Onychomycosis diagnosis by histology and/or culture is mandatory before any systemic therapy. Topical therapy is sufficient if nail infestation is less than 50% without matrix infestation. Dermatophytes are among the most common fungal pathogens. The first-choice agent for systemic therapy is terbinafine. Systemic therapy should always be combined with topical therapy. Patient education on hygiene measures is required.
Nail fungal infection (onychomycosis) is a common dermatologic condition affecting up to 20% of adults. The toenails are much more commonly affected than the fingernails, and affected individuals most commonly present with interdigital foot mycosis. Single, several or rarely all nails may be affected. Pathogens include dermatophytes (filamentous fungi) and molds and yeasts. Onychomycoses of the toes are mainly caused by dermatophytes (most common representative Trichophyton rubrum), while onychomycoses of the fingers are more often caused by yeasts [1–3].
How does onychomycosis occur?
As a rule, predisposing factors must be present for nail fungal disease to occur. These include genetic predisposition, age, and angio- and polyneuropathy. Tinea pedis is almost always present at the same time. Furthermore, a warm and humid environment, recurrent trauma, diabetes mellitus, immunodeficiency, nail psoriasis as well as eczema of the foot can promote nail fungus [4,5].
Clinic
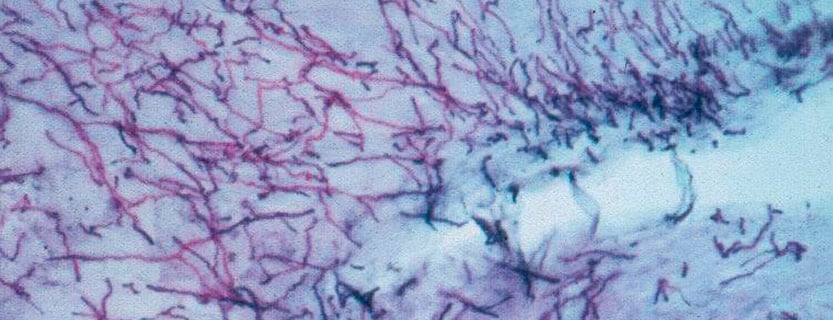
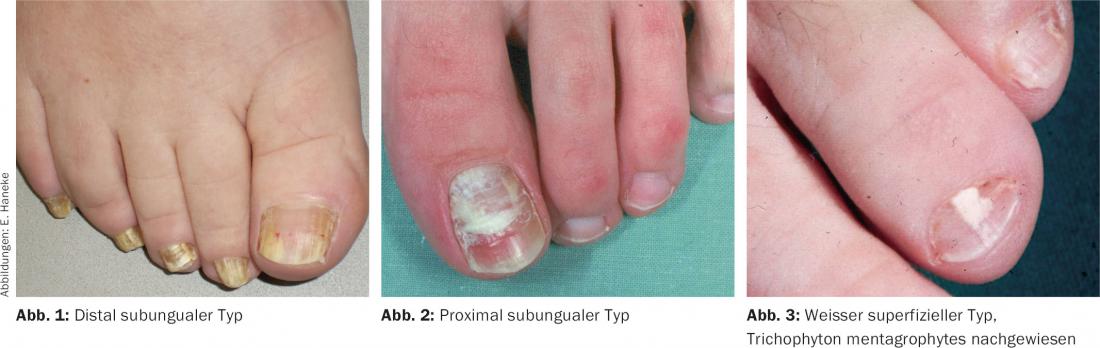
The disease usually begins with subungual hyperkeratosis, where the main mass of fungi is located. Later, the nail plate turns whitish-yellowish-brown. In the later course, crumbly decay of the nail may occur. This indicates a complete infestation of the nail bed and matrix, from where the fungi invade the nail plate. Different types are distinguished depending on the route of infection:
- Distal subungual type: 90% of cases, most common pathogen Trichophyton rubrum (Fig. 1).
- Proximal subungual type (Fig. 2)
- White superficial type, in Central Europe mainly caused by Trichophyton mentagrophytes (Fig. 3).
- Endonyx type: Infestation of the interior of the nail plate, leaving the nail surface and bed intact; preferably by Trichophyton soudanense or Trichophyton violaceum.
- Total dystrophic onychomycosis (end stage)
Differential diagnosis should include nail psoriasis, lichen ruber, eczema and post-traumatic nail changes.
Diagnostics
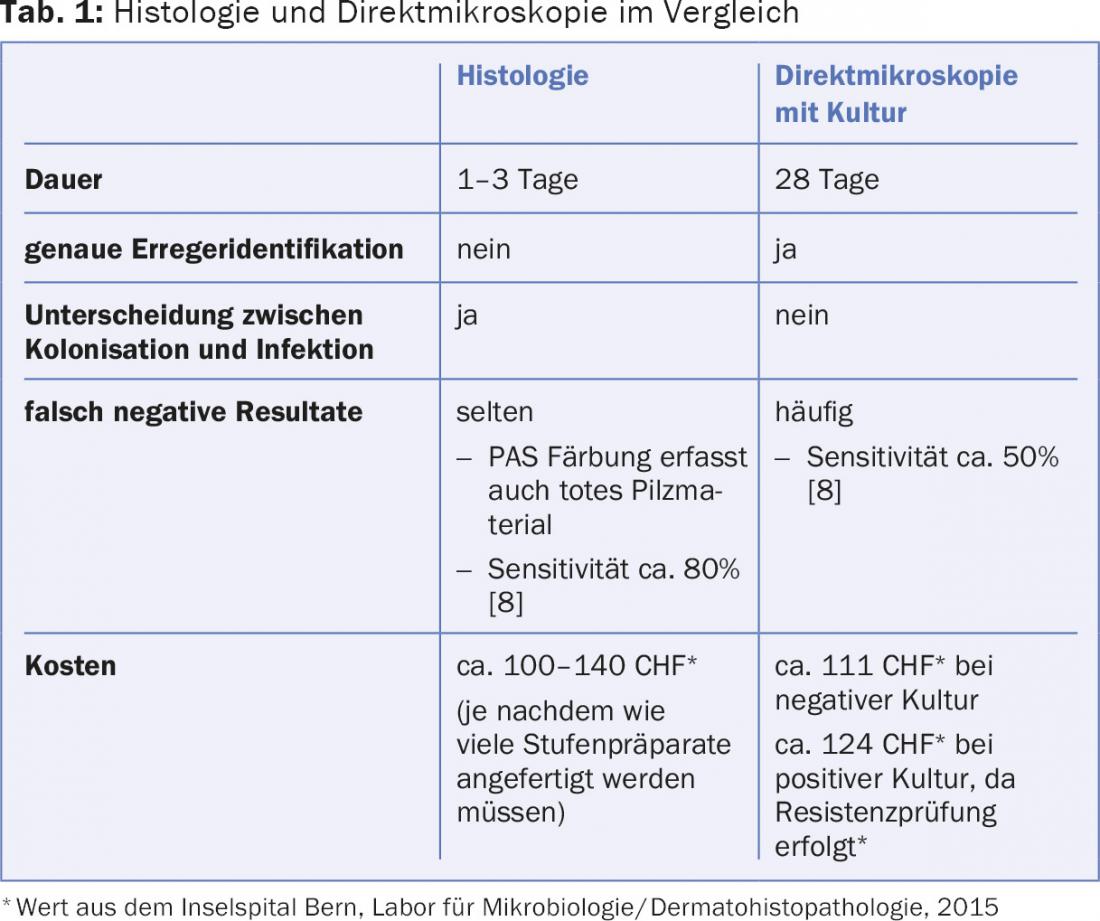
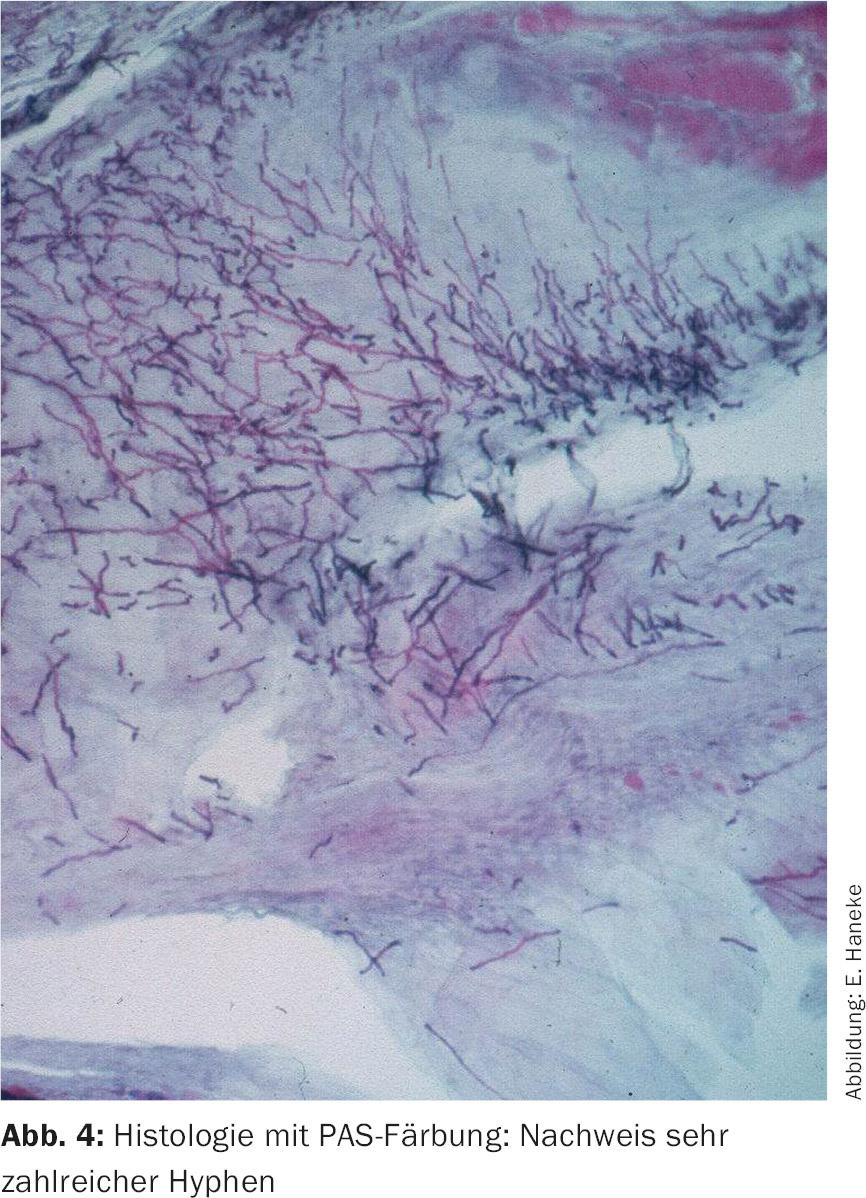
Laboratory diagnosis is optional before topical therapy, but mandatory before any systemic therapy. Two examination procedures have become established in the meantime. One is histology and the other is direct microscopy with culture. Histology allows differentiation between colonization and infection (Fig. 4) . Culture allows the exact determination of the pathogen. The main advantages and disadvantages of both methods are listed in Table 1 . Because of the frequently false-negative results of culture, we recommend histology as a diagnostic procedure. In complex cases, both diagnostic measures can be performed.
How to obtain nail material? In the distal subungual type, material is obtained from the nail bed under the affected nail for culture, and the nail with the nail bed keratosis is obtained for histology. For the remaining types of onychomycosis, the nail material can be obtained by punch biopsy. This does not require local anesthesia, but the necessary sensitivity to avoid nail bed injuries. The nail plate should be removed beforehand for min. Soak for 10 minutes with a lukewarm hand or foot bath.
Therapy
Does onychomycosis need to be treated? A nail fungus disease can, but does not always have to be treated. For the patient, onychomycosis is often a cosmetic problem. However, pain may also occur, limiting the patient’s athletic activity [6]. It should not be forgotten that onychomycosis is an infectious disease. The fungus can spread to the surrounding skin as well as to the other nails and in individual cases lead to total onychodystrophy of all nails. Furthermore, there is a risk of infecting contact persons. In the presence of concomitant diabetes mellitus or immunosuppression, onychomycosis may promote bacterial infection such as erysipelas [7].
Treatment is quite reasonable and desirable in young patients to prevent nail dystrophy and/or recurrent cutaneous mycoses. In older patients, it is perfectly reasonable to refrain from treatment. The decision for systemic therapy should be made individually depending on the level of suffering (pain? cosmetically disturbing?), age, comorbidities (known liver disease? Ipsilateral recurrent erysipelas?), after clarification of the side effect profile and the high recurrence rate.
Practical therapy tips: Therapy requires perseverance and good patient compliance. Hygiene measures such as regular washing of socks and towels at at least 60°C (better 95°C) and keeping feet dry are recommended. The affected nail should be removed as far as possible by cutting or filing. If the nail plate is very thick, urea 20-40% in ointment base can be applied occlusively for at least three to five days to soften the nail. Subsequently, the affected area can be removed as atraumatically as possible using scissors or a scalpel.
Topical therapy: If less than 50% of the nail plate is affected and the nail matrix is not affected, topical therapy is often sufficient. Two nail polish preparations have proven effective: Ciclopirox 8% and Amorolfine 5%.
Ciclopirox 8% is applied 1× daily or 1× weekly, depending on the nail varnish: Ciclopoli® nail varnish (application 1×/d), Ciclocutan® nail varnish (application every other day in the first month, 2×/week in the second month, 1×/week from the third month).
Amorolfine 5% is applied 1-2×/week.
The duration of therapy with both active substances is at least 9-12 months for toenails and at least six months for fingernails.
Systemic therapy: If more than 50% of the nail plate or the nail matrix is affected, systemic therapy can be applied after positive fungal detection by histology and/or culture (Tab. 2).
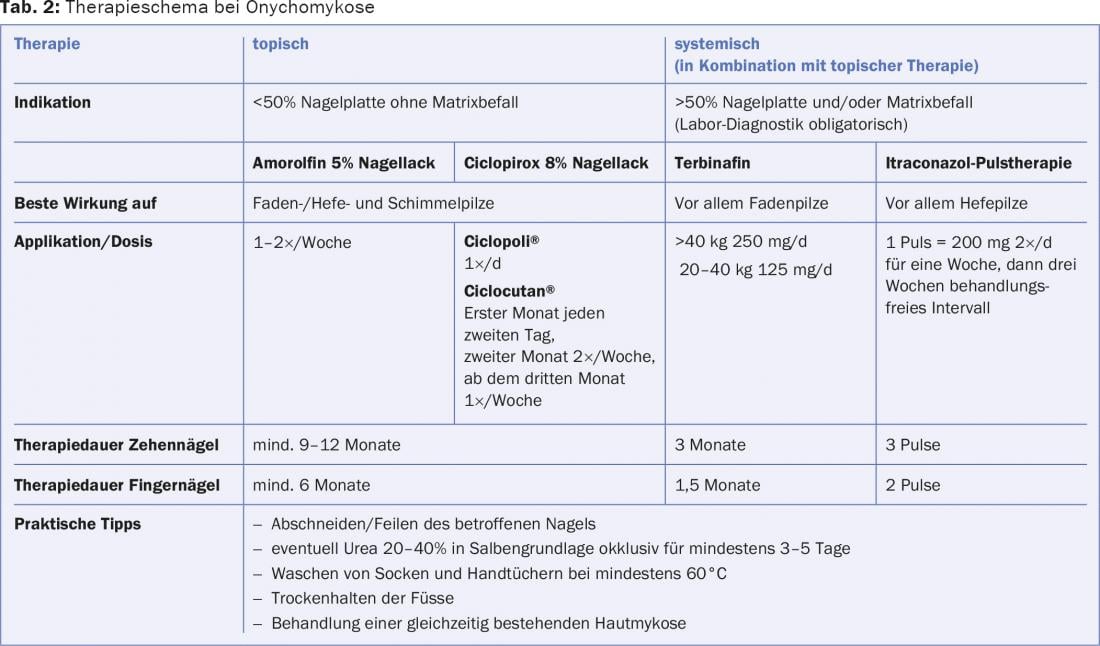
First-line agent for systemic therapy is terbinafine (>40 kg 250 mg/d, 20-40 kg 125 mg/d). The duration of therapy is three months for toenails and 1.5 months for fingernails. Terbinafine has a broad spectrum of activity and is most effective against Trichophyton rubrum, the most common nail fungus in Europe. The drug is basically well tolerated and has the lowest recurrence rate. The most common side effects include headache and nausea. However, it may also cause reversible taste disturbances and skin lesions (exanthema, psoriasis, subacute lupus) and hepatitis (frequency 1/1000-10,000). Liver enzyme monitoring (ASAT/ALAT) is recommended prior to initiation of therapy and every four to six weeks during therapy. If liver enzymes are elevated, the drug should not be given or should be discontinued. In renal insufficiency with a glomerular filtration rate below 50%, terbinafine therapy is not recommended because insufficient data are available.
Itraconazole is considered second-line therapy for dermatophyte but first-line therapy for Candida infections. Pulse therapy is preferable to continuous therapy because it is considered more effective, has fewer side effects, and is less expensive.
- Pulse therapy: one pulse = 200 mg 2×/d for one week, then three weeks treatment-free interval. Therapy duration of toenails three pulses, for fingernails two pulses.
- Continuous therapy: 100 mg 2×/d. Therapy duration of toenails three months, fingernails 1.5 months.
Alternatively, fluconazole 150-450 mg/week can be used until the onychomycosis heals. Liver enzyme monitoring is recommended with continuous itraconazole as well as fluconazole therapy.
Due to frequent interactions with other drugs, the patient’s drug list should be clarified regarding interactions with itraconazole and fluconazole (CYP3A4 inhibitors) prior to initiating therapy.
Success/Recurrence Rate: The success rate of terbinafine therapy (primarily fungicidal) is approximately one-half to two-thirds of cases. With itraconazole, which is primarily fungistatic, success is seen in about one-third to one-half of cases.
Systemic therapy should always be combined with topical therapy. This can cut the failure rate in half. Onychomycosis recurrence after successful therapy is observed in approximately one-third to one-half of cases after two years [8–11]. Interval therapy with topical antifungal agents may be attempted to decrease the recurrence rate [12].
Literature:
- Gupta AK, et al: Prevalence and epidemiology of onychomycosis in patients visiting physicians’ offices: a multicenter Canadian survey of 15000 patients. J Am Acad Dermatol 2000; 43: 244.
- Romano C, Gianni C, Difonzo EM: Retrospective study of onychomycosis in Italy: 1985-2000. Mycoses 2005; 48: 42.
- Foster KW, Ghannoum MA, Elewski BE: Epidemiologic surveillance of cutaneous fungal infection in the United States from 1999 to 2002. J Am Acad Dermatol 2004; 50: 748.
- Sigurgeirsson B, Steingrímsson O. Risk factors associated with onychomycosis. J Eur Acad Dermatol Venereol 2004; 18: 48.
- Faergemann J, et al: Genetic predisposition – understanding underlying mechanisms of onychomycosis. J Eur Acad Dermatol Venereol 2005; 19 Suppl 1: 17.
- Elewski BE: The effect of toenail onychomycosis on patient quality of life. Int J Dermatol 1997; 36: 754.
- Roujeau JC, et al: Chronic dermatomycoses of the foot as risk factors for acute bacterial cellulitis of the leg: a case-control study. Dermatology 2004; 209: 301.
- Wilsmann-Theis D, et al: New reasons for histopathological nail-clipping examination in the diagnosis of onychomycosis. J Eur Acad Dermatol Venereol 2011; 25: 235.
- De Cuyper C, Hindryckx PH: Long-term outcomes in the treatment of toenail onychomycosis. Br J Dermatol 1999; 141 Suppl 56: 15.
- Piraccini BM, Sisti A, Tosti A: Long-term follow-up of toenail onychomycosis caused by dermatophytes after successful treatment with systemic antifungal agents. J Am Acad Dermatol 2010; 62: 411.
- Gupta AK, Ryder JE, Johnson AM: Cumulative meta-analysis of systemic antifungal agents for the treatment of onychomycosis. Br J Dermatol 2004; 150: 537.
- Warshaw EM, St Clair KR: Prevention of onychomycosis reinfection for patients with complete cure of all 10 toenails: results of a double-blind, placebo-controlled, pilot study of prophylactic miconazole powder 2%. J Am Acad Dermatol 2005; 53: 717.
DERMATOLOGIE PRAXIS 2015; 26(1): 10-13