Norovirus is a “pest” that strikes again every year, especially in the winter months – but it is far from being the only pathogen causing infectious diarrhea. Antibiotic-associated illness caused by the hospital germ Clostridium difficile is particularly tricky. This is where stool transplants may prove valuable.
Diarrhea is defined as frequent, i.e., more than three times daily, liquid bowel movements of more than 200 g per day. This definition is, of course, to be understood from a scientific, rather than an everyday, perspective. The patient himself sometimes already speaks of “diarrhea” when the stool is liquid (without specifically considering the frequency or quantity).
If the diarrhea lasts less than two weeks, it is by definition acute; if it lasts more than four weeks, it is a chronic form. There is a certain transitional or gray area in between. Further, two broad groups can be basically distinguished: infectious and antibiotic-associated diarrhea. Chronic forms are usually not infectious, but acute forms usually are. With three simple questions, a tentative diagnosis can already be made in practice:
- Are you currently taking or have you taken any new medications, especially antibiotics, in the past month or so?
- Have you recently returned from a trip to tropical areas?
- Do people around you suffer from diarrhea?
Infectious diarrhea
Acute diarrhea does not require culture or specific diagnosis. Fluid replacement is the top priority. “One should not underestimate the importance of fluid deficiency for general health,” the speaker said. For the night, antidiarrheal agents are an option. Otherwise, medicinal steps are not indicated; antibiotics are not normally used. Exceptions are severe courses with high fever, bloody diarrhea, poor general condition, and immunosuppression. In these cases, ciprofloxacin 2× 750 mg/d or azithromycin 500 mg/d for seven days may be considered for the two most common infectious forms of diarrhea, Campylobacter and Salmonella gastroenteritis, for example.
Known pathogens that are transmitted from person to person are the noro or rotavirus. Clostridium difficile is also one of them – one of the most common causes of nosocomial infections. Sources of enteritic Salmonella, on the other hand, are not humans but primarily animals such as chickens and the food products derived from them. The same applies to Campylobacter, which also comes mainly from the animal pathogen reservoir.
A particularly contagious, unpleasant and annually recurring form of diarrhea, especially in winter, is norovirus gastroenteritis. “You don’t want it” is the motto according to the speaker. However, this is not so easy with cases in the immediate vicinity. As few as 10 (!) to 100 viruses, which are transmitted primarily via stool and vomit (droplets) from infected persons, are sufficient to cause the disease to break out after an incubation period of no more than two days (in the truest sense of the word). Other sources of infection are contaminated food, surfaces and water. Unfortunately, hand disinfection with ethanol has only a limited preventive effect; nevertheless, in addition to a mask, gloves and an overapron, it is indispensable for close physical contact when caring for norovirus sufferers. In any case, you should do it for a long enough time, i.e. at least 30 seconds. Surfaces are to be disinfected with Kohrsolin® (aldehyde). The affected person himself feels “piss-poor” from one moment to the next due to the severe nausea. Furthermore, he is often plagued by (mild) fever, headache and aching limbs. “The only positive thing about it is that the whole thing only takes one to two days,” Prof. Krause said.
Clostridium difficile can be much more persistent. The gram-positive, spore-forming, obligate anaerobic rod-shaped bacterium is most common in hospitals. The trigger of Clostridium difficile-associated diarrhea is usually antibiotic administration. Therapy (so far) is again with antibiotics. However, recurrences are common and pose a problem. Metronidazole at a dosage of 3× 500 mg for ten days is the first choice and is used again in exactly the same way even if it occurs twice. Switch to oral vancomycin only if recurrence occurs, in
- Week 1: 4× 125 mg/d
- Week 2: 2× 125 mg/d
- Week 3: 1× 125 mg/d
- Week 4: 1× 125 mg/2 days
- Weeks 5 and 6: 1× 125 mg/3 days.
In the future, the importance of stool transplantation will probably increase here. It has been approved by U.S. health authorities for the treatment of Clostridium difficile infections since 2011. Although the exact processes in the intestine after transplantation are still unclear, it has been shown that the composition of the intestinal flora changes in the long term. The stool is transplanted via various routes, e.g. freeze-dried stool is now available in capsules.
Probiotics also useful
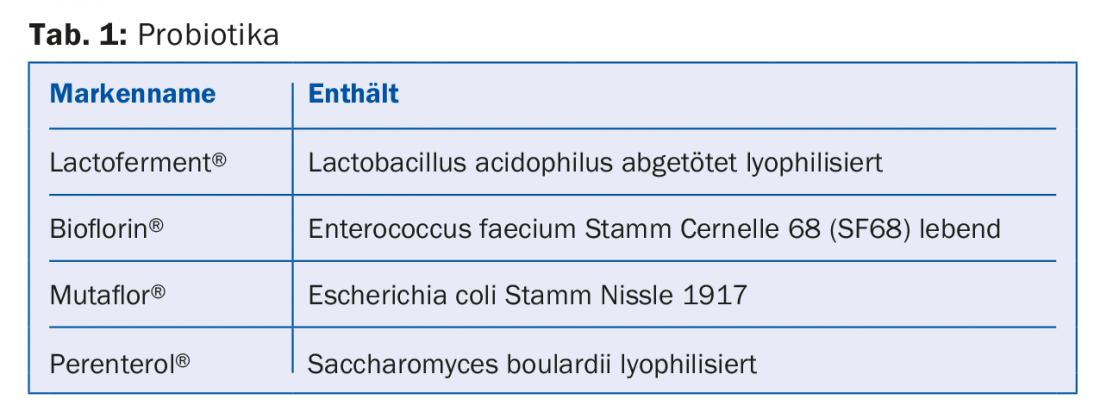
The latter effect, i.e. a change in the intestinal flora with a better long-term microbial intestinal balance, is also achieved with probiotics. In general terms, these are apathogenic but living germs that exert specific positive effects in the gastrointestinal tract. Among others, Lactobacillus sp., Bifidobacteria, Enterococci, E. coli Nissle 1917, Saccharomyces boulardii and combinations are used as probiotics. Some products already on the market shows Table 1.
“Although mainly studies with small patient numbers and a large product variation (bacterial species, dose) exist and probiotics are not noted as standard therapy in the guidelines, we still use them with success mainly in antibiotic-associated diarrhea, but partly also in acute infectious diarrhea and irritable bowel syndrome. 82 randomized-controlled trials on the use of Bifidobacteria, Lactobacillus and Saccharomyces for 5-28 days in different antibiotic therapies have shown an NNT of 13, i.e. you had to treat 13 people to prevent diarrhea,” Prof. Krause concluded.
Source: General Internal Medicine Update Refresher, June 6-9, 2018, Zurich.
HAUSARZT PRAXIS 2018; 13(7) – published 8.6.18 (ahead of print).











