et al: Outcomes With Edoxaban Versus Warfarin in Patients With Previous Cerebrovascular Events: Findings From ENGAGE AF-TIMI 48 (Effective Anticoagulation With Factor Xa Next Generation in Atrial Fibrillation-Thrombolysis in Myocardial Infarction 48). Stroke 2016; 47(8): 2075-2082.
- Zonneveld TP, et al: Blood pressure-lowering treatment for preventing recurrent stroke, major vascular events, and dementia in patients with a history of stroke or transient ischaemic attack. Cochrane Database Syst Rev 2018 Jul 19;7(7): CD007858. doi: 10.1002/14651858.CD007858.pub2.
InFo NEUROLOGY & PSYCHIATRY 2022; 20(6): 34-35.