Myocardial perfusion studies using single-photon emission computed tomography (SPECT) and positron emission tomography (PET) are established methods with high diagnostic accuracy for noninvasive ischemia diagnosis in suspected and known CAD. PET and SPECT are also playing an increasing role in the evaluation of infiltrative and inflammatory diseases.
Cardiac imaging has shown rapid development in recent years and has established itself as an important cornerstone in everyday cardiology. The introduction of the first gamma camera or scintigraphy occurred in the 1950s. This makes myocardial scintigraphy, along with echocardiography, one of the oldest and most established noninvasive imaging modalities worldwide with correspondingly extensive long-term data. Technical advances in recent years have expanded the areas of application of nuclear medicine examination methods in cardiology. While for a long time the main application of single-photon emission computed tomography (SPECT) and positron emission tomography (PET) in cardiology was the evaluation of patients with known or suspected coronary artery disease (CAD), other indications have recently gained importance, such as the detection of sources of infection (including endocarditis), and the evaluation of infiltrative and inflammatory diseases (e.g., amyloidosis, sarcoidosis). While myocardial SPECT is widely used and relatively inexpensive, PET has the higher temporal and spatial resolution, allows quantification of myocardial blood flow, and thus has been instrumental in providing insight into the pathophysiological regulation of myocardial circulation.
Basics and technical aspects
SPECT: Myocardial perfusion SPECT is based on the principle of radionuclide uptake into viable myocytes and detection of gamma radiation emitted during decay. Today, the nuclide 99mTechnetiumis mainly used for this purpose, bound to the “tracers” sestamibi or tetrofosmin. In contrast to 201Thallium, 99mTechnetiumallows better image quality with lower radiation exposure. The latter could be significantly reduced, especially with the advent of modern semiconductor detector technology based on cadmium-zinc-tellurite alloys, and is currently in the range of 2-5 mSv [1].
Exercise can be done medicinally (dobutamine or adenosine) or physically by ergometry. Exercise-induced or resting perfusion deficits allow the detection of ischemia or myocardial scar, respectively, and thus the detection of coronary artery disease with high diagnostic accuracy. Prognostic data from many thousands of patients are available for SPECT, highlighting the role of this method also for risk stratification of patients with CHD [2].
PET: PET examination is also based on the detection of radioactive decay. However, the method differs fundamentally from SPECT in terms of the type of radionuclides used: Whereas for myocardial perfusion SPECT, radionuclides with gamma decay and relatively long half-lives (e.g., 6 h for 99mtechnetium) are used, those used in myocardial perfusion PET are those with β+ decay and comparatively short half-life (e.g., 10 min for 13N-ammonia), which implies the availability of a cyclotron for their immediate on-site production; an exception is 82rubidium, which can be produced by means of a generator. The resolution of PET is significantly better than that of SPECT, resulting in PET offering one of the highest diagnostic values of all imaging modalities [3]. In addition, PET allows absolute quantification of myocardial blood flow in ml/min/g, which allows detection of coronary three-vessel disease or microcirculatory dysfunction [4]. The radiation exposure of a 13N-ammoniamyocardial perfusion study is only 1-3 mSv due to its short half-life.
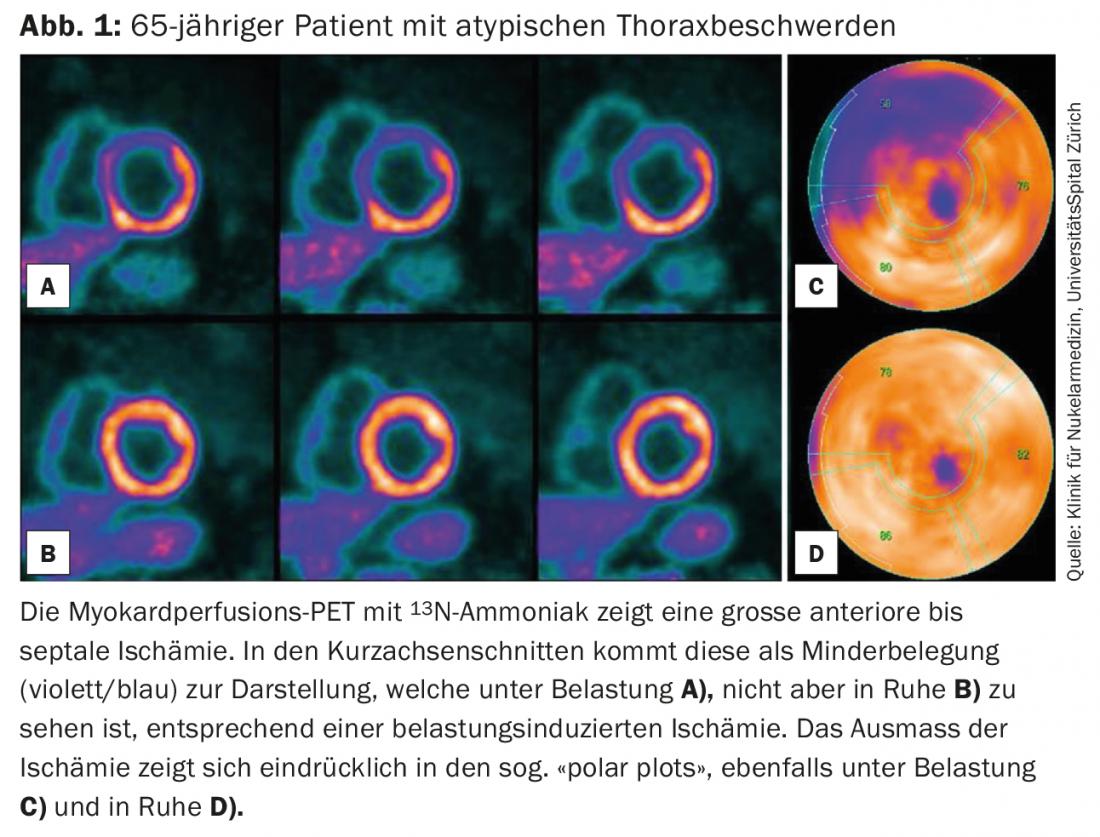
Alternatively or complementary to perfusion (Fig. 1) , PET can also be used to obtain information on metabolism using other tracers, especially 18F-fluorodeoxyglucose(FDG), depending on the protocol used. Thus, viable – and thus metabolically still active – myocytes in an infarcted myocardial area can be visualized, which allows stratification with regard to the expected prognosis or the indication for revascularization of the corresponding myocardial area. Alternatively, 18F-FDGPET can be used to detect increased metabolism in active inflammation, eg, myocardial in myocarditis or sarcoidosis or cardiac/extracardiac in endocarditis and/or device-associated infections.
Ischemia diagnostics in clinical routine with SPECT and PET
Myocardial perfusion SPECT as well as myocardial perfusion PET are established methods for ischemia diagnosis in routine clinical practice – indicated in patients with known or suspected CHD [5]. The ESC (European Society of Cardiology) guidelines recommend SPECT or PET scanning in symptomatic patients with an intermediate pretest probability (15-85%) regarding CHD (details in Fig. 2) [3]. These nuclear cardiac functional noninvasive tests allow assessment of myocardial perfusion disturbance and evaluation of infarct scars by recording under resting and stress conditions. In addition, left ventricular volumes in systole and diastole, as well as ejection fraction and wall motion can also be assessed. 18F-FDGPET is also another investigative method available for evaluating myocardial viability [6].
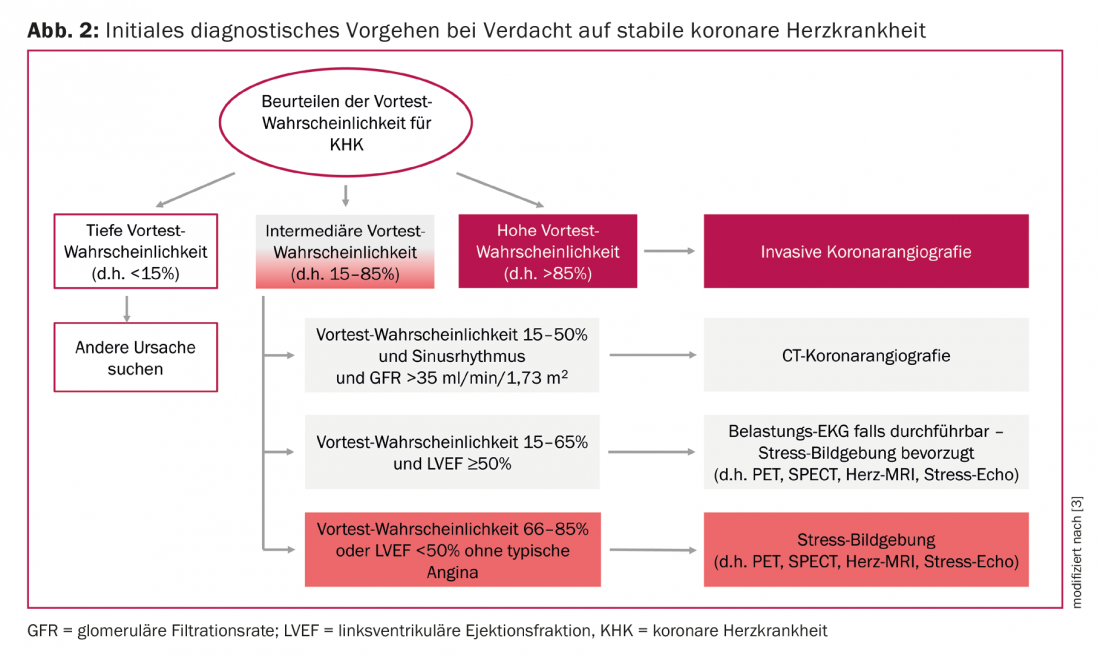
The extent of ischemia is relevant with regard to indication for revascularization. If there is a strain-induced circulatory disturbance of more than 10%, the patient will benefit from invasive revascularization in terms of long-term prognosis [7]. In patients with smaller ischemic area, revascularization has no prognostic benefit compared with a conservative strategy with optimal drug therapy. Accordingly, the guidelines recommend evidence of ischemia in patients with stable heart disease before any intervention [3].
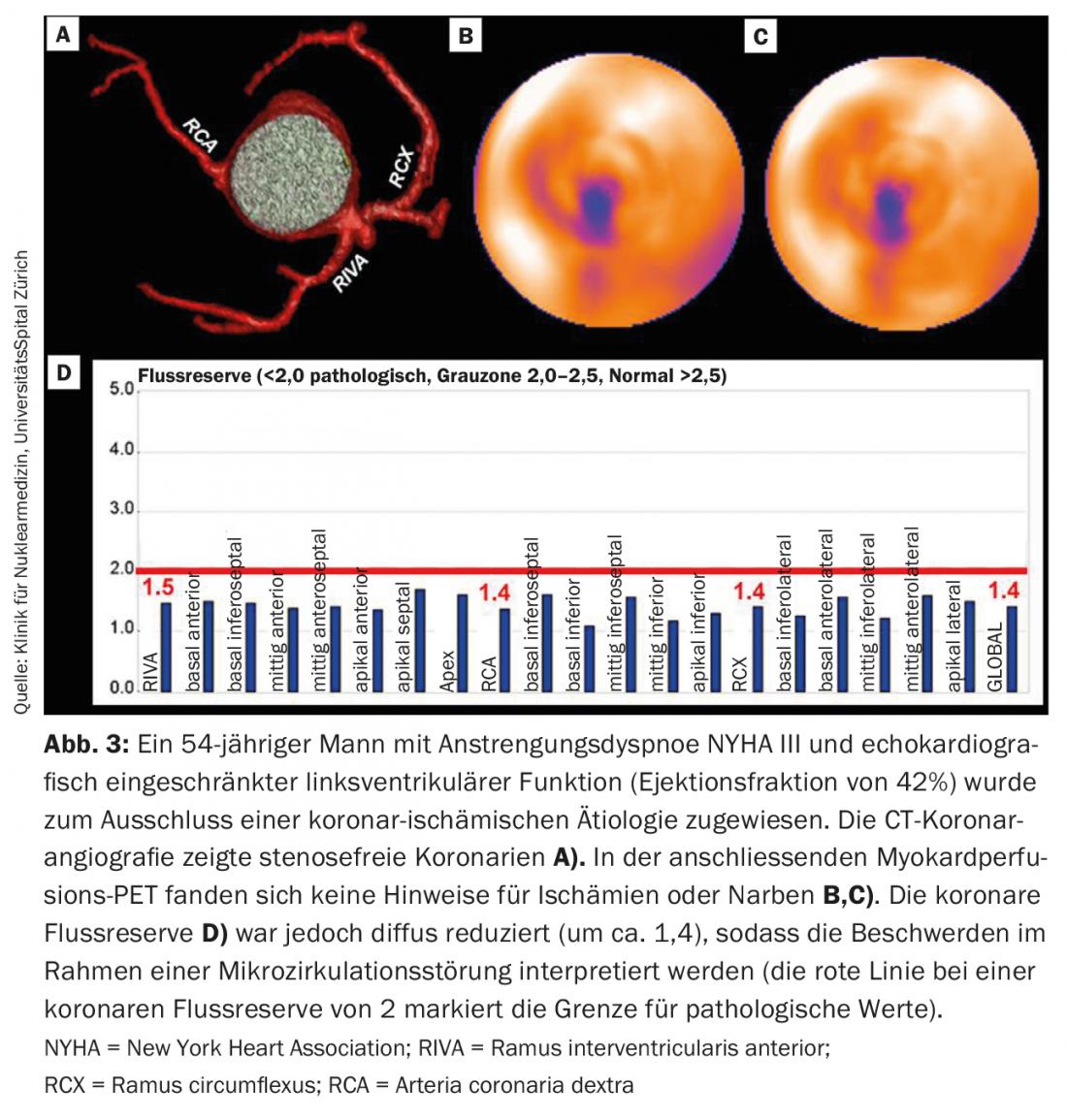
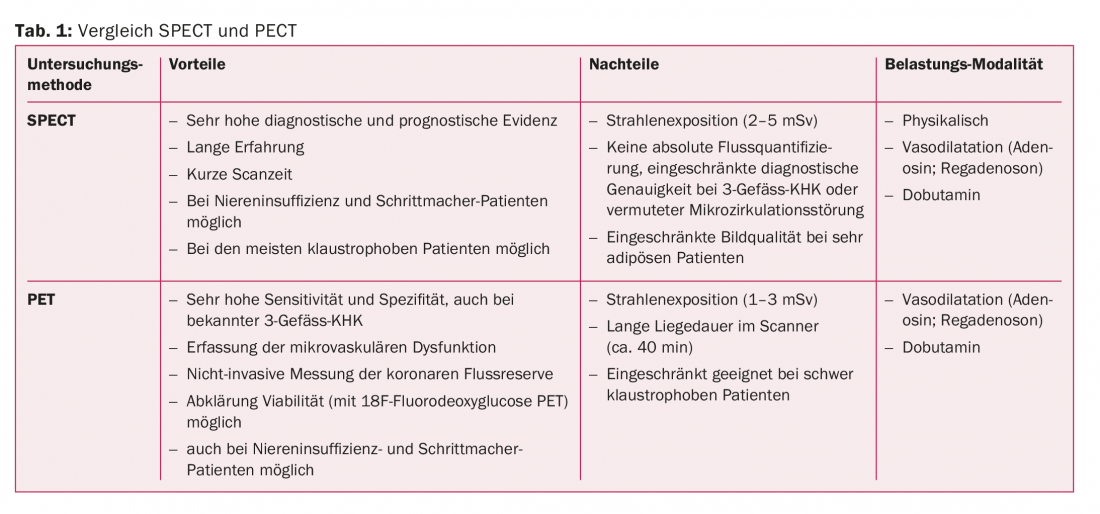
Compared with SPECT, PET examination has a higher sensitivity and specificity with regard to the assessment of relevant CHD [3]. Further, PET examination has the advantage of noninvasively assessing coronary flow reserve. The latter represents another important independent risk marker in addition to perfusion [8]. PET thus offers significant advantages, particularly in coronary three-vessel disease, in diabetics with diffuse involvement of CHD, and in microcirculatory disorders (Fig. 3). Table 1 presents the advantages and disadvantages of the two examination methods SPECT and PET.
To achieve optimal image quality, native computed tomography (CT) is performed in addition to SPECT/PET acquisition for attenuation correction [9]. In addition to attenuation correction, this native CT also allows simultaneous acquisition of calcium score, which is another established risk marker. The calcium score can thus be included in the assessment without additional uptake.
Hybrid imaging
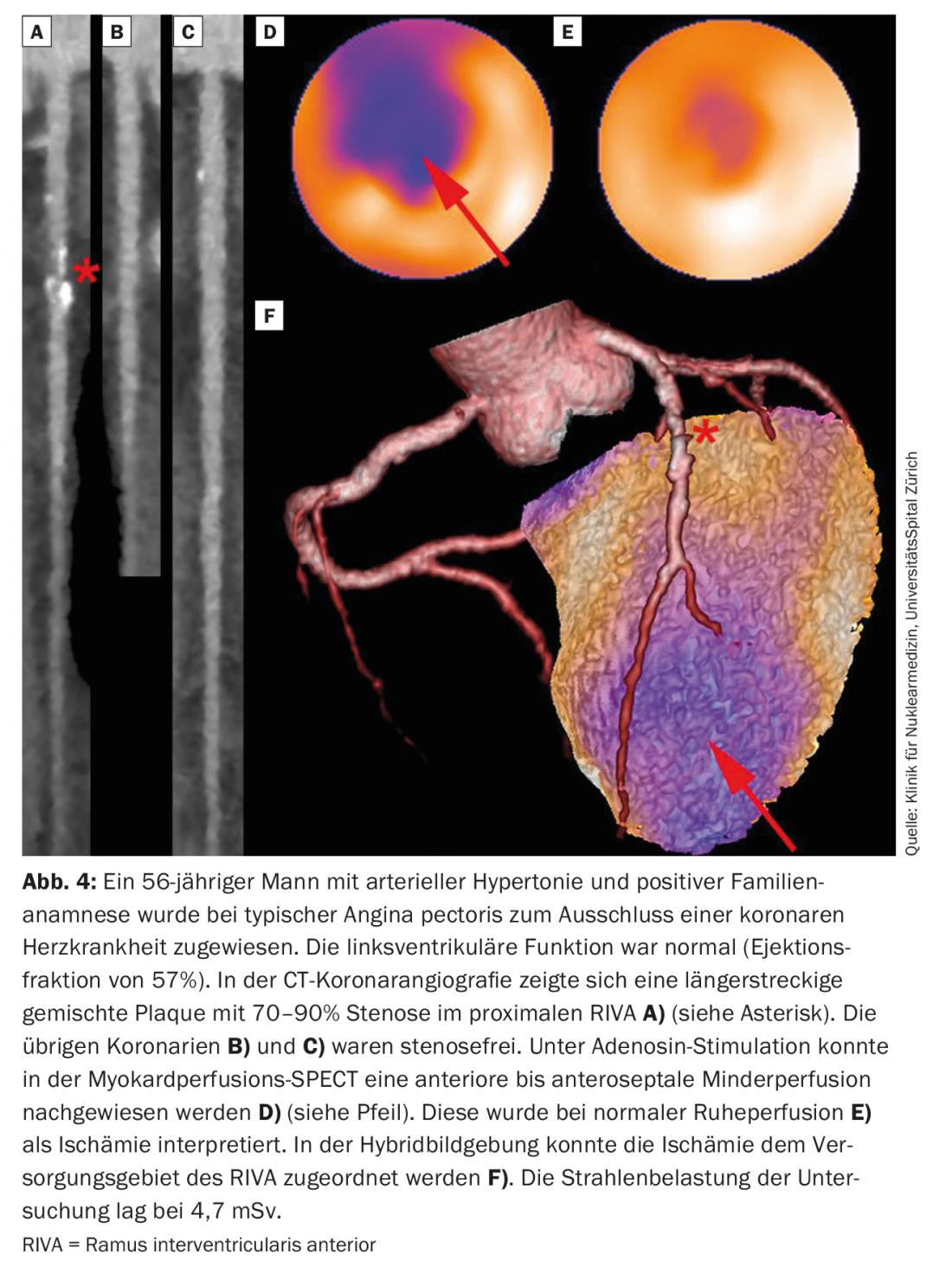
Hybrid imaging is described as the process of fusing two multimodal data sets. Ideally, a combination of an anatomic examination (e.g., coronary CT) and a functional examination (e.g., myocardial perfusion PET or SPECT) should be performed to obtain the best possible information. In this process, the data sets can be acquired on two different scanners and then fused to form a hybrid image. Hybrid imaging using coronary CT and SPECT or PET is particularly useful in patients with multivessel disease (including after bypass surgery) and significant side-branch stenoses by allowing accurate co-localization of the stenosed coronary artery to the respective ischemic myocardial territory (Fig.4). In addition to a high diagnostic accuracy, the prognostic significance of this examination has also been demonstrated [10]. This showed that patients with congruent findings (coronary stenosis with ischemia in the corresponding supply area) have a significantly worse prognosis than patients with incongruent findings (e.g., stenosis without ischemia) or patients with normal findings.
Non-ischemic cardiac clinical pictures
Infiltrative diseases: Sarcoidosis and Amyloidosis: 18F-FDGPET is an established modality in the workup of cardiac sarcoidosis, due to its excellent diagnostic and prognostic value [11]. In addition, however, PET as a quantitative imaging modality also allows accurate determination of metabolic/inflammatory activity, which underscores its utility in the context of therapy monitoring [12]. However, an important prerequisite for this examination is optimal patient preparation to prevent physiological FDG accumulation in the myocardium, which would limit the specificity of the examination. This includes in particular a strict carbohydrate-free diet, if necessary combined with intravenous heparin administration.
Less well known is the possibility of clarifying suspected cardiac amyloidosis by means of easily available and relatively inexpensive skeletal scintigraphy. This fact is surprising, considering the excellent sensitivity of this study. Indeed, skeletal scintigraphy has been shown to have a 100% positive predictive value for cardiac ATTR (familial transthyretin amyloidosis) amyloidosis after exclusion of AL amyloidosis (no monoclonal proteins in urine or blood) and with inclusion of the pattern of accumulation in myocardium and other soft tissues [13]. Therefore, recent studies question the necessity of myocardial biopsy for diagnosis [13].
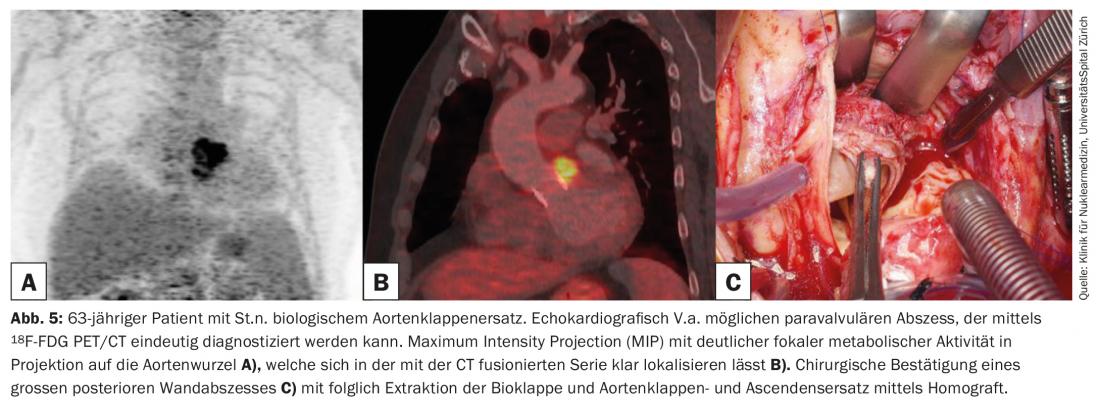
Endocarditis/Device Infections: The current European Society of Cardiology (ESC) guidelines recently list 18F-FDGPET as a major criterion in the diagnosis of suspected endocarditis in prosthetic valves and recommend its use in cases of inconclusive echocardiography [14]. This is again due to the high sensitivity of this modality for inflammation in the area of prostheses (Fig. 5), but also due to the possibility of simultaneously identifying septic emboli – which are found in more than 50% of cases [15], and last but not least due to the possibility of detecting potential ports of entry. In contrast, in the setting of native valves, 18F-FDGPET is not suitable for endocarditis because of the inadequate low sensitivity there, primarily because of the mobility and small size of vegetations on native valves. Comparable to endocarditis is also the role of 18F-FDGPET in questionable device infections.
Summary
In conclusion, noninvasive imaging using nuclear medicine examinations has contributed essentially to the understanding of coronary artery disease and is nowadays a cornerstone of cardiac diagnostics. In addition to its long-established role in ischemia and viability diagnostics, nuclear cardiology has become increasingly important in the search for sources of infection (e.g., endocarditis) and the evaluation of infiltrative and inflammatory diseases (e.g., amyloidosis, sarcoidosis).
Take-Home Messages
- Myocardial perfusion studies using single-photon emission computed tomography (SPECT) and positron emission tomography (PET) are established methods with high diagnostic accuracy for noninvasive ischemia diagnosis in suspected and known coronary artery disease.
- PET has the advantage over SPECT of detecting coronary flow reserve with lower radiation exposure and is the method of choice especially in cases of known coronary 3-vessel disease.
- Hybrid imaging (coronary CT plus SPECT or PET) allows simultaneous acquisition of both coronary anatomy and functional information.
- 18F-FDGPET is listed in the current guidelines as a major criterion in the diagnosis of suspected endocarditis in prosthetic valves.
- PET and SPECT are playing an increasing role in the evaluation of infiltrative and inflammatory diseases (e.g., amyloidosis, sarcoidosis).
Disclosure: The University Hospital Zurich holds a research contract with GE Healthcare.
Literature:
- Acampa W, Buechel RR, Gimelli A: Low dose in nuclear cardiology: state of the art in the era of new cadmium-zinc-telluride cameras. Eur Heart J Cardiovasc Imaging 2016; 17(6): 591-595.
- Shaw LJ, Iskandrian AE: Prognostic value of gated myocardial perfusion SPECT. Journal of nuclear cardiology: official publication of the American Society of Nuclear Cardiology 2004; 11(2): 171-185.
- Task Force M, et al: 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 2013; 34(38): 2949-3003.
- Fiechter M, et al: Diagnostic value of 13N-ammonia myocardial perfusion PET: added value of myocardial flow reserve. Journal of nuclear medicine: official publication, Society of Nuclear Medicine 2012; 53(8): 1230-1234.
- Acampa W, et al: Role of risk stratification by SPECT, PET, and hybrid imaging in guiding management of stable patients with ischaemic heart disease: expert panel of the EANM cardiovascular committee and EACVI. European heart journal cardiovascular Imaging 2015; 16(12): 1289-1298.
- Gaemperli O, Kaufmann PA: PET and PET/CT in cardiovascular disease. Ann N Y Acad Sci 2011; 1228: 109-136.
- Hachamovitch R, et al: Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 2003; 107(23): 2900-2907.
- Herzog BA, et al: Long-term prognostic value of 13N-ammonia myocardial perfusion positron emission tomography added value of coronary flow reserve. J Am Coll Cardiol 2009; 54(2): 150-156.
- Pazhenkottil AP, et al: Improved outcome prediction by SPECT myocardial perfusion imaging after CT attenuation correction. J Nucl Med 2011; 52(2): 196-200.
- Pazhenkottil AP, et al: Prognostic value of cardiac hybrid imaging integrating single-photon emission computed tomography with coronary computed tomography angiography. Eur Heart J 2011; 32(12): 1465-1471.
- Youssef G, et al: The use of 18F-FDG PET in the diagnosis of cardiac sarcoidosis: a systematic review and metaanalysis including the Ontario experience. Journal of nuclear medicine: official publication, Society of Nuclear Medicine 2012; 53(2): 241-248.
- Lee PI, Cheng G, Alavi A: The role of serial FDG PET for assessing therapeutic response in patients with cardiac sarcoidosis. Journal of nuclear cardiology: official publication of the American Society of Nuclear Cardiology 2017; 24(1): 19-28.
- Gillmore JD, et al: Nonbiopsy Diagnosis of Cardiac Transthyretin Amyloidosis. Circulation 2016; 133(24): 2404-2412.
- Habib G, et al: 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). European heart journal 2015; 36(44): 3075-3128.
- Salomaki SP, et al: (18)F-FDG positron emission tomography/computed tomography in infective endocarditis. Journal of nuclear cardiology: official publication of the American Society of Nuclear Cardiology 2017; 24(1): 195-206.
CARDIOVASC 2018; 17(2): 4-9