The treatment of valvular heart disease has been undergoing a major transformation for several decades. Patients who were previously rejected for heart surgery now have new opportunities. However, transcatheter interventions are still in their infancy. Of particular interest are the new developments in MK and TC.
Valvular heart disease is one of the relevant causes of morbidity and mortality worldwide. Although the aortic valve (AK) as well as the mitral valve (MK) are of great importance in cardiac surgery, the tricuspid valve (TC), also called the “forgotten valve” [1], has gained momentum in cardiac surgery [1] due to new treatment options. Conventional surgery, via median sternotomy and with the use of the heart-lung machine (HLM), is the gold standard in cardiac surgery with proven and reproducible results.
Cardiac surgery as one of the youngest surgical disciplines is in a continuous development. The first replacement of a heart valve (AK) was performed in the early 1960s by Dr. Harken [2] via a median sternotomy and with the use of HLM. Since then, the development of cardiac surgery focused on the improvement of implanted prostheses. Indeed, the improvement of surgical technique could be achieved by minimally invasive procedures, but patients still need to be connected to HLM.
In recent decades, various innovative interventional techniques have been successfully used in cardiac surgery [3]. These new therapeutic methods were initially used mainly in patients who were too high risk or in patients who were designated inoperable. With the initial experience of these new methods, several clinical studies were conducted, which showed the efficiency and safety of these methods [4-7]. As in the 1960s, interventional procedures were started with AK (transcatheter aortic valve implantation, TAVI). Now the MK as well as the TC are treated with these methods. Although these methods are safer and more comfortable for patients, the indication for these procedures is still controversial in the literature as well as in cardiac surgery practice.
In this article, we provide an overview into these new and exciting methods in the field of aortic, mitral, and tricuspid valves, as well as the indication for the methods that are mentioned.
The aortic valve
Pathologies at the AK are the most common valvular heart diseases in the Western population [8], especially aortic valve stenosis (AS), which affects a prevalence of more than 4.5% of the population older than 75 years. The gold standard treatment for symptomatic AS or aortic regurgitation (AI) is surgical repair of the valve (replacement or reconstruction). Surgical repair of the diseased valves significantly improves the symptoms, survival rate, and quality of life of patients [9]. Patient mortality varies depending on comorbidities and impaired left ventricular heart function. To assess the risk of patients, two score systems are used in daily practice: EuroSCORE (European System for Cardiac Operative Risk Evaluation) and STS (the Society of Thoracic Surgeons)-Score [10,11].
In Switzerland, the EuroSCORE is the most widely used and is critical in the selection of valve interventions. The choice of which method to use should not be based on age or refusal to undergo conventional surgery. This decision should be based on a multidisciplinary assessment of the patient by a so-called “heart team” (Class I recommendation) [12]. In principle, interventional intervention should be preferred in patients with an elevated EuroSCORE (logistic >20%) or STS score (>10%). This decision is based on several clinical studies that have shown superiority of the TAVI method in high-risk patients [5,13,14]. The use of TAVI in patients who are at lower risk (namely, intermediate or low) remains controversial. Indeed, recent clinical trials have shown that TAVI is not inferior or, in some cases, superior in patients at intermediate risk compared with surgical aortic valve replacement [15,16]. It is important to note that TAVI is already performed in intermediate-risk patients in large hospitals. However, this group of patients has a higher risk of vascular complications (e.g., inguinal vessels, dissections of the aorta) and implantation of definitive pacemakers compared with conventional surgery [15].
Another criterion for the indication of interventional aortic valve implantation is the patient’s anatomic conditions. Computed tomography must be performed before deciding between TAVI vs. conventional surgery. Here, the vascular status of the patients is assessed (Fig. 1). Of particular importance is the assessment of the coronary arteries (relevant stenoses), the ascending aorta (porcelain aorta) and the peripheral vessels (size, tortuosity and calcifications of the femoral vessels).

Furthermore, the correct preoperative selection of the size of the valve, determined by various measurements with special computer software, is important. These measurements are especially important for a good postoperative result. It is worth mentioning that most TAVI procedures are performed percutaneously through the femoral vessels under local anesthesia. Transapical TAVI is little practiced nowadays. A recently published study showed poorer patient prognosis by this method [17]. As an alternative, the subclavian artery is used when the condition or anatomy of the femoral vessels is difficult.
The mitral valve
MK pathologies, along with AK, are among the most common valvular heart diseases [8]. The pathologies of MK can be divided into two categories: Stenosis and insufficiency. MK insufficiency is the most common recognizable pathology of MK. Mitral valve regurgitation may be degenerative (myxomatous or fibroelastic degeneration) or functional (left ventricular dysfunction and dilatation).
Surgical repair of MK is nowadays the gold standard treatment for mitral regurgitation (MI), especially for degenerative MI with good long-term results [18]. In contrast, surgical repair of functional MI is controversial because the prognosis depends on the underlying heart disease. Indeed, the etiology of MI is crucial for the proper treatment and prognosis of these patients. Surgical repair can be performed minimally invasively (via right lateral mini-thoracotomy) or conventionally (via median sternotomy). The specific surgical techniques for the two causes of MI are not discussed in this article. However, it is important to note that the timing of surgery plays a large role in the prognosis of patients. Of particular importance are cardiac function, symptomatology, atrial fibrillation, age, and underlying cardiomyopathy [19].
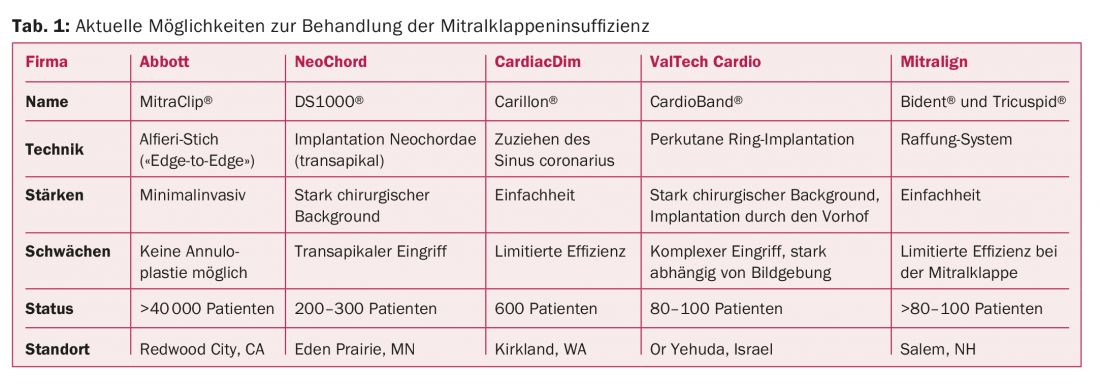
In high-risk patients (e.g., due to advanced age, severely impaired cardiac function, left ventricular dysfunction, elevated systolic pulmonary pressure), surgical repair with the use of HLM should be reconsidered because of the poor prognosis [20,21]. With the development of interventional procedures, the treatment of MK pathologies in high-risk patients became possible. One of the first methods developed is the Mitraclip (Abbott Vascular, Menlo Park, CA), which was first implanted in 2003. The Mitraclip is an interventional version of a so-called surgical “edge-to-edge” or “Alfieri’s stitch” reconstruction [21], which is performed under a short anesthetic with transesophageal echocardiography and fluoroscopy. The results of clinical trials showed very good outcomes in high-risk patients (degenerative as well as functional MI) with a success rate of over 75% [22,23]. To date, over 40,000 patients have been treated with the Mitraclip, and it is the method of choice in the interventional treatment of MI.
Since the development of the Mitraclip, other therapies have emerged. One of the most exciting newest methods for functional MI is the Cardioband system (Edwards LifeScience, Irvine, USA), a direct annuloplasty system [24,25]. This system has been implanted in over 100 patients and clinical trials are currently underway. The Cardioband system offers the option of completely catheter-based therapy with annuloplasty and leaflet reconstruction with Mitraclip. MK replacement is still in the development phase, and there is no proven method yet. However, it is an area that is currently undergoing intensive development [26] (Tab. 1).
The tricuspid valve
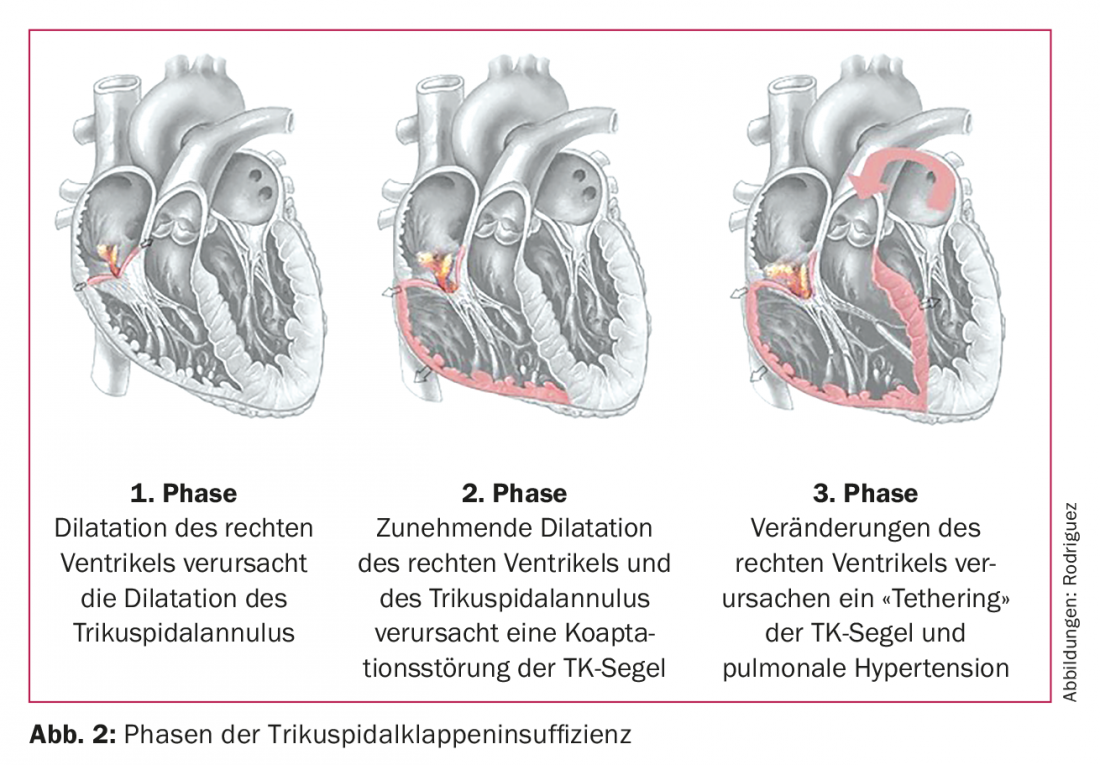
TK is often called “the forgotten valve” because of its very small share in the incidence of cardiac surgery. Only 0.5% of cardiac surgery cases are performed at TC {27]. The pathologies of TC are also divided into insufficiency and stenosis, but the stenoses of TC are rare and usually have a congenital component [28]. They are even less common than tricuspid regurgitation (TI) and are not discussed in detail. TI is further divided into degenerative as well as functional insufficiencies, although compared with AK and MK, functional insufficiencies are most common here (approximately 75% of cases) [28]. TI is very often asymptomatic, but patients in advanced stages may show low cardiac output, fatigue, and peripheral edema. A TI is recognized as clinically relevant when the annulus diameter is greater than 40 mm or greater than 21 mm/m2 [29] (Fig.2).
Primarily, TI is treated with medications (diuretics, vasodilators, therapy for atrial fibrillation, and rhythm control). Isolated surgical repair of TI is rarely performed, but is usually done in conjunction with other surgical procedures. Approximately 90% of the operations are reconstructions of the valve using various methods, which are not discussed in detail here, but the most commonly performed methods are suture annuloplasty (Kay bicuspidization, de Vega plasty) and ring annuloplasty (with flexible or rigid ring). Replacement of the TC in case of insufficiency is rarely performed.
However, some clinical studies have shown that reconstructions of the TC are a significant improvement in cardiac function as well as functional prognosis without significant risk to patients, and therefore there is now a general tendency to treat these patients earlier. As a result of this new trend, the number of surgical as well as interventional procedures is increasing. Compared to surgical interventions, some of which are stagnant in their development, the development of transcatheter interventions is growing exponentially. Interventional treatments are a good solution for the increasingly elderly population worldwide. Medical devices such as Trialign (Mitralign, MA, USA), TriCinch (4Tech Cardio, Galway, Ireland), Cardioband (Edwards LifeSciences, CA, USA), FORMA (Edwards LifeSciences, CA, USA), and Mitraclip (Abbott Vascular, CA, USA) have been successfully implanted in patients with significant improvement in patient quality of life, but long-term clinical trials are needed to evaluate these therapies. It is important to note that such therapies exist today and can be offered to patients. However, the indication for implantation of such medical devices is individualized with respect to basic pathology and patient anatomy and should be discussed in a heart team.
Concluding remarks
The treatment of valvular heart disease has been undergoing a major transformation since the last few decades. Patients who were previously rejected for heart surgery now have a chance for improved quality of life without taking a major risk. However, transcatheter interventions are still in their infancy despite more than a decade of experience. Of particular interest are the new developments in MK and TC. However, the decision of which method (interventional vs. surgical) to use in patients is not yet clearly defined. The so-called heart teams (fusion between cardiologists and cardiac surgeons) now play an extremely important role in deciding the method used for the patient. It’s no longer a competition between cardiologists and cardiac surgeons, but a joint effort for the well-being of patients. In fact, clinical trials are still needed to assess long-term outcomes as well as outcomes in other risk groups. The development of treatments for valvular heart disease remains an exciting area.
Take-Home Messages
- Although innovative interventional techniques are safer and more comfortable for patients, the indication for these procedures is still controversial.
- The gold standard treatment for symptomatic AS or AI is surgical repair of the valve.
- In Switzerland, EuroSCORE is usually decisive in the selection of valve interventions. In patients with elevated EuroSCORE, interventional procedures should usually be preferred.
- The use of TAVI in lower-risk patients remains controversial.
- Surgical repair of MK is the gold standard treatment for MI today.
- One of the newest methods for functional MI is the Cardioband system, a direct annuloplasty system.
- The decision whether to treat interventional or surgical should be made in so-called heart teams.
Literature:
- Mylotte D: The forgotten valve no more. EuroIntervention: 2017; 12(15): e1799-1801.
- Harken DE, et al: Aortic valve replacement with a caged ball valve. Am J Cardiol 1962; 9: 292-299.
- Candreva A, et al: Mitraclip and transcatheter aortic valve implantation (TAVI): state of the art 2015. Curr Heart Fail Rep 2015; 12(6): 379-388.
- Mauri L, et al: 4-year results of a randomized controlled trial of percutaneous repair versus surgery for mitral regurgitation. J Am Coll Cardiol 2013; 62(4): 317-328.
- Leon MB, et al: Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 2010 Oct 21;363(17):1597-1607.
- Feldman T, et al: Percutaneous repair or surgery for mitral regurgitation. N Engl J Med 2011; 364(15): 1395-1406.
- Smith CR, et al: Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 2011; 364(23): 2187-2198.
- Nkomo VT, et al: Burden of valvular heart diseases: a population-based study. The Lancet 2006; 368(9540): 1005-1011.
- Taramasso M, et al: Emerging approaches of transcatheter valve repair/insertion. Cardiol Res Pract 2010; 2010.
- Wendt D, et al: Society of Thoracic Surgeons score is superior to the EuroSCORE determining mortality in high risk patients undergoing isolated aortic valve replacement. Ann Thorac Surg 2009; 88(2): 468-474; discussion 474.
- Barili F, et al: Does EuroSCORE II perform better than its original versions? A multicentre validation study. Eur Heart J 2013; 34(1): 22-29.
- Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC), European Association for Cardio-Thoracic Surgery (EACTS), Vahanian A et al: Guidelines on the management of valvular heart disease (version 2012). Eur Heart J 2012; 33(19): 2451-2496.
- Reynolds MR, et al: Health-related quality of life after transcatheter or surgical aortic valve replacement in high-risk patients with severe aortic stenosis: results from the PARTNER (Placement of AoRTic TraNscathetER Valve) Trial (Cohort A). J Am Coll Cardiol 2012; 60(6): 548-558.
- Gilard M, et al: Registry of transcatheter aortic-valve implantation in high-risk patients. N Engl J Med. 2012; 366(18): 1705-1715.
- Zhou Y, et al: Transcatheter versus surgical aortic valve replacement in low to intermediate risk patients: A meta-analysis of randomized and observational studies. Int J Cardiol 2017; 228: 723-728.
- Reardon MJ, et al: Surgical or Transcatheter Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med 2017; 376(14): 1321-1331.
- McNeely C, et al: Transcatheter aortic valve replacement outcomes in nonagenarians stratified by transfemoral and transapical approach. Ann Thorac Surg 2017; 103(6): 1808-1814.
- Detaint D, et al: Surgical correction of mitral regurgitation in the elderly: outcomes and recent improvements. Circulation 2006; 114(4): 265-272.
- Taramasso M, et al: Interventional vs. surgical mitral valve therapy. Which technique for which patient? Heart 2013; 38(5): 460-466.
- De Bonis M, et al: Treatment and management of mitral regurgitation. Nat Rev Cardiol. 2011; 9(3): 133-146.
- Alfieri O, et al: An effective technique to correct anterior mitral leaflet prolapse. J Card Surg 1999 Dec; 14(6): 468-470.
- Feldman T, et al: Percutaneous mitral repair with the MitraClip system: safety and midterm durability in the initial EVEREST (Endovascular Valve Edge-to-Edge REpair Study) cohort. J Am Coll Cardiol 2009; 54(8): 686-694.
- Whitlow PL, et al: Acute and 12-month results with catheter-based mitral valve leaflet repair: the EVEREST II (Endovascular Valve Edge-to-Edge Repair) High Risk Study. J Am Coll Cardiol 2012; 59(2): 130-139.
- Taramasso M, et al: Transcatheter direct mitral annuloplasty with Cardioband: feasibility and efficacy trial in an acute preclinical model. EuroIntervention 2016; 12(11): e1428-1434.
- Kuwata S, et al: Evaluation of Valtech’s transcatheter mitral valve repair device. Expert Rev Med Devices 2017; 14(3): 189-195.
- Muller DWM, et al: Transcatheter mitral valve replacement for patients with symptomatic mitral regurgitation: A global feasibility trial. J Am Coll Cardiol 2017; 69(4): 381-391.
- Agarwal S, et al: Interventional cardiology perspective of functional tricuspid regurgitation. Circ Cardiovasc Interv 2009; 2(6): 565-573.
- Brüstle K, et al: How to treat tricuspid valve disease: what’s new on the horizon? Curr Treat Options Cardiovasc Med 2017; 19(3): 18.
- Vahanian A, et al: Guidelines on the management of valvular heart disease (version 2012): the Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur J Cardiothorac Surg 2012; 42(4): S1-44.
CARDIOVASC 2017; 16(3): 10-14