Almost half (45%) of all patients with – mainly severe – asthma are also affected by chronic rhinosinusitis with nasal polyps (CRSwNP). As many as 60% have allergic rhinitis as a concomitant disease and as many as 15% belong to the group of so-called “NERD “s who have to struggle with sensitivity to aspirin. To effectively address the co-occurrence of these conditions, an ENT specialist provided recommendations.
Looking at it the other way around from the ENT physician’s point of view, CRSwNP is also accompanied by asthma in 50%, about 75% suffer from allergic rhinitis in parallel, and one in five has aspirin sensitivity. Prof. Dr. Martin Wagenmann, head of the focus on rhinology, allergology and endoscopic skull base surgery at the Department of Otolaryngology at the University Hospital Düsseldorf (D), referred to the TCRS study for a better understanding of the correlations, in which it was found that children who do not yet have asthma, but already have allergic rhinitis, carry the highest risk of also developing asthma in the course of the following years [1]. This effect increases the older the patients become.
If both diseases are already present on the other side, they also influence each other. For example, of 749 children tested who had inner-city asthma and were heavily exposed to allergens, 93.5% developed rhinitis. Seasonal exacerbations occurred in 34.2% of these patients in addition to their perennial allergic rhinitis. Strikingly, rhinitis symptoms persisted despite treatment with intranasal glucocorticosteroids (INCS) and oral antihistamines (OAH) in this study, and those patients who had difficult-to-control asthma were also the very ones who had the more severe rhinitis symptoms. There was also a close association between the time course of rhinitis and asthma exacerbations. “This is once again a clear indication of how important it is to pay attention to both the upper and lower airways in therapy,” Prof. Wagenmann cautioned.
Few therapy options
Chronic rhinosinusitis (CRS) occurs in Europe with a prevalence of approximately 11%. The phenotype with nasal polyps accounts for a proportion of 2-4%. However, even without polyps, CRS leads to a significant reduction in quality of life, the expert pointed out. The most important main symptoms of CRS are considered to be.
- the nasal obstruction
- Smell reduction
- nasal secretion
- Facial or headache
In patients with nasal polyps, the main focus is on olfactory diminution as well as nasal obstruction, which may already be helpful in the history. Secondary symptoms in both forms of CRS may also include cough, sleep disturbance/attention, and depressed mood. “In terms of drug treatment, we are relatively limited,” Prof. Wagenmann acknowledged. The basic therapy for both forms of CRS is continuous treatment with intranasal glucocorticosteroids. In addition, nasal douches are used – often simultaneously. Systemic (usually oral) steroids are effective but want to be avoided if possible because of the side effects. Antibiotics, on the other hand, do not play a role because CRS is not a bacterial disease and therefore they are ultimately ineffective.
NNH surgery with effect on asthma?
From an ENT perspective, there is also the option of surgical intervention: With the so-called FESS (Functional Endoscopic Sinus Surgery), many patients can be expected to improve their symptoms. However, regarding an effect of NNH surgery on parallel asthma disease, study data are conflicting. In a meta-analysis of 22 studies, individual aspects could be improved (reduction of asthma attacks, improved control), but overall no too large effect was demonstrated: A reduction of ICS or SABA could only be achieved in less than one third of the operated patients each time, and the improvement of lung function was non-significant [2].
From the ENT point of view, there is also the big problem of recurrences after surgery – especially in those patients with nasal polyps. Data from a prospective study [3] with 549 subjects show: In a control group without risk factors, about one in five to one in four of the operated patients suffer polyp recurrences over the years. The situation is worse for patients who suffer from asthma at the same time; more than half of them suffer recurrences after surgery. The worst off are patients with a so-called Samter’s triad, i.e. aspirin intolerance + asthma + nasal polyps: “Here it is basically the rule that polyp recurrences occur already one year after surgery”. (Fig.1).

Biologics now also in CRSwNP
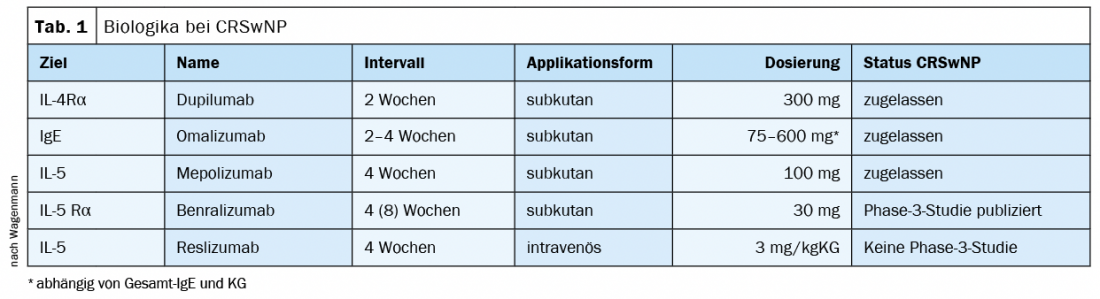
The dilemma surrounding recurrences, among other factors, has contributed to the advent of biologics for the treatment of CRSwNP in the ENT field as well. The IL-4Rα antagonist dupilumab is approved, as well as the IgE-targeting omalizumab and the IL-5-targeting mepolizumab. For benralizumab, a phase 3 study has been published in Germany; there is no study activity for the indication CRSwNP for reslizumab (Tab. 1). In the phase 3 studies vs. placebo, a reduction in polyp size was achieved with all four of the first-mentioned biologics.
What does this mean for patients who suffer from CRSwNP and asthma at the same time – Prof. Wagenmann cited a subgroup analysis from a study on mepolizumab [4] as an example: “Those affected who suffer from asthma at the same time are also those who benefit more from the biologic. In contrast, the effect of blood eosinophilia in terms of improvement at the nose is relatively small.”
Take-Home Messages
- Allergic rhinitis and chronic rhinosinusitis are the most important upper respiratory tract comorbidities.
- Diagnosis by nasal endoscopy to also distinguish the phenotypes of CRS.
- Interdisciplinary cooperation, ideally resulting in simultaneous therapy of the coexisting diseases.
- Biologics as a therapeutic option for severe forms.
Source: Streamedup! – PneumoLive: Pneumological Comorbidities, 10/13/2021.
Literature:
- Carr TF, et al: Clin Exp Allergy 2019; 49: 35-43.
- Vashishta R, et al: Int Forum Allergy Rh 2013; 3 (10): 788-794.
- Mendelsohn D, et al: Ann Otol Rhinol Laryngol 2011; 120: 162-166.
- Han, et al: Lancet Respir Med 2021; ahead of print.
InFo PNEUMOLOGY & ALLERGOLOGY 2022; 4(1): 28-29.











