Bruno Kägi, MD, Zurich, reported on his experience with VNS and explained how it can be combined with other psychiatric treatments in cases of severe or treatment-resistant depression.
The vagus nerve consists of 80% afferent fibers that terminate predominantly in the nucleus tractus solitarius (NTS), which is connected to the amygdala and the limbic system. Stimulation of the vagus nerve affects neurotransmitters such as gamma-aminobutyric acid (GABA), serotonin, and norepinephrine [1]. There are others, but they play a minor role.
The role of the vagus nerve has been studied for over one hundred years. In 1988, the company was founded by Dr. Kiffin Penry first treated a patient with refractory epilepsy with VNS. The procedure was first approved by the FDA in 1997. Since then, it has been used worldwide in the treatment of epilepsy when conventional drugs do not work. Since the beginning of this century it has also been used in Switzerland for depression.
Concept of treatment-resistant depression
“Treatment-resistant depression” (TRD) can be said to occur when there is an inadequate response to usual therapy in the context of the relevant guidelines, Kägi elaborated. “Response” is the opposite of “resistance”. In research, “response” means a greater than 50% reduction in symptoms from “baseline” as measured by standardized rating scales [2,3]. Nearly half of the remitted patients still have symptoms – a full remission is rather rare anyway. At least 35% of patients are non-responsive for depression despite forced therapy with more than four conventional treatments. The suicide rate in this group is twice as high as in the non-therapy resistant depression group [4].
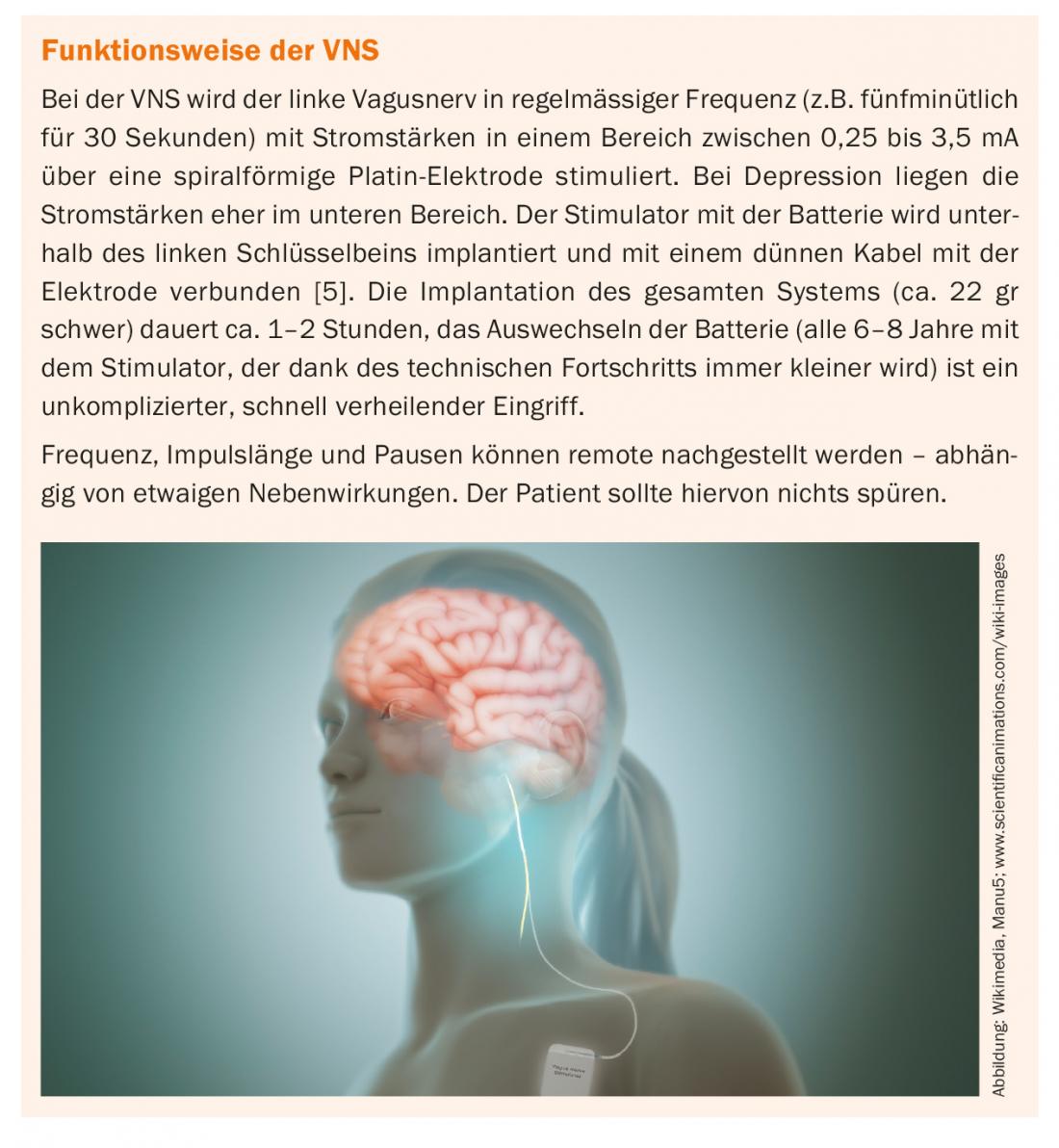
Mode of action of the VNS
The VNS alters pathways between the NTS, amygdala, and limbic system over an extended period of time (approximately three quarters of a year). β-adrenergic receptors are activated. It also modulates the activity of limbic, paralimbic, and cortical structures. Regional blood flow (rCBF) in the dorsolateral and prefrontal cortex is altered [6–8].
This increases the concentration of monoamines and produces an effect similar to that of SSRIs. Dr. Kägi went on to say that almost all patients reported augmenting existing therapy with VNS.
The efficacy of VNS showed up to 60% reduction in depressive symptoms, although some of the studies had low case numbers, Dr. Kägi said [9]. Efficacy can also be achieved for anxiety or obsessive-compulsive disorders over a period of more than half a year [10,11]. A metastudy of 14 uncontrolled studies showed a “response” of 31.8% [12]. In a study of outcome in TRD, treatment as usual (TAU) together with VNS achieved better results than TAU alone in a five-year follow-up, with a cumulative response rate of 67.6% compared with 40.9% [13].
Compatibility
From his practice, Dr. Kägi was able to report that VNS is generally well tolerated. Hoarseness, coughing or shortness of breath during stimulation, and neck pain were among the side effects that could be easily controlled by readjusting the stimulation settings (frequency, current intensity, pauses). In the case of swallowing difficulties, acid regurgitation and vomiting, it may be necessary to take countermeasures with medication. Rarely, tachycardia is noted, which may need to be treated with beta-blockers. Wound infection is also rare, he said. The dosages must be adapted to the individual patient in a finding process. In addition to adjusting the stimulation itself, additional psychotropic drugs (SSRI, SNRI) can support the effect. Contraindications exist in cases of acute suicidality, anamnestic non-compliance, manifest addictive disorders or personality disorders (case example: the paranoid processing of the foreign body) or concomitant severe psychiatric illnesses.
Conclusion
In summary, Dr. Kägi rates VNS as a safe neurostimulation procedure for the treatment of TRD or major depression that combines well with other psychiatric treatments and has augmentative effects. It contributes to remission in the long-term course.
Source: Forum for Continuing Medical Education, Psychiatry and Psychotherapy Update Refresher, June 14, 2018, Zurich.
Literature:
- George MS, et al: Novel treatments of mood disorders based on brain circuitry (ECT, MST, TMS, VNS, DBS). Semin Clin Neuropsychiatry 2002; 7(4): 293-304.
- Trevino K, et al: Defining treatment-resistant depression: a comprehensive review of the literature. Ann Clin Psychiatry 2014; 26(3): 222-232.
- Malhi GS, Byrow Y: Is treatment-resistant depression a useful concept? Evid Based Ment Health 2016 Feb; 19(1): 1-3.
- Rush AJ: STAR*D: what have we learned? Am J Psychiatry 2007; 164(2): 201204.
- Sackeim HA: Vagus Nerve Stimulation, in: Lisanby SH (editor): Brain Stimulation in Psychiatric Treatment (Review of Psychiatry Series, Volume 23; Oldham JM and Riba MB, series editors). Washington, DC, American Psychiatric Publishing, 2004; 99-142.
- Nemeroff CB, et al: VNS therapy in treatment-resistant depression: clinical evidence and putative neurobiological mechanisms. Neuropsychopharmacology 2006; 31(7): 1345-1355.
- Shah A, et al: Therapeutic modalities for treatment-resistant depression: focus on vagal nerve stimulation and ketamine. Clin Psychopharmacol Neurosci 2014; 12(2): 83-93.
- Kosel M, et al: Chronic vagus nerve stimulation for treatment-resistant depression increases regional cerebral blood flow in the dorsolateral prefrontal cortex. Psychiatry Res 2011; 191(3): 153-159.
- Carreno FR, Frazer A: Vagal Nerve Stimulation for Treatment-Resistant Depression. Neurotherapeutics 2017; 14(3): 716-727.
- Müller HHO, et al: Efficacy and long-term tuning parameters of vagus nerve stimulation in long-term treated depressed patients. J Clin Neurosci 2017; 44: 340-341.
- Müller HHO, et al: Vagus Nerve Stimulation (VNS) and Other Augmentation Strategies for Therapy-Resistant Depression (TRD): Review of the Evidence and Clinical Advice for Use. Front Neurosci 2018; 12: 239.
- Martin JL, Martín-Sánchez E: Systematic review and meta-analysis of vagus nerve stimulation in the treatment of depression: variable results based on study designs. European Psychiatry 2011; 27(3): 147-155.
- Aaronson ST, et al: A 5-Year Observational Study of Patients With Treatment-Resistant Depression Treated With Vagus Nerve Stimulation or Treatment as Usual: Comparison of Response, Remission, and Suicidality. J Psychiatry 2017; 174(9): 907.
InFo NEUROLOGY & PSYCHIATRY 2018; 16(4): 33-34. published 6/21/18 (ahead of print).