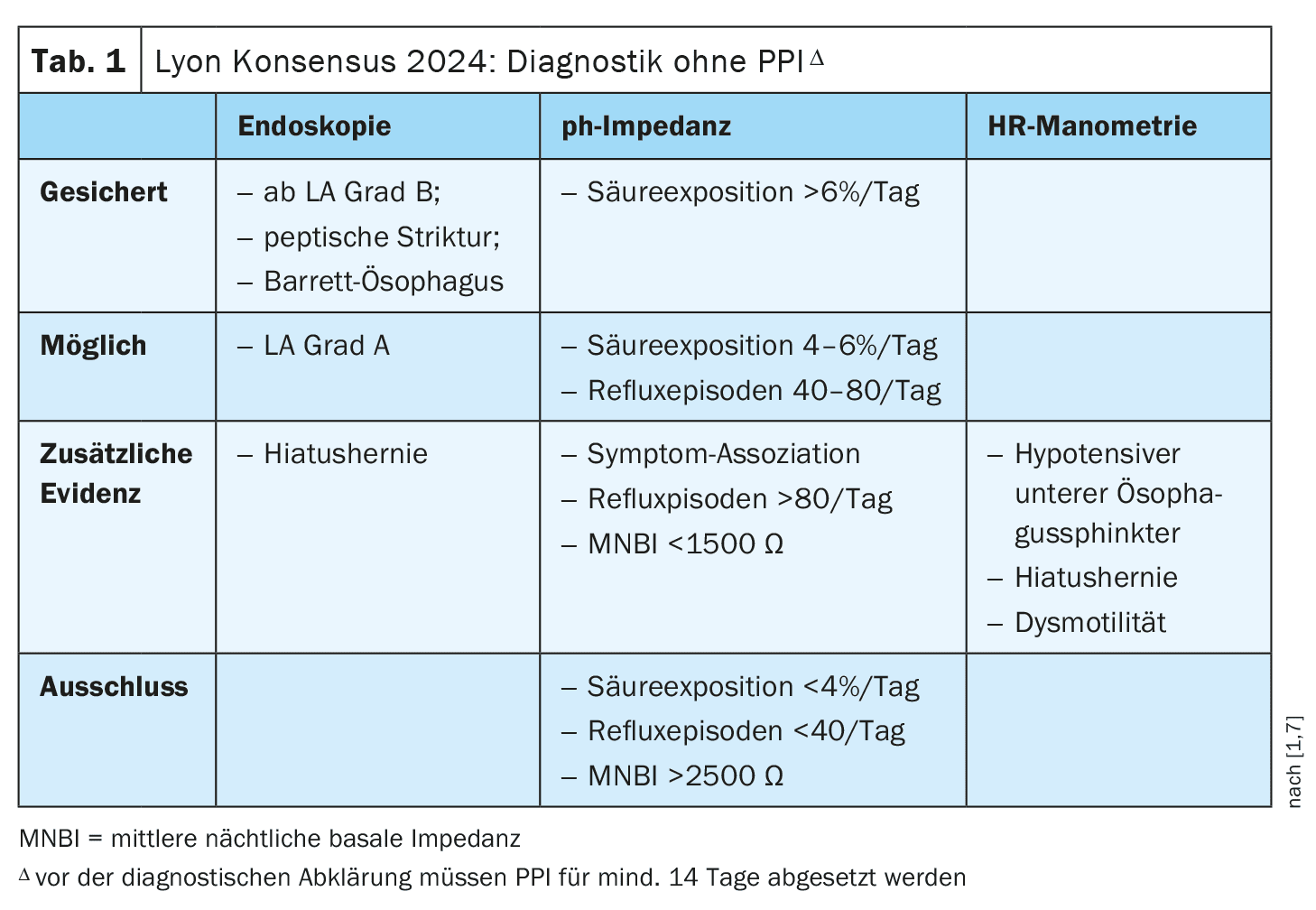
The Lyon consensus decision published last year included some important innovations. The criteria for confirming the diagnosis of GERD and the exclusion criteria have been slightly modified. There are slightly differing recommendations in international guidelines on the question of which cases should be investigated for the presence of Barrett’s metaplasia or oesophageal adenocarcinoma.
In gastroesophageal reflux disease (GERD), reflux of stomach contents into the oesophagus causes disturbing symptoms and/or complications. “You can initially treat patients with typical reflux symptoms empirically, provided there are no alarm symptoms, anemia, dysphagia or weight loss and the family history is negative,” says Prof. Franz Ludwig Dumoulin, MD, Chief Physician Internal Medicine, Community Hospital Bonn [1]. “You can then even treat them with an increased PPI dose, but after 2 x 8 weeks, a third to half of patients still suffer from symptoms” [1]. The speaker emphasized that this is the latest point at which it is important to consider whether reflux disease is really present [1].
Checking a suspected diagnosis: two key criteria
To get to the bottom of the question, an endoscopy of the upper digestive tract** should first be performed to examine the oesophagus for any reflux-related mucosal changes that can be evaluated according to the Los Angeles (LA) classification [2]. According to the Lyon consensus updated in 2024, esophagitis from LA grade B$ qualifies for a GERD diagnosis. This is an important innovation; in previous consensus decisions, at least grade C was required. In contrast, low-grade oesophagitis (LA grade A) is still not considered pathological [2,7]. If the suspected diagnosis of GERD cannot be confirmed by endoscopy, outpatient reflux monitoring should be performed, whereby patients must not be under PPI treatment. According to the Lyon consensus, the acid exposure time acts as a decisive alternative criterion; if this is >6% during impedance pH monitoring, the GERD diagnosis is considered confirmed. Increasing acid exposure time correlates with a higher severity of esophagitis and an increased length of intestinal metaplasia [2]. If the acid exposure time is <4%, reflux disease can be ruled out. A nocturnal basal impedance >2500 Ω serves as a new exclusion criterion [1].
** Do not take PPI for at least 14 days beforehand [1].
$ LA Grade B corresponds to erosions >5 mm [3]
Barrett’s screening only for GERD symptoms?
Barrett’s esophagus – also known as Barrett’s metaplasia – is characterized by a transformation of the squamous epithelium into a cylindrical epithelium [4]. It is the only known precursor of esophageal adenocarcinoma. On the question of whether patients should undergo screening, the German s2k guideline cites several years of reflux symptoms as a key criterion [5]. According to the speaker, this is also in line with the recommendation of other guidelines – the only one that goes somewhat against the grain is the AGA Clinical Practice Update published in 2022 [6]. This guideline suggests screening for Barrett’s oesophagus and oesophageal adenocarcinoma in patients with at least three established risk factors – regardless of whether a reflux problem is present [6]. These risk factors include: male gender, fair-skinned ethnicity, age >50 years, history of smoking, chronic reflux symptoms, obesity or a positive family history of Barrett’s oesophagus and/or oesophageal adenocarcinoma.
Congress: Internist update
Literature:
- “Gastroenterology I”, Prof. Dr. med. F.L. Dumoulin, internist update, 22-23.11.2024, livestream.
- Davis TA, Gyawali CP: Refractory Gastroesophageal Reflux Disease: Diagnosis and Management. J Neurogastroenterol Motil 2024; 30(1): 17-28.
- Armstrong D, et al: The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology 1996; 111(1): 85-92.
- “Barrett’s esophagus”, https://flexikon.doccheck.com,(last accessed 14.01.2025).
- Madisch A, et al: S2k guideline Gastroesophageal reflux disease and eosinophilic esophagitis of the German Society of Gastroenterology, Digestive and Metabolic Diseases (DGVS), March 2023 – AWMF registry number: 021-013.
- Muthusamy VR, et al: CGIT Barrett’s Esophagus Consensus Conference Participants. AGA Clinical Practice Update on New Technology and Innovation for Surveillance and Screening in Barrett’s Esophagus: Expert Review. Clin Gastroenterol Hepatol 2022; 20(12): 2696-2706.e1.
- Gyawali CP, et al: Updates to the modern diagnosis of GERD: Lyon consensus 2.0. Gut 2024; 73(2): 361-371.
HAUSARZT PRAXIS 2025; 20(1): 34 (published on 23.1.25, ahead of print)