A sufficient vitamin D supply is essential for healthy bone metabolism. However, studies show that in Switzerland around 50% of the population is undersupplied with vitamin D. Therefore, vitamin D supplementation is recommended especially for young children, the elderly, and pregnant and lactating women.
Vitamin D is a fat-soluble substance that is ingested either with foods of plant origin (vitamin D2) or animal origin (vitamin D3, cholecalciferol), but is mainly produced in human skin. Because of this hormonal nature of cholecalciferol, it cannot in principle be classified as a vitamin.
Vitamin D is indispensable for mineral metabolism: it ensures that calcium and phosphate are absorbed from the intestine, and it is important for the incorporation of calcium and phosphate into bone and tooth substance. In addition, the organism also needs vitamin D for the normal functioning of the muscles and the entire musculoskeletal system. In addition, vitamin D is also involved in the differentiation of cells and in the maintenance of the immune system.
Little sun – little vitamin D
90% of the biologically active vitamin D in the body is formed from cholesterol precursors in the skin. The prerequisite for this is sufficient exposure to sunlight (UVB). Since this is not always and not everywhere the same, in Switzerland there are the following risk factors for insufficient formation of vitamin D in the skin:
- Wintertime: In winter, the sun does not shine long and strong enough for enough vitamin D to be formed. Besides, in winter the skin is usually covered with clothes.
- Skin type: The darker the skin type, the worse the vitamin D formation in the skin.
- Duration of sun exposure: people who spend a lot of time outdoors have more frequent opportunities for vitamin D formation than people who are mostly indoors (e.g., residents of nursing homes, hospital patients).
- Age: In older people, the skin’s ability to produce vitamin D decreases.
- Sunscreen: The use of sunscreen prevents the formation of vitamin D in the skin.
At least 50 nmol/l hydroxy vitamin D in the blood
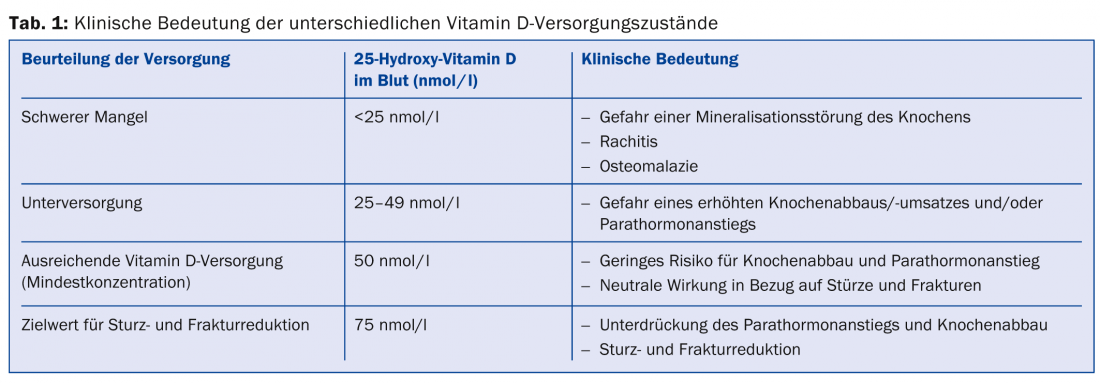
To investigate vitamin D supply, 25-hydroxy vitamin D (25[OH]D) is determined in the blood. Values ≥50 nmol/l 25(OH)D are considered sufficient according to the 2012 expert report of the Swiss Federal Commission on Nutrition. At values below 50 nmol/l, a distinction is made between undersupply and severe deficiency (Tab. 1) .
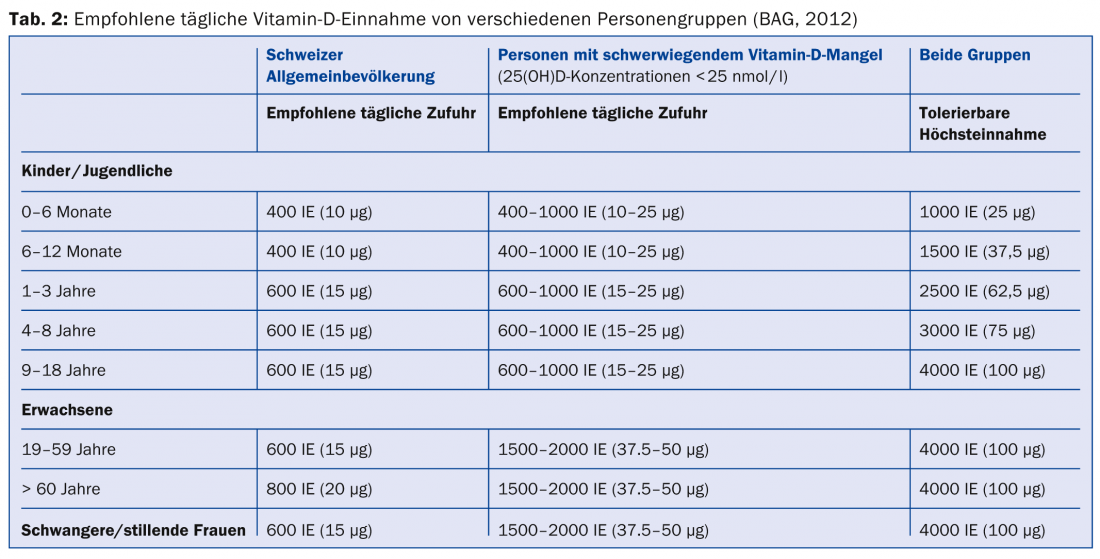
According to the FOPH, 80% of the Swiss population is sufficiently supplied with vitamin D during the summer season. However, in winter, more than 60% of the population is undersupplied or shows serum levels (concentration of 25[OH]D) below the recommended level of 50 nmol/l. Some populations are more at risk than others for vitamin D deficiency; these include infants and young children, pregnant women, and the elderly. Determination of blood 25(OH)D levels is recommended for certain groups of individuals at increased risk for vitamin D insufficiency (Table 3).
Vitamin D and osteoporosis
Vitamin D insufficiency or deficiency increases the risk of osteoporosis because vitamin D is necessary for calcium to be absorbed from the intestine, and vitamin D deficiency results in increased breakdown of calcium and phosphate from bone. Studies have shown that a sufficiently high concentration of vitamin D reduces the risk of falls and bone fractures in people over 60. For risk reduction, concentrations of ≥75 nmol/l must be present in the blood. To achieve such a concentration, supplementation requires dosages of at least 800 IU/d. According to recent studies, the benefit in individuals with high vitamin D supplementation (800 IU/d) is greater when less than 1000 mg/d of calcium per day is taken as a supplement. Vitamin D supplementation appears to have a calcium-sparing effect.
Recommendations for vitamin D supply
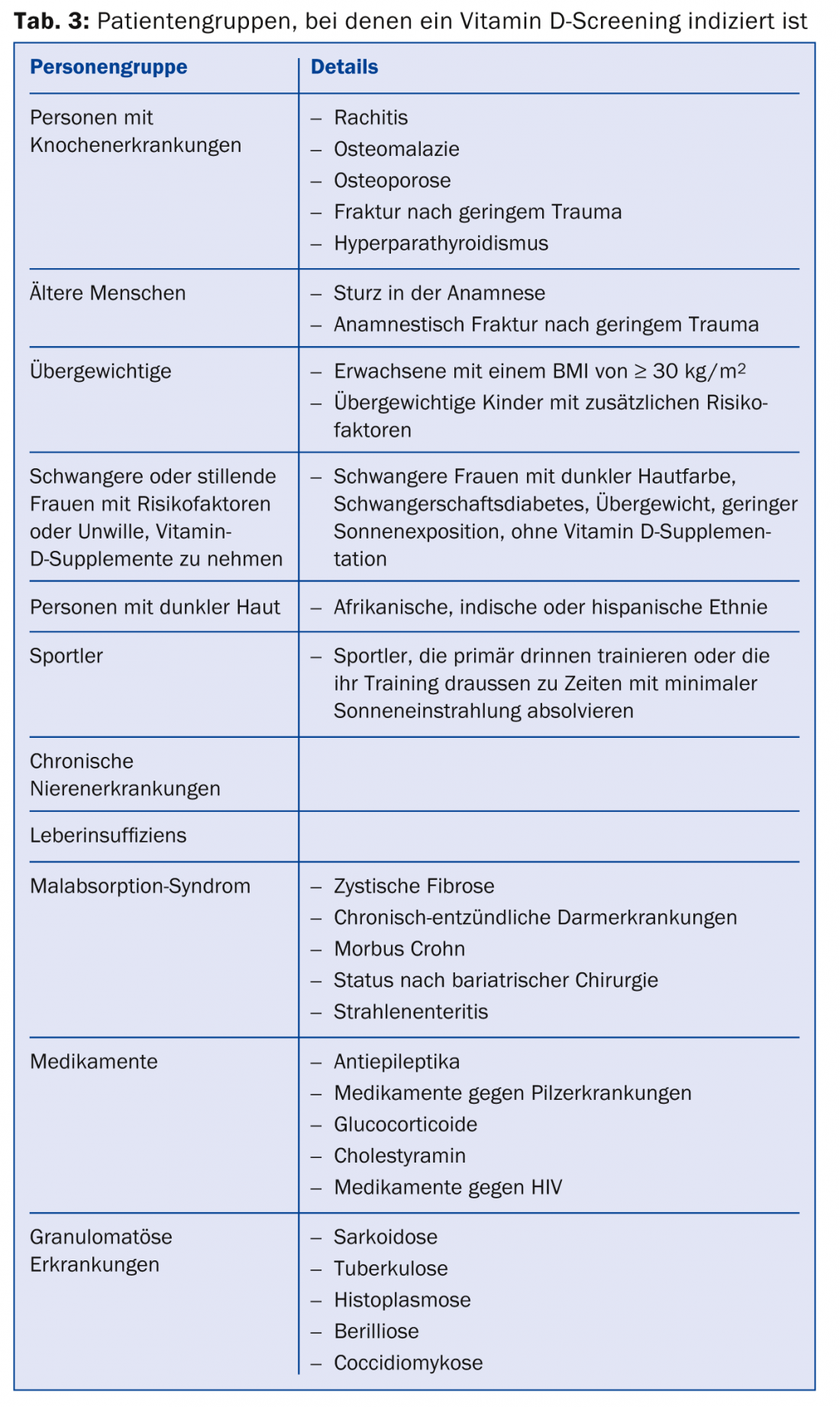
In 2012, the FOPH updated the recommendations for vitamin D supply (Tab. 2) .
The doses given aim to have at least 97% of the population reach a vitamin D concentration of >50 nmol/l. Vitamin D should be supplemented in children under three years of age, the elderly, and pregnant and lactating women, since sufficient vitamin D supply can hardly be achieved in these groups of people through diet and sun exposure.
Literature:
- Federal Commission for Nutrition. Vitamin D deficiency: Evidence, safety, and recommendations for the Swiss Population. Expert report of the FCN. Zurich: Federal Office for Public Health, 2012. www.blv.admin.ch/themen/04679/05065/05104/index.html?lang=de
- Vitamin D Recommendations of the Federal Food Safety and Veterinary Office, June 2012. www.blv.admin.ch/themen/04679/05065/05104/index.html?lang=de
- Vitamin D – the most important facts. Federal Office of Public Health, 2012. www.blv.admin.ch/themen/04679/05065/05104/index.html?lang=de
- Bischoff-Ferrari H, Stähelin H: Vitamin D and calcium supplementation. New guidelines and public health aspects. Switzerland Med Forum 2011; 11(50): 930-936.
- Bischoff-Ferrari H: Calcium and vitamin D for osteoporosis prevention. the informed physician 2013 (03): 20-25.
HAUSARZT PRAXIS 2014; 9(9): 34-36











