Various procedures are available today for the treatment of varicose veins. The technique chosen depends on the anatomical conditions and patient characteristics. Endovenous techniques involve thermal, mechanical, and/or chemical destruction of the veins; these procedures can usually be used on an outpatient basis. Surgical varicose vein therapy is now considered by many professional societies to be the method of second choice because of the higher rate of side effects.
Varicose veins are very common in the general population with a prevalence of 5-30%. The selection of the right varicose vein therapy is multifaceted and requires a thorough understanding of the patient’s symptoms and needs as well as of the anatomical and clinical situation. pathophysiologically underlying source of venous disease. Due to the often chronic and slowly progressive course, many patients do not relate their complaints to any existing venous disease, and they are therefore often all the more surprised by the substantial gain in quality of life after vein treatment.
Symptoms of varicose vein disease include pain and tightness, leg heaviness, itching, burning, nighttime calf cramps, edema, skin changes, and paresthesias. These symptoms may be increased during the course of the female cycle, during pregnancy, and under exogenous hormonal therapy. In contrast to the symptoms of peripheral arterial disease, the symptoms associated with varicose vein disease typically decrease with ambulation or elevation of the legs.
Successful varicose vein therapy usually involves elimination of superficial venous reflux with consideration of the perforating veins and deep venous system. A detailed and accurate duplex ultrasound examination with appropriate documentation is mandatory for correct diagnosis and treatment planning. Endovenous therapy is usually used to treat the truncal veins, namely the great saphenous vein, the parval saphenous vein and the anterior/posterior saphenous vein, but in special cases it is also used, for example, for perforating veins. (Fig. 1). Except in isolated cases, endovenous therapy is also possible in patients who are candidates for truncal vein stripping. Endovenous techniques involve either thermal, mechanical, and/or chemical vein destruction and can usually be performed on an outpatient basis without difficulty; they can also be combined with miniphlebectomy and/or sclerotherapy of side branches or veins. reticular varices is possible.

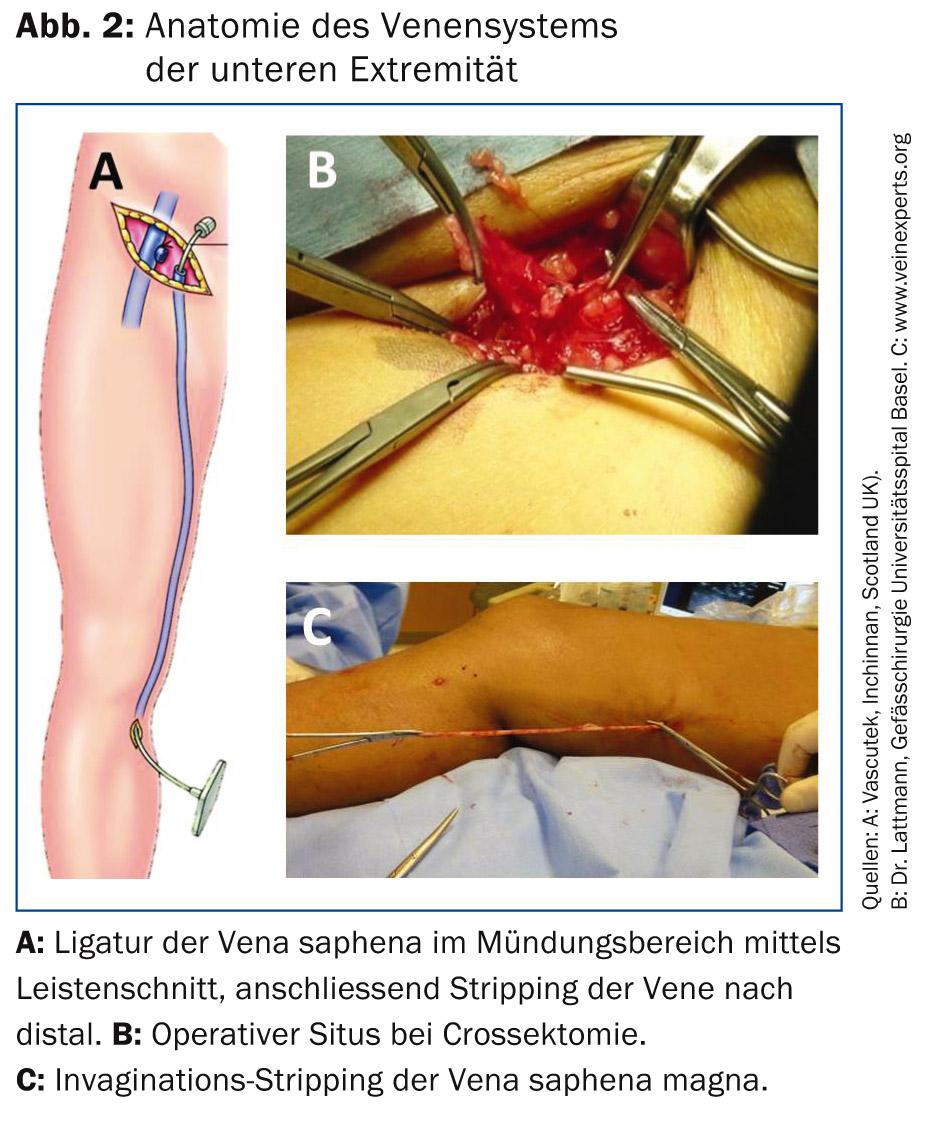
Surgical therapy (crossectomy/stripping)
The traditional treatment of varicose veins consists of a surgical interruption of the truncal veins in the area where they join the deep vein system by means of a groin incision (crossectomy) and mechanical “tearing out” (stripping) of the vein, usually under general or spinal anesthesia.(Fig. 2). Many studies have proven beyond doubt the effectiveness of surgical therapy in the treatment of varicose veins. Compared to modern endovenous procedures, stripping is more invasive and associated with higher morbidity (hematomas, nerve lesions, infections). Therefore, surgical varicose vein therapy is now considered the 2nd choice method by many professional societies [1,2].
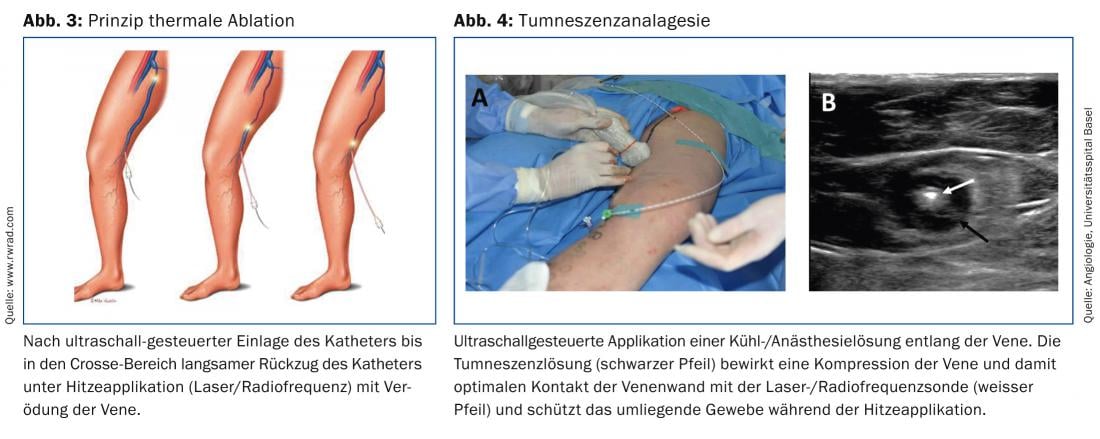
Thermal endovenous vein ablation (laser or radiofrequency)
The principle of endovenous laser and radiofrequency vein ablation is based on local thermal destruction of the vein wall with consecutive shrinkage and fibrosis of the treated vein (Fig. 3). In contrast to traditional varicose vein surgery (crossectomy/vein stripping), these modern procedures no longer require an incision in the groin or popliteal fossa under anesthesia. After ultrasound-guided puncture of the vein, a microcatheter is inserted into the vein through an access of size 1.7 mm (15G gray Venflon) to 3 mm (7 French lock). After application of a local cooling and anesthetic solution (tumescence) along the vein (Fig. 4) , the catheter is then withdrawn in a controlled manner and the vein is thermally obliterated in the course.
Several randomized trials have demonstrated at least equal efficacy of thermal catheter ablation compared with conventional surgery with concomitant reduced side effects and faster return to normal daily activities [3–5]. With all methods, an occlusion rate (persistent complete occlusion of the treated vein) in the range of >90-95% can be assumed. The development of newer catheters and increasing experience have made it possible to treat relevant perforating veins and to effectively close very large veins up to 30 mm in diameter with this procedure [6,7].
Chemical ablation (sclerotherapy)
Chemical ablation can be performed in many forms. In general, this is understood to mean ultrasound-guided foam sclerotherapy using a sclerosant – in Switzerland mainly aethoxysclerol in various concentrations. For the treatment of the truncal veins, an aethoxysclerol-air mixture is injected into the vein either via syringe or catheter under ultrasound control. In addition to vasospasm, the sclerosant causes vein endothelial damage, leading to thrombosis and ultimately fibrosis of the treated vein segment. A relatively common side effect of sclerotherapy is thrombophlebitis and consecutive hyperpigmentation along the treated vein due to hemosiderin deposition. Local thrombus expression 1-3 weeks after treatment can significantly reduce the inflammatory response and hyperpigmentation, which is usually temporary. Advantages of sclerotherapy compared to the other procedures, in addition to the lower cost, are the relative ease and speed of application. Because of its comparatively lower effectiveness (~80% occlusion rate), at least at our center, sclerotherapy is not used as the method of first choice for the treatment of truncal veins, but for the time being for the treatment of side branches and/or recurrent varicosis.
Mechano-chemical ablation (MOCA-Clarivein)
The MOCA catheter system is a further development of the sclerotherapy method and is based on a dual principle of action. After ultrasound-guided placement, a rotating catheter tip causes mechanical damage to the endothelium, while sclerosant injected simultaneously during retraction also causes chemical obliteration. The effectiveness could thus be increased compared to sclerotherapy: Compared to thermal methods, a comparably high (>90%) closure rate is achieved in the treatment of truncal veins [8]. Since this method does not involve the application of heat, no local cooling or cooling is required. anesthesia along the vein is no longer necessary and the risk of skin or nerve damage is practically negligible. This also allows the treatment of very distal sections of the great saphenous vein/parva on the lower leg without increased risk of nerve injury. For patients with asthma, patent (symptomatic) foramen ovale, or migraine, this method is not recommended because of the relatively large amount of sclerosant applied.
Cyanoacrylate tissue adhesive (VenaSeal)
The most modern and least invasive method of treating truncal veins is obliteration using cyanoacrylate, a special “superglue”. A special Teflon catheter is inserted into the vein under ultrasound control, and an applicator is used to glue the vein from the inside via the catheter with a total of approx. 1 ml of the tissue glue.
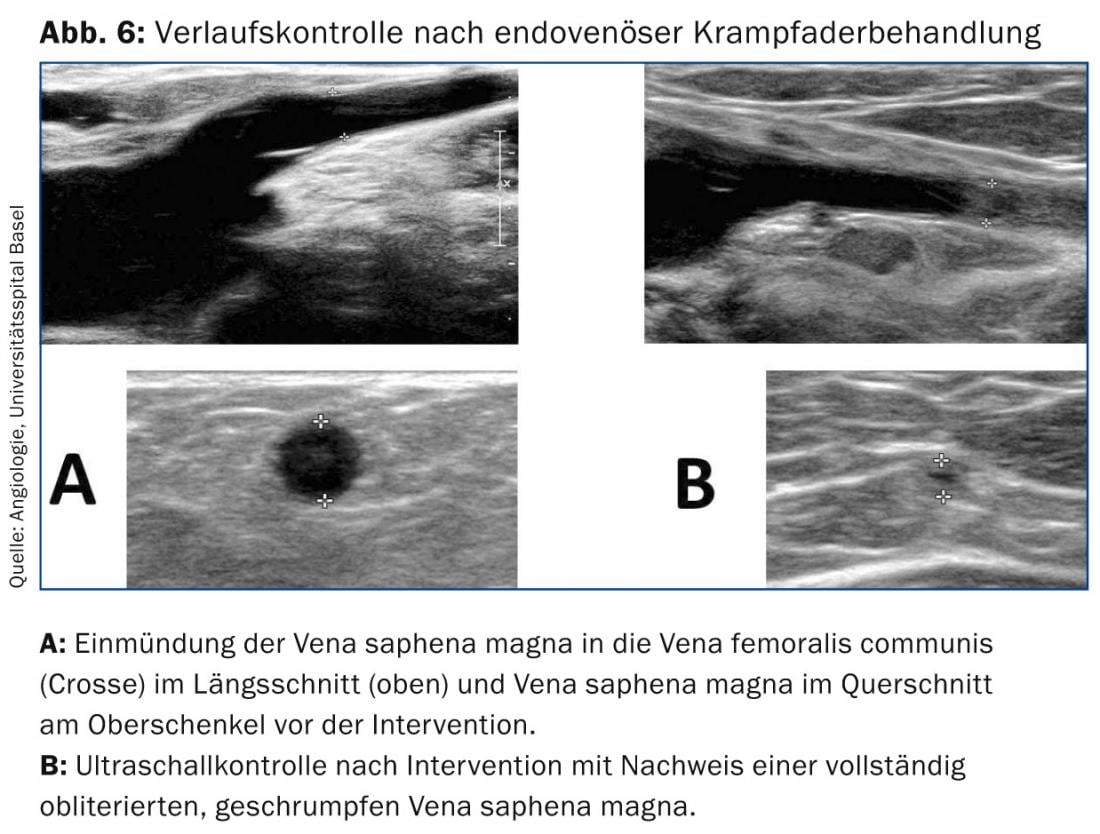
(Figs. 5 and 6).

Clear advantages of the method are that local anesthesia (tumescence) is not required and the vein can be treated in all sections, i.e. all the way distally, without risk of nerve injury. There is also no need to wear compression stockings. Patients can usually resume normal activities immediately after the procedure .
A first European study (eSCOPE) was able to show a closure rate of 92.9% after twelve months, latest data of a randomized study from the USA (VeClose) with 222 patients show an even higher closure rate of 98.9% after six months [9]. Successful minimally invasive treatment of perforating veins has also been described using this method [10]. Due to the very low side effects (temporary local inflammatory reactions) and high success rate, this form of therapy is thus an increasingly interesting therapeutic option for patients with varicose veins, despite the (still) lack of long-term data. Due to its low invasiveness, this method is the first choice in our center for patients under therapeutic anticoagulation.
Conclusion
The treatment of varicose veins has made great strides in recent years with the development of effective, minimally invasive endovenous methods. However, careful and accurate diagnosis including duplex sonography remains crucial so that the most appropriate method can be selected for each patient depending on the progress of the disease.
Conclusion for practice
- Venous leg complaints are common, but often underestimated.
- The basis of every treatment is a competent medical history, clinical examination and duplex sonography.
- Outpatient endovenous procedures, with at least the same level of effectiveness but fewer side effects, are increasingly replacing traditional
- surgery as the method of first choice in the treatment of truncal veins.
- Side branches resp. reticular veins can be treated in the same session by sclerotherapy or miniphlebectomy.
- All methods have advantages and disadvantages or limitations; individual selection based on existing symptoms and anatomical findings is elementary for optimal outcome and maximum patient satisfaction.
Literature:
- Gloviczki P, et al: J Vasc Surg 2011; 53: 2S-48S.
- Marsden G, et al: BMJ 2013; 347: f4279.
- Brittenden J, et al: N Engl J Med 2014; 371: 1218-1227.
- Nesbitt C, et al: Cochrane Database. Syst Rev 2014; 7: CD005624.
- Murad MH, et al: J Vasc Surg 2011; 53: 49S-65S.
- Zerweck C, et al: Phlebology 2014; 29: 30-36.
- Starodubtsev V, et al: Endovenous laser ablation in patients with wide diameter of the proximal segment of the great saphenous vein: Comparison of methods. Phlebology 2014 Oct 10. pii: 0268355514555546. [Epub ahead of print].
- Vun S, et al: Lower pain and faster treatment with mechanico-chemical endovenous ablation using ClariVein(R). Phlebology 2014 Oct 8. pii: 0268355514553693. [Epub ahead of print]
- Almeida JI, et al: Two-year follow-up of first human use of cyanoacrylate adhesive for treatment of saphenous vein incompetence. Phlebology 2014 Apr 30. [Epub ahead of print].
- Toonder IM, et al: Phlebology 2014; 29: 49-54.
PD Dr. med. Heiko Uthoff
Luca Spinedi, MD
Prof. Dr. med. Daniel Staub
HAUSARZT PRAXIS 2015; 10(1): 36-40