Most vaccinations are given in early childhood. But there are also vaccination dates for adults that should be observed, because they not only provide individual protection, but also contribute to the protection of fellow people and the entire population. There are also special vaccination recommendations for people with chronic diseases, as well as for regions in Germany and abroad where there is an increased incidence of certain diseases.
Basically, you never have to start over with vaccinations, explains Prof. Philip Tarr, M.D., Co-Chief Physician of the University Medical Clinic and Head of Infectiology and Hospital Hygiene at the Baselland Cantonal Hospital, Bruderholz [1]. Also, for very large vaccination intervals, with several years between them, simply administer the missing doses. This is because a longer interval between vaccine doses is generally more immunogenic and results in higher antibody titers than an interval that is too short. For example, the third vaccination dose for hepatitis B should rather be given 6-12 months after the second dose and not after 4-5 months.
Hepatitis B
Generally, for hepatitis B, a person is considered immune if he or she can provide written documentation of a complete vaccination series of at least three doses. In Switzerland, HBsAK ≥ 100 IU/mL are still considered protective for employees in the medical sector. In the USA, a HBsAK ≥ 10 IU/mL has been considered a protective titer since 2013. Immunocompetent individuals with these criteria have long-term protection. You don’t need any other titer controls or boosters. If these criteria cannot be met, for example because the written documentation is missing, a titer check can be performed. However, so-called blind titers must be considered here. These can be negative despite the immunological memory. It is then recommended to administer another vaccine dose and measure the titer again after 1-2 months [2]. If an anamnestic immune response has occurred, the titer control is positive after this period. If it is still negative, it is referred to as a non-responder. Approximately five to eight percent of those vaccinated are non-responders. In these individuals, chronic hepatitis B should first be ruled out by HBsAg and HBcAK. If chronic hepatitis B is not present, additional doses of vaccine can be administered and the HBs-AK repeated. Typically, circa 25-50% of individuals seroconvert after one additional dose of vaccine, 67% after three additional doses, and 80% after Twinrix than when only one hepatitis B vaccine is administered [3].
If the vaccination status is unclear, the vaccinations should be made up
If the immune status of a person with a wound needs to be clarified quickly, the tetanus antibody titer can provide information on whether there is sufficient vaccination protection against tetanus. Depending on the results, a booster dose may be given. On the other hand, if the test is negative, three doses 0, 2, 8 months are administered. However, determining vaccination status is difficult, especially for applicants who often enter the country without written documentation. Therefore, applicants without a vaccination card or documented vaccinations should be considered unvaccinated and vaccinated with priority vaccines within the first few days of arrival. These include: dTPa-IPV according to titer or 0, 2, 8 months, HiB (no vaccination if age ≥5 years, MMR if born 1964 or younger two doses at least four weeks apart, HBV three doses 0, 1, 6 months after exclusion of chronic hepatitis B by HBsAg and HBcAK, and varicella ages 0-39 years two doses at least four weeks apart. Varicella vaccination is explicitly recommended in children 12 months to 11 years of age, although it is not recommended for native children until 11 years of age in the Swiss Vaccination Schedule [4].
Vaccination in immunosuppression
Immunocompromised individuals may not only be more susceptible to certain infections, they may also have more severe courses of certain infections and severe vaccine reactions/complications may occur with live vaccinations. This includes, for example, patients with advanced HIV infection and AIDS (CD4 lymphocyte count <15% at age 1-5 years, <200/μL at age 6 years and older), steroid treatment (prednisone equivalent ≥2 mg/kg/day or ≥20 mg/day for >14 days), use of other immunosuppressive drugs, severe (chronic) diseases such as leukemia, lymphoma, or cancer, and patients with congenital immunodeficiency. The Federal Office of Public Health (FOPH) therefore recommends administering live attenuated vaccines at least four weeks before starting immunosuppression. Live attenuated and therefore contraindicated vaccines include MMR, varicella, Zostavax (not Shingrix = dead vaccine), yellow fever, oral polio vaccine (not injected polio vaccine = dead vaccine), and oral Salmonella typhi vaccine. Temporary discontinuation of immunosuppression (two or four weeks) due to vaccination may result in transient relapses depending on the severity of the disease.
Prior to organ transplantation, the same vaccination recommendation generally applies as for the general population, with the exception of live vaccines. There are no safety concerns with inactivated vaccines, but they may be less effective. It should also be noted that vaccination response depends on the degree of disease. The worse the patient’s health, the worse the vaccination response. Therefore, it is important to close the vaccination gaps as early as possible, administer booster doses and measure the vaccination response 1-3 months later.
Vaccinate during pregnancy
Similarly, pregnancy is considered an immunosuppressive condition. MMR and varicella vaccinations are contraindicated in this condition. However, an all-clear can be given for accidentally vaccinated pregnant women; so far, no damage to the fetus is known. Flu vaccinations, on the other hand, can also be recommended during pregnancy, as they have a positive effect on the mother and the newborn in terms of antibiotic use, fever, and influenza illness. Pertussis vaccination should also be given, as it provides more than 80% protection for newborns. Ideally, vaccination is given in the second trimester and should be repeated in each pregnancy, as vaccine protection lasts only 1-3 years. All other persons with baby contact should also receive a pertussis booster if the last vaccination was more than ten years ago. The minimum interval to the last tetanus vaccination should be at least four weeks.
Varicella vaccination
According to the FOPH, the history of a previous varicella infection is reliable. These individuals may be considered immune. All non-immune individuals 11 years of age and older are recommended to be vaccinated with two doses at four-week intervals until 39 years of age, because a severe course is possible with a varicella primary infection after 16 years of age (varicella pneumonia). If vaccination is denied, IgG control can be offered; if positive, vaccination is not necessary.
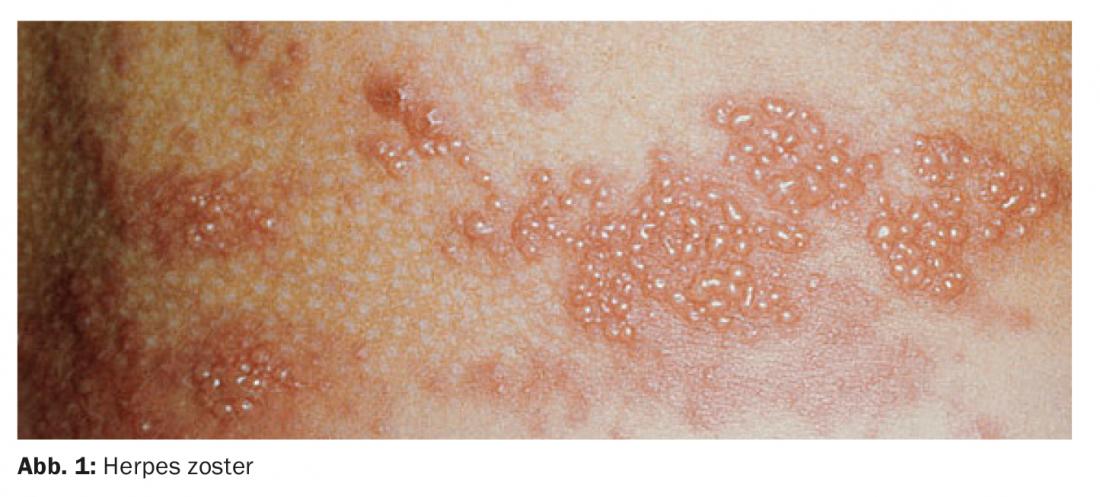
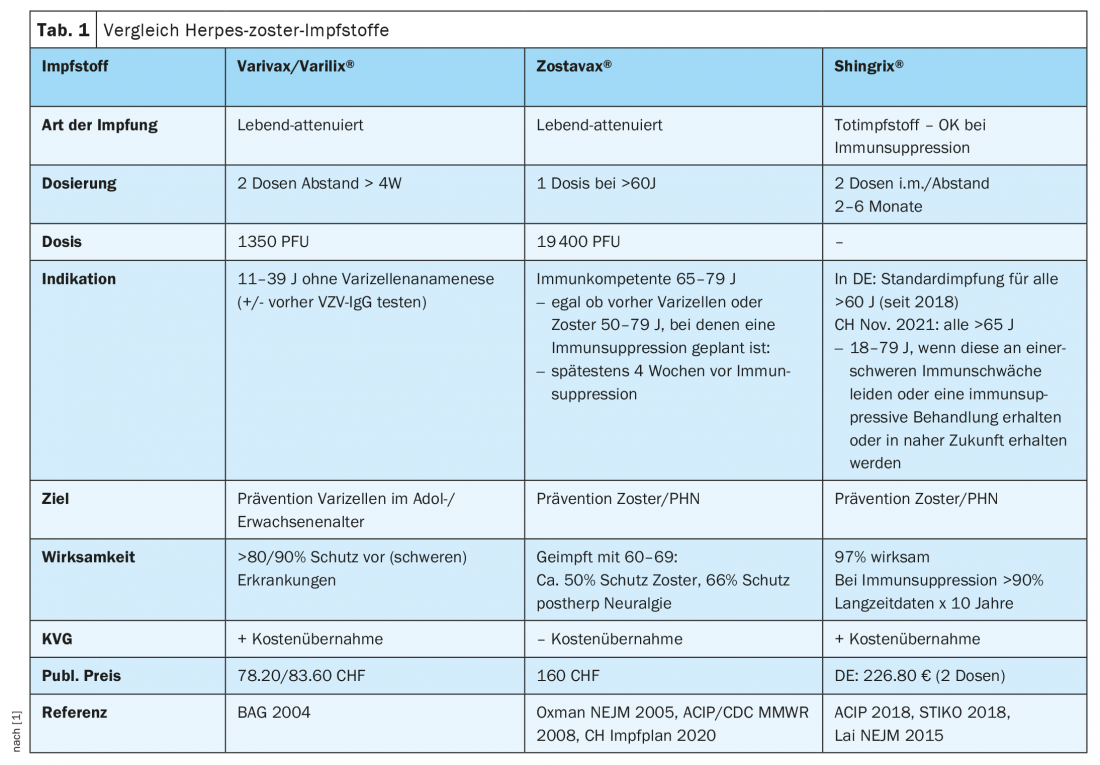
New recommendation for vaccination against herpes zoster
In October 2021, Swissmedic approved the vaccine Shingrix in Switzerland. The dead vaccine, unlike the conventional vaccine, is administered in two doses 2-6 months apart and can also be used in individuals with immunosuppression. One dose (0.5 ml) contains 50 μg of VZV glycoprotein E (gE) antigen produced by recombinant DNA technology. Efficacy is 97% and long-term immunological data are available for a duration of ten years. However, local reactogenicity is higher and pain at the injection site is more common than with most other vaccines. (Tab. 1) [1].
Vaccinations for splenectomy
A single pneumococcal vaccination with Prevenar 13 is recommended for splenectomy. The vaccination interval from the last Pneumovax should be at least 12 months. For persons >5 no KVG cost coverage obligation, as Prevenar 13 is not Swissmedic approved in this age group (retail price CHF 91.20). Furthermore, vaccination against meningococcal disease is recommended. Vaccination is done with Menveo in two doses 0 and 2 months. A booster vaccination should be given after five years. The vaccination interval from the last Mencevax dose should be at least 12 months. In addition, the annual influenza vaccination should be given and an emergency kit with CoAmoxicillin 3x1g/d is recommended. Vaccinations are ideally administered before splenectomy, as a better immune response can be expected.
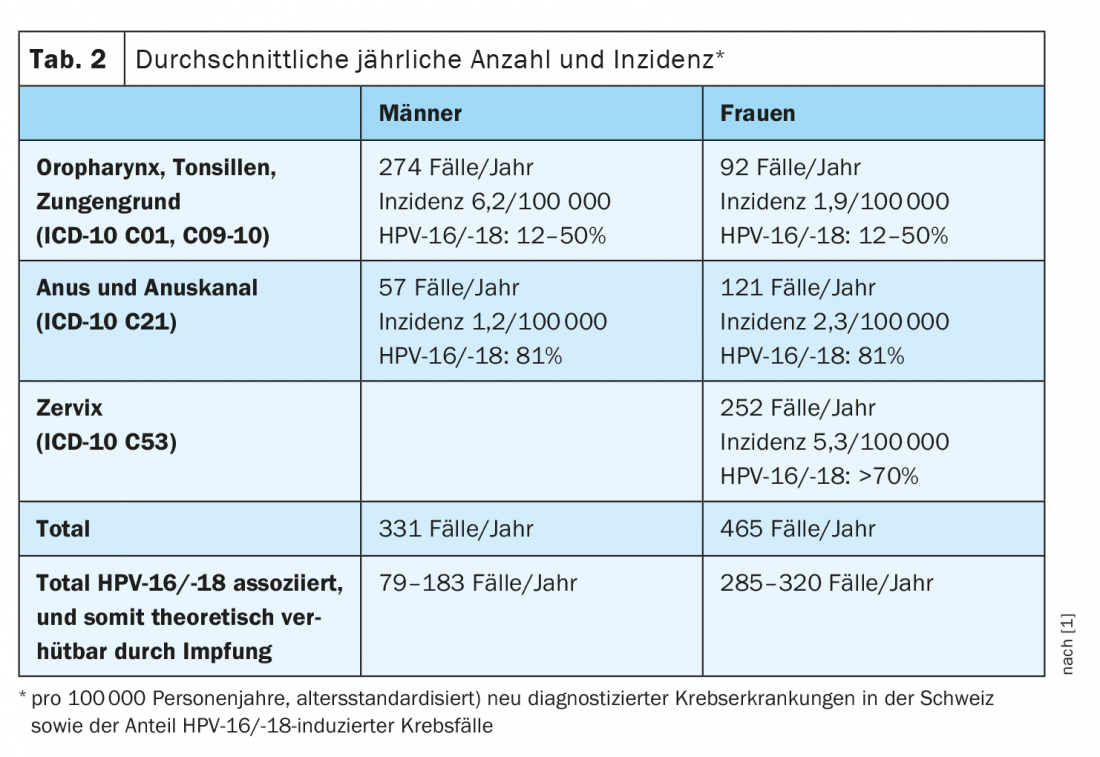
HPV vaccination
HPV vaccination may in principle be carried out by any doctor, but it is only paid for within the framework of cantonal vaccination programs and up to the age of 26. The first vaccination is best given before the first sexual intercourse. If the first dose is given before the age of 15, a total of two doses of vaccine are given, followed by a total of three doses. Since 2015, vaccination has also been recommended for young men, especially due to the increase in oropharyngeal cancer but also penile and anal cancer and genital warts [5]. According to the FOPH, about 79-183 HPV-associated cancers per year can be prevented by vaccination in men, and 285-320 cases per year in women. Thus, HPV also plays a significant role in the development of neoplasms in men in Switzerland, although overall HPV-associated cancers are less common in men than in women (Table 2) [6].
Meanwhile, studies have shown that HPV vaccination reduces not only dysplasia and persistent HPV infections, but also cervical cancer. For example, vaccination with the active ingredient Gardasil reduces the risk of cancer cells appearing by about 60%. The effect could be even greater (almost 90%) if vaccination is given before the age of 17 [7]. In contrast to the naturally passed HPV infection, 99% of the vaccinated form antibodies. These last much longer and are 10-100 times higher than after natural infection [8]. Since antibody titers hardly decrease over 10 years, booster vaccinations are not recommended. The vaccine protection lasts at least 20 years, probably even a lifetime.
Rabies vaccination
Rabies vaccination is nowadays carried out in a more low-threshold manner and is especially recommended for trekking or backpacking in Asia. Basic immunization consists of two doses (0, 28 months) intramuscularly, preferably four weeks before travel. For immunosuppression, a total of three doses are administered (0, 7, 21-28 months). To ensure that protection lasts for the long term (at least 10 years), a booster vaccination should be given after 12 months or, if necessary, before the next trip. Measures for post-exposure prophylaxis (PEP) are to be implemented only if the suspicion of exposure to rabies virus cannot be refuted. Previously vaccinated individuals will receive two booster doses on days 0 and 3 and an antibody titer check on day 14 when PEP is performed. Previously unvaccinated individuals will receive four active vaccine doses on days 0, 3, 7, and 14 and a subsequent antibody titer check on day 21.
TBE and Salmonella typhi vaccination
The TBE vaccination recommendation has remained unchanged since 2006 and is recommended for all persons living in or temporarily residing in endemic areas (≥14 days per tick season). Basic immunization consists of three doses of vaccine: Encepur, children 6 years and older, 0, 1-3, 9-12 months and TBE Immune, Junior, 0, 1-3, 5-12 months. Vaccine protection is present two weeks after the second vaccination, and a booster is recommended every 10 years.
The FOPH recommends Salmonella typhi vaccination only for travel to the Indian subcontinent, i.e. for India, Nepal, Pakistan and Bangladesh. In this case, the live-attenuated oral vaccination in three doses at intervals of 48 hours is possible (not applicable in case of immunosuppression or together with mefloquine or antibiotics) and the dead vaccination by injection with Typhim Vi, which is performed only via the Tropical Institute, explains the speaker.
Congress: Forum for Continuing Medical Education
Literature:
- Prof. Philip Tarr, MD: Vaccination recommendations for adults, Forum Medizin Fortbildung (FOMF) lecture, Jan. 28, 2022.
- Schillie, et al: MMWR: CDC Guidance for Evaluating Health-Care Personnel for Hepatitis B Virus Protection and for Administering Postexposure Management. Morbidity and Mortality Weekly Report 2013, www.cdc.gov/mmwr/pdf/rr/rr6210.pdf.
- Loubet, et al: Alternative hepatitis B vaccine strategies in healthy non-responders to a first standard vaccination scheme. The Lancet 2020, https://doi.org/10.1016/S1473-3099(19)30582-1.
- Notter, et al: Recommendations for vaccination and prevention and outbreak management of communicable diseases in federal asylum centers and cantonal collective housing. FOPH 2019.
- Dietrich, et al: HPV vaccination: 2019 update for vaccination counseling. Swiss Medical Forum – Schweizerisches Medizin-Forum, 19(1314), 220-226, https://doi.org/10.4414/smf.2019.08064.
- Federal Office of Public Health (FOPH): Bulletin 10/15. 2015
- Lei, et al: HPV Vaccination and the Risk of Invasive Cervical Cancer. N Engl J Med 2020, doi: 10.1056/NEJMoa1917338.
- Beachler, et al: Natural Acquired Immunity Against Subsequent Genital Human Papillomavirus Infection: A Systematic Review and Meta-analysis. The Journal of Infectious Diseases 2016. https://doi.org/10.1093/infdis/jiv753.
HAUSARZT PRAXIS 2022; 17(2): 40-42 (published 2/14/22, ahead of print).