Irritable stomach syndrome and irritable bowel syndrome are benign conditions, but can severely limit the quality of life of those affected. Functional flatulence is a common shared characteristic and is considered very bothersome by sufferers. There is no uniform standard therapy; multimodal, symptom-oriented therapy has proven to be effective.
Functional gastrointestinal disorders are common and can be diagnosed using Rome IV criteria in the absence of evidence of other structural disease [1]. The causes are often diffuse, sometimes unfavorable eating habits and stress play a role. Motility disorders and visceral hypersensitivity are critical factors in the pathomechanism. Typical symptoms of functional gastrointestinal complaints are flatulence, abdominal pain or cramps, bloating, diarrhea or constipation.
Symptoms even with normal gas
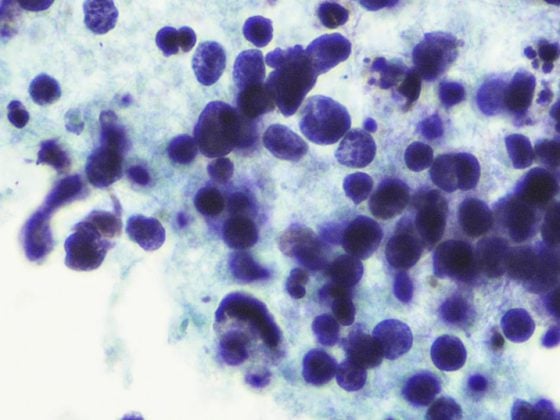
Flatulence is the subjective sensation of a distended abdomen, which is perceived by sufferers as very disturbing. It is a common symptom of various functional diseases of the gastrointestinal tract (Fig. 1) [2–5]. Sometimes there is an objectively detectable increase in abdominal girth, but this is not mandatory. The severity and course of the disease vary from person to person. While in some symptoms remit spontaneously, in others they persist chronically and lead to significant impairment [6]. The pathomechanism is multifactorial; visceral hypersensitivity, behaviorally induced abnormal reflexes, and effects of poorly absorbed fermentable carbohydrates and alterations of the microbiome (e.g., due to infection) are thought to play a role [7]. The modern concept of the gut-brain axis (“brain-gut axis”) refers to the relationship between the peripheral and central nervous systems [8]. In this explanatory model, it is assumed that visceral allodynia leads to the subjective perception of bloating and that this can occur even with normal or only slightly increased gas production [9,10]. The mechanism of visceral hypersensitivity, that is, increased vigilance to specific sensations in the gastrointestinal tract, has long been described as an important pathogenetic factor for flatulence and other functional digestive complaints [5,7,11]. A lower perceptual and pain threshold to intestinal stimuli contributes to central nervous sensitization.
Caraway oil: carminative properties
Therapy is challenging for both practitioners and patients. There is no single strategy for treating functional flatulence; a multimodal symptom-based procedure is most promising. Regarding diet, a low FODMAP diet has been shown in controlled empirical studies to favor a reduction in gastrointestinal symptoms [12]. FODMAPs are fermentable carbohydrates whose absorption is problematic in certain individuals. In addition to dietary changes, behavioral therapy may also be useful, for example, for stress management strategies. It is known that stress can affect the qualitative and quantitative composition of the “microbiome” [13]. Besides the general measures, phytotherapy has also proven to be effective . According to a 2020 publication by Lacy et al. the success of treatment is particularly promoted by the following factors [14]: psychoeducation, support for lifestyle modification, nutritional counseling. Phytotherapeutically, carminative substances, such as caraway, can provide relief. The effect of herbal carminatives is based on relaxation of intestinal muscles and inhibition of gas and foam formation. Caraway oil (Carvi aetheroleum) also has antimicrobial effects, which contributes to reduced gas production by microorganisms [15]. This selectively inhibits the growth of pathogenic germs without exerting negative effects on beneficial intestinal bacteria [15]. Caraway oil also has analgesic effects by reducing visceral sensitivity (TRPA1 receptor). Peppermint oil also has analgesic effects (TRPM8 receptor) as well as a relaxing effect via inhibition of voltage-dependent calcium influx [16]. The high-dose active ingredient combination of peppermint oil and caraway oil contained in the capsule-shaped drug Carmenthin® [17] has been shown to relieve functional digestive disorders such as flatulence, cramps, bloating and epigastric pain.
Literature:
- Stanghellini V, et al: Gastroenterology 2016 pii: S0016-5085(16)00177-3.
- May B, et al: Efficacy and tolerability of a fixed combination of peppermint oil and caraway oil in patients suffering from functional dyspepsia. Aliment Pharmacol Thera 2000; 14: 1671-1677.
- Noe S, et al: An open-label, multicenter, pharmacy-based, prospective cohort study of menthacarin for functional gastrointestinal symptoms. Internist 2016; 57 (Suppl. 1), S42-S42.
- Storr M, Stracke B: Treatment effect and tolerability of menthacarin in patients with functional dyspepsia – an 11-month follow-up. Z Gastroenterol 2017; 55: e220-e220.
- Madisch A, et al: Diagnosis and therapy of functional dyspepsia. Dtsch Arztebl Int 2018; 115: 222-232.
- Kamboj AK, Oxentenko AS: Workup and Management of Bloating. Clin Gastroenterol Hepatol 2018; 16(7): 1030-1033.
- Mari A, et al: Bloating and abdominal distension: clinical approach and management. Adv Ther 2019; 36(5): 1075-1084.
- Matricon J, et al: Associations Between Immune Activation, Intestinal Permeability and the Irritable Bowel Syndrome. Aliment Pharmacol Ther 2012; 36(11-12): 1009-1031.
- Malagelada J, et al: Bloating and abdominal distension: old misconceptions and current knowledge. Am J Gastroenterol. 2017; 112(8): 1221-31.
- Hellström PM: Pathophysiology of the Irritable Bowel Syndrome – Reflections of Today. Best Pract Res Clin Gastroenterol 2019; 40-41:101620.
- Serra J, et al: Modulation of gut perception in humans by spatial summation pheno-mena. J Physiol 1998; 506(2): 579-587.
- Halmos EP, et al: A Diet Low in FODMAPs Reduces Symptoms of Irritable Bowel Syndrome. Gastroente-rology 2014; 146(1): 67-75.e5
- Cuntz U: Basic concepts of gastrointestinal psychophysiology. Behavior Therapy 2014; 24: 100-106.
- Lacy BE, et al: Management of Chronic Abdominal Distension and Bloating. Clinical Gastroenterology and Hepatology, April 01, 2020, DOI:https://doi.org/10.1016/j.cgh.2020.03.056
- Hawrelak JA, et al: Essential oils in the treatment of intestinal dysbiosis: A preliminary in vitro study. Altern Med Rev 2009; 14(4): 380-384.
- Deutsche Apothekerzeitung (DAZ): DAZ 2018 (9): 73, 01.03.2018.
- Carmenthin: www.compendium.ch
GP PRACTICE 2020; 15(7): 44