Infectious diseases are a common cause of training and competition cancellations. What could be the reason for this? Do competitive athletes even have a reduced defense?
It is interesting that this question was already researched at the end of the 19th century with the modest knowledge and possibilities at that time compared to today. Publications dating back to 1893 can be found that examined leukocyte responses to physical exertion and showed that a short ten-minute period of intense physical exertion resulted in an increase in white blood cells. These were probably the first papers on the subject of immunology and sport. Today, we are clearly further along, and the topic deserves attention, as it is not only relevant for the care of athletes, but rather for the entire population.
Immunological basics
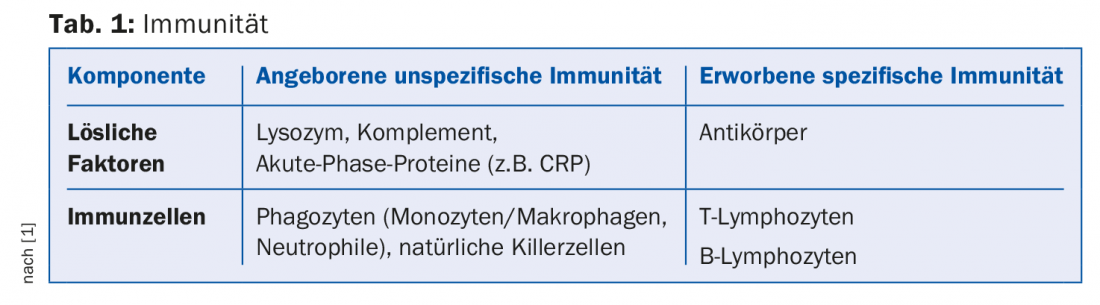
But first, it seems appropriate to recall some basics of immunology. In order to effectively hold its own against a fundamentally hostile environment full of bacteria, viruses, fungi and parasites, the human organism has various, highly differentiated and staggered protective systems. These include the skin and the mucous membranes of the organ system, which are in contact with the outside world (respiration, digestion, urogenital system), and an extremely complex natural immune system. This makes it possible to eliminate the foreign substances that have penetrated from the outside. Classically, a non-specific immune system is distinguished from a specific one, both consisting of a humoral, soluble and a cellular part. Schematically, this composition can be imagined as in table 1.
At this point, the interaction of these various defensive reactions should be noted. A constant efficiently functioning communication flow across the whole organism is indispensable for this, for which the cytokines are responsible. These released chemicals are proteins that play an essential role in the regulation of the immune response.
The “open window
Of course, the human immune system does not stand in isolation, but functions in close interaction with other bodily functions and systems. Thus, age, environment, social and psychological factors, diet, and physical activity influence resp. stress the immune defense quite significantly.
During sports activities, so-called immediate responses and delayed immune responses occur. Leukocytosis, described more than 100 years ago, is the typical immediate response. In the performing body the immune cells, in the foreground the leukocytes, are mobilized. Normally, 50% of white blood cells are free circulating and 50% are adherent to the vascular endothelium. Quite quickly after the onset of stress, these dormant cells are released by the autonomic conversion (sympathicotonia). The increase in the leukocyte count is sometimes considerable, 20′000/mm3 are not uncommon!
This spectacular increase normalizes after the load is stopped. During this time, as an expression of the delayed response, there is a decrease in natural killer cells, lymphocytes, and immunoglobulins in serum and saliva (where the change can be “easily” measured). This period is called the “open window”, a critical period when the occurrence of infections is favored.
The J-curve
However, this unfavorable timing is highly dependent on the intensity of the load. Somewhat sweepingly, it can be said that moderate training strengthens the immune system, while very intensive physical activity significantly weakens it. In a curve progression known as the J-curve in the literature, it was found that less active people have more infections than recreational athletes, but fewer than competitive athletes.
It may be taken for granted that during athletic performance countless bodily functions experience quantitatively but also qualitatively relevant changes: Cardiovascular, endocrinological and metabolic activities usually have to be raised to a higher level to meet the increased energetic demand. The defense system is thus also affected, which may explain its unfavorable decrease in performance. It is speculated that increased respiratory volume may load the airways with more germs, that general increased blood flow may alter mucosal permeability, or that metabolic changes such as acidosis or hormonal ones such as increases in cortisol may promote changes in immune cells through suppressive mechanisms.
In addition to these factors directly related to physical activity, the lifestyle of competitive athletes also plays an immunologically bionegative role: living in a collective with facilitated possibility of transmission of infectious microorganisms, working outdoors, in poor weather conditions with risk of hypothermia, or improved tendency of bacteria to multiply in heat. The psyche is also stressed – the tendency to infection increases in stressful situations with lack of sleep (jet lag).
Nutrition is also at the top of the list of causes: Malnutrition in general, frequent changes in eating habits, deficiencies in the vitamin and mineral balance.
How to prevent?
These possible reasons show the direction in which prophylaxis must go in competitive athletes: careful planning of the training program (especially the recovery time), targeted regeneration (sauna), sleep, mindful nutrition (possibly supplementation with vitamins and minerals), vaccinations and banal hygiene measures (change of clothes, drying hair, etc.). Avoidance of potentially infectious contacts (e.g., at press conferences) should also be considered.
What may seem self-evident at first glance is extremely complicated to realize in practice, and from my own experience one of the most thankless tasks of a supervising sports physician.
One last but important note in connection with sports and infections: Even though the illness is usually mild and short, training must be reprogrammed during this time. Do not exercise if you have a fever, swelling of the lymph nodes or general fatigue. Experiments have shown that infections are more severe if heavy physical labor was performed during the incubation period. In addition, one increases the risk of myocarditis and thus for acute cardiac death. A rule of thumb allows resumption of light training after twice as many days as fever days, for example, two days of fever, four more days to start.
In team sports, strict action must be taken to avoid epidemics with serious sporting consequences.
Literature:
- Weineck J: Sports Biology. 10th revised and expanded edition. Spitta Verlag 2009.
Further reading:
- Knechtle B: Physical activity, immune system and cancer. Swiss Journal of Sports Medicine and Sports Traumatology 2003; 51(3): 145-151.
- Steidl A, et al: Sports activity, immune system and susceptibility to infections. Austrian Journal of Sports Medicine 1996; 1-2: 1-24.
- Schwaninger L, Jenoure A: Effect of physical activity in breast cancer patients taking aromatase inhibitors. Diploma thesis Zurich University of Applied Sciences 2017.
HAUSARZT PRAXIS 2018; 13(1): 4-5











