The diagnosis of HIV is no longer a death sentence, because the infection can be treated with antiretroviral combination therapy. The following article shows when which therapy should be started and what the “Swiss Statement” is all about.
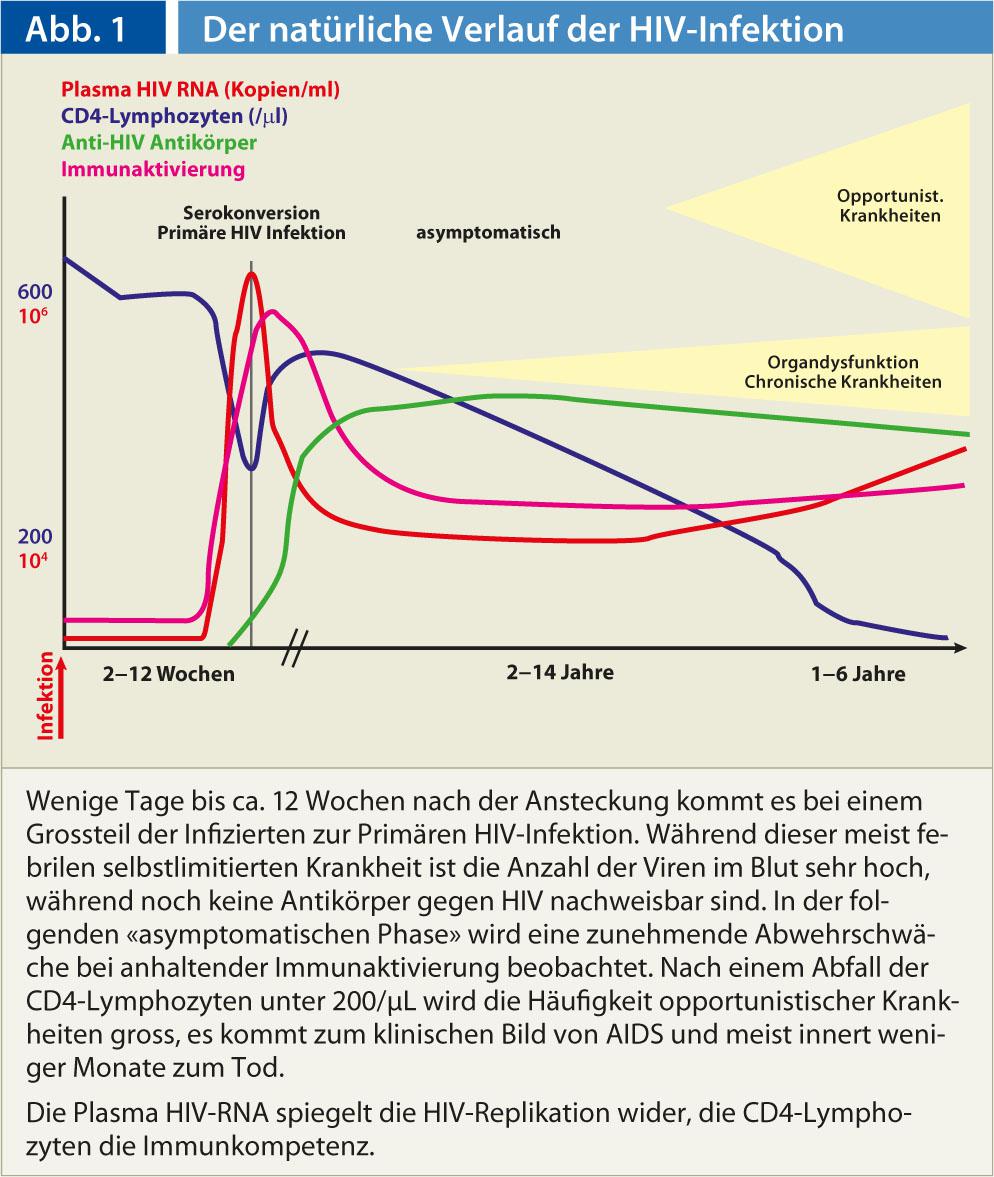
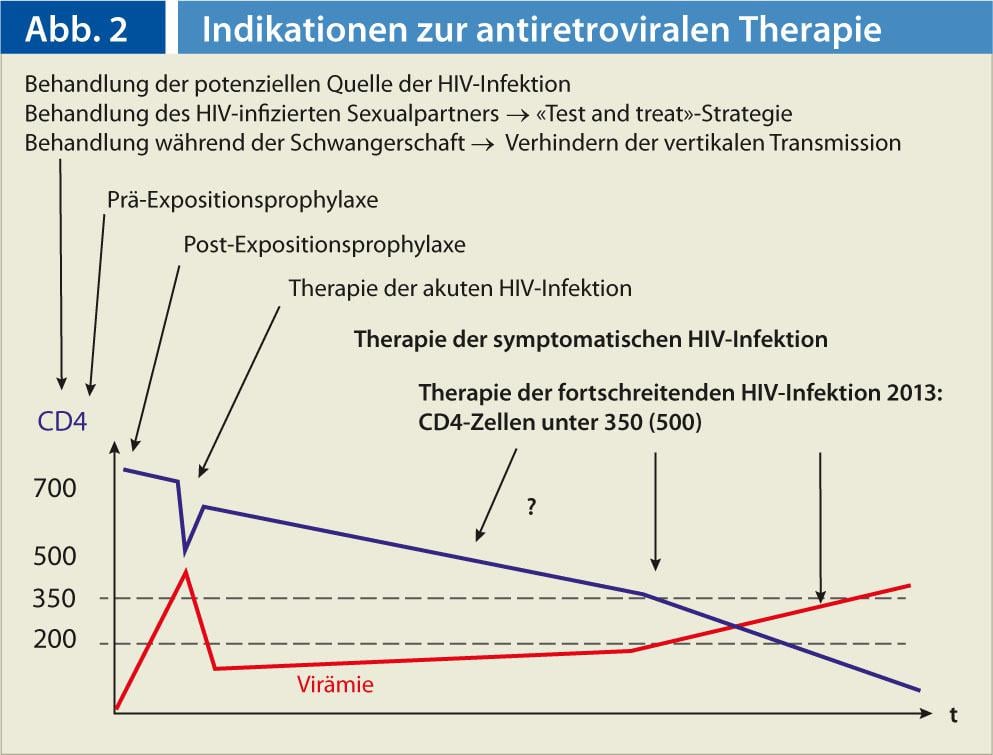
Combination antiretroviral therapy (ART), which has been used since 1996 with the aim of completely suppressing HIV replication, has significantly improved the “natural course” (Fig. 1) of HIV infection in terms of morbidity and mortality in HIV-infected individuals and has led to a life expectancy comparable to that of the normal population in many affected individuals. Also, successful treatment massively reduces the infectivity of the HIV-infected person. In addition to treating chronic progressive HIV infection, antiretroviral medications are also used to treat acute HIV infection, prevent transmission from mother to newborn, and provide post-exposure prophylaxis (PEP). Pre-exposure prophylaxis (PrEP), i.e., treatment prior to high-risk behavior to prevent infection (Fig. 2), is also a possible use – but one that is not covered by health insurance.
Antiretroviral drugs disrupt the life cycle of HIV by inhibiting the docking of the virus to the cell (CCR5 and fusion inhibitors) and interfering with viral enzymes through nucleoside and non-nucleoside reverse transcriptase inhibitors, inhibitors of integrase and protease. The goal is complete suppression of HIV replication. This is monitored with the measurement of HIV RNA in plasma. The value of HIV RNA must be below the detection limit of current amplification methods if antiretroviral therapy is successful.
The therapy of progressive HIV infection
Therapy for progressive HIV infection is the most common indication for ART prescription. The essential questions in this indication are:
- Is the patient ready for ART?
- When to start?
- Choice of ART?
- Care of patients on ART?
Readiness for ART: The decision to start antiretroviral therapy is a major break in the daily life of the HIV-infected person. He must decide to take daily medication with possible side effects for the rest of his life. A therapy adherence of >90% is necessary for sustained therapy efficacy, otherwise drug resistance will develop. The decision to treat cannot be made in a single consultation, and the patient’s environment should be involved in this decision. Only when the individual actively chooses ART should treatment be considered.
When to start? Undisputed is the use of ART in symptomatic HIV infection, especially in the presence of opportunistic disease. Inhibition of HIV replication allows recovery of the immune system, which is characterized by an increase in CD4 lymphocytes in peripheral blood. This recovery of the immune system subsequently prevents further opportunistic diseases (Fig. 3).
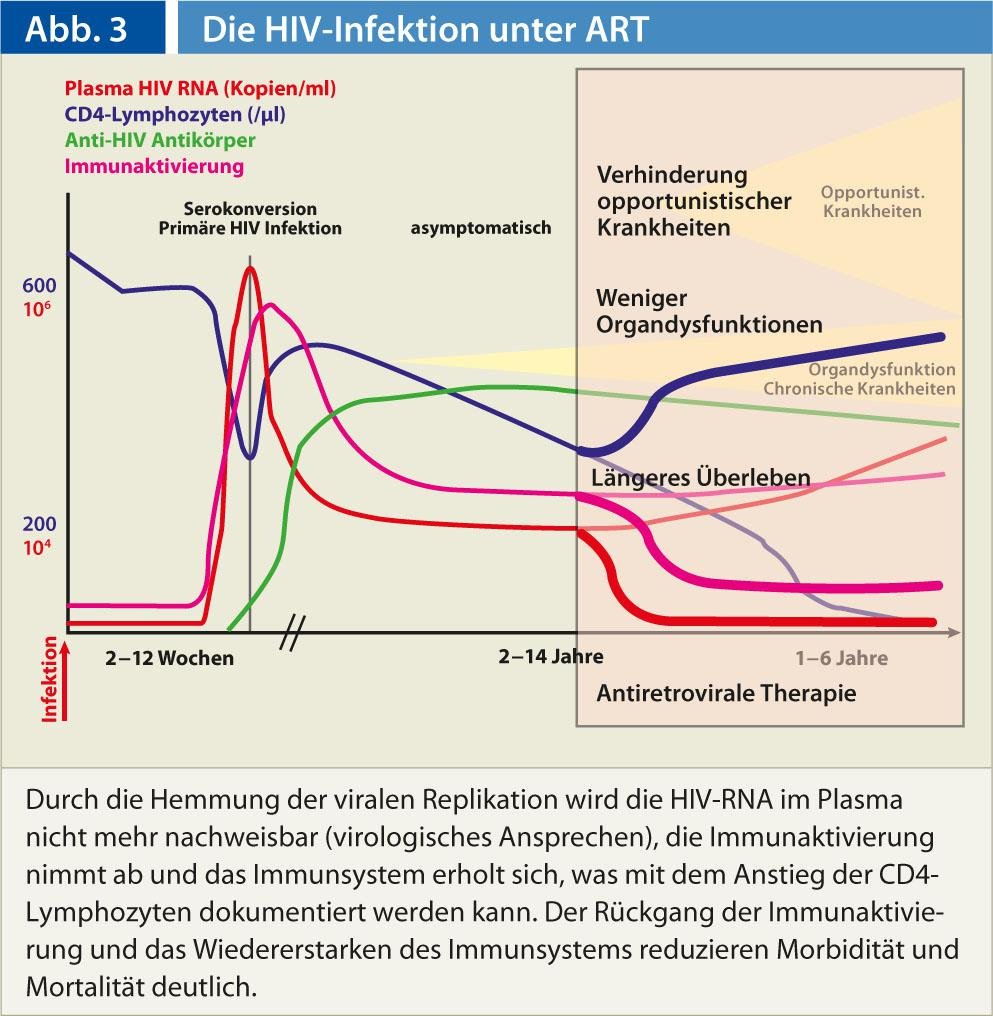
In asymptomatic patients, ART is intended to prevent the morbidity and mortality of HIV infection; therefore, it is used before the onset of opportunistic diseases. It must be continued for life. In the early stages of HIV infection, when CD4 lymphocyte counts are high, complications are very rare. However, in many HIV-infected individuals, there is measurable activation of the immune system even in this “asymptomatic” phase (Fig. 1), which, like all chronic inflammatory states, is likely to be associated with organ dysfunction in the longer term. With decreasing CD4 lymphocytes to levels below 350/µL, the higher incidence of such dysfunctions, e.g. cardiovascular disease, becomes measurable. In a randomized trial, a survival benefit resulted for starting therapy above this level versus waiting until CD4 cells fall below 250/µL [1].
Data from randomized trials that would show a survival benefit of starting ART in asymptomatic patients with CD4 lymphocytes above 350/µL or even above 500/µL are not available. A larger American observational study, which believed to show such [2], could not be verified in European cohorts [3, 4].
Proponents of starting therapy earlier argue that suppression of HIV replication reduces immune activation and that the benefits of this therapy outweigh the disadvantages of potential long-term side effects of ART.
The decision for an early therapy should be made individually, especially clinical symptoms have to be looked for and the individual course (virus replication, CD4 drop e.g. within one year) has to be considered. On the other hand, the annual costs of ART of more than CHF 15 000 per patient must also be taken into account.
A large, global, randomized trial comparing early therapy initiation with CD4 cells above 500/µL with ART initiation when CD4 cells fall below 350/µL (http://insight.ccbr.umn.edu/start/) has been recruiting since 2008. Until the results of this study are available in 2016, the indication for early ART initiation in asymptomatic patients remains a “matter of faith.”
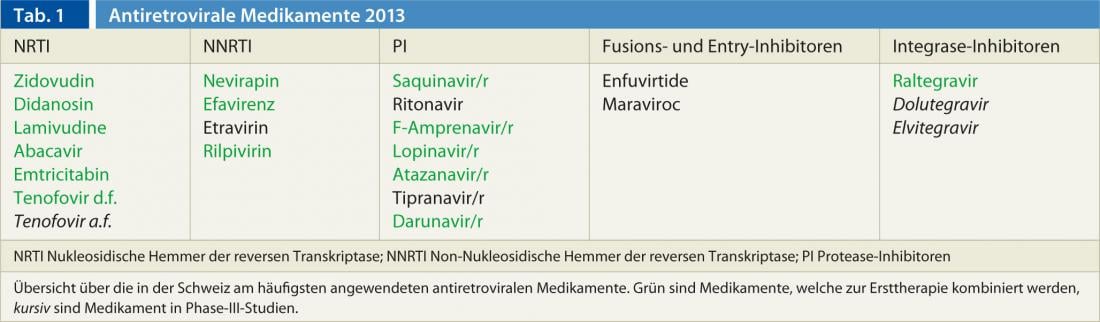
Choice of ART? The choice of antiretroviral drugs available in Switzerland is wide (Table 1) . Usually, three drugs are combined, typically two NRTIs and one PI/NNRTI or integrase inhibitor. Before starting therapy, resistance testing must be performed to ensure that the selected drugs are effective against the viral strains in the patient. The side effect and complex interaction profile of the selected drugs must be adapted to the patient’s diseases, metabolic risk profile, and daily routine.
There are some combination preparations on the market, so that the number of tablets per day can often be kept small. However, with these combination preparations, attention must be paid to the different pharmacokinetics, especially in renal insufficiency, and to the different interaction profiles of the individual substances. Given the individualization of the regime to be chosen, the initiation of ART in Europe should be left to the experts (www.europeanaidsclinicalsociety.org/images/stories/EACS-Pdf/EacsGuidelines-v6.1-2edition.pdf).
Care of patients on ART: Patients on antiretroviral therapy are monitored regularly for virologic (plasma HIV RNA), immunologic (CD4 lymphocytes), and clinical response (history, physical examination). Therapy adherence is evaluated at each consultation. By means of medical history, physical examination and targeted laboratory tests, side effects are recorded according to the side effect profile of the substances used.
Because many antiretroviral drugs have a complex potential for interaction, potential interactions must be ruled out before using any other drug, especially including nonprescription and/or herbal preparations (www.hiv-druginteractions.org). Care is typically provided in the closest collaboration between primary care providers and specialists. Because the long-term effects of ART cannot be captured in drug registration studies, HIV patients should be included in long-term observational studies. The Swiss HIV Cohort Study (www.shcs.ch) is one of the world’s best studies in this regard, prospectively enrolling HIV-infected individuals since 1988.
Treatment of primary, acute HIV infection
Two to approximately ten weeks after infection, the clinical picture of acute or primary HIV infection develops (Fig. 1), a febrile self-limited disease [5]. Within the first few days of this phase of the disease, there is the possibility of stopping the spread and fixing of the virus in the body, which can potentially lead to a functional cure of HIV infection. This unique opportunity for treatment is often missed, either because this condition is not thought of or because the immediate referral to specialists for diagnosis and ART start within a few days is not made.
Treatment of the potential source of HIV infection
Prevention of vertical HIV infection: successful ART of a pregnant woman resulting in undetectable plasma HI viremia in the last weeks of pregnancy prevents vertical perinatal transmission of the virus to the child. Therefore, every woman must be tested for HIV in early pregnancy so that ART can be started in a timely manner. If the risk persists during pregnancy, the HIV test should be repeated before the due date.
Treatment of the HIV-infected sexual partner: In 2008, Swiss experts published the statement that HIV-infected people without other sexually transmitted diseases are not sexually infectious under effective ART [6]. This “Swiss Statement”, which is becoming known worldwide, could be confirmed by a large randomized study [7]. This finding is a great relief, especially for sero-discordant couples who wish to have a child, as nothing more stands in the way of a pregnancy from a medical point of view. The aforementioned study included mainly heterosexual couples. The proof that the “Swiss Statement” also applies to male homosexual sero-discordant couples is therefore pending. Certainly, however, the infectivity of successfully treated homosexual men is significantly reduced by successful ART.
A common question today is whether an HIV-infected person with high CD lymphocyte counts who does not have an indication for ART should be treated antiretrovirally to reduce their infectivity. Sexual transmission of HIV can also be prevented by condoms highly efficiently, without side effects and much cheaper. In individual cases, adherence to ART may be significantly better than to condoms and could argue for the use of ART. Some epidemiologists even question whether all persons should not be tested for HIV and HIV-infected persons treated equally. This could put a stop to the HIV epidemic: “Test and Treat”.
Post-exposure prophylaxis (PEP)
After significant exposure to HIV, through needle stick in hospital or through unprotected sexual contact with an HIV-infected partner, ART should be initiated as soon as possible, i.e. preferably within a few hours, for four weeks. This can reduce the risk of infection by more than 80%.
Pre-exposure prophylaxis (PrEP)
It is known from animal studies that antiretroviral therapy before and after SIV exposure can prevent infection. Several large placebo-controlled randomized trials have examined this strategy. In several of these studies, the preventive efficacy of antiretroviral agents was insufficient. This was mainly attributed to poor treatment adherence. And really, in a study in sero-discordant couples with better treatment adherence, the protective effect was greater [8, 9]. Pre-exposure prophylaxis is currently not a service subject to compulsory health insurance in Switzerland.
Conclusion for practice
- Combination antiretroviral therapy (ART) has transformed HIV infection from a “death sentence” to a treatable disease. The selection of the three components of ART should be made by experts.
- The primary care physician should be aware of the complex and potentially dangerous interaction profile of antiretroviral medications.
- He should also know that ART prevents HIV transmission from mother to child and therefore every pregnant woman should be tested for HIV.
- The two emergency indications for ART are: treatment of acute primary HIV infection and post-exposure prophylaxis.
Prof. Dr. med. Hansjakob Furrer
Literature:
- Emery S, et al: Major clinical outcomes in antiretroviral therapy (ART)-naive participants and in those not receiving ART at baseline in the SMART study. J Infect Dis 2008; 197(8): 1133-1144.
- Kitahata MM, et al: Effect of early versus deferred antiretroviral therapy for HIV on survival. N Engl J Med 2009; 360(18): 1815-1826.
- Sterne JA, et al: Timing of initiation of antiretroviral therapy in AIDS-free HIV-1-infected patients: a collaborative analysis of 18 HIV cohort studies. Lancet 2009; 373(9672): 1352-1363.
- Cain LE, et al: When to initiate combined antiretroviral therapy to reduce mortality and AIDS-defining illness in HIV-infected persons in developed countries: an observational study. Ann Intern Med 2011; 154(8): 509-515.
- Aceto L, et al: [Primary HIV-1 infection in Zurich: 2002-2004]. Schweiz Rundsch Med Prax 2005; 94(32): 1199-1205.
- Vernazza P, et al: AIDS Clinical and Therapeutic Expert Committee. HIV-infected people without other STDs are sexually noninfectious under effective antiretroviral therapy. Swiss Medical Journal 2008; 89(5): 165-169.
- Cohen MS, et al: Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011; 365(6): 493-505.
- Cohen MS, Baden LR: Preexposure prophylaxis for HIV-where do we go from here? N Engl J Med 2012; 367(5): 459-461.
- Okwundu CI, Uthman OA, Okoromah CA: Antiretroviral pre-exposure prophylaxis (PrEP) for preventing HIV in high-risk individuals. Cochrane Database Syst Rev 2012;7:CD007189.











