If, in the case of year-round bronchial asthma, no causative agent can be identified from among the usual suspects such as budgerigars or desert jumping mice, but any aquarium dwellers are innocently doing their rounds, then a look into the food cans of these faithful co-inhabitants could solve the mystery. The author coined the term aquarium allergy for this.
Medical history
The 27-year-old patient (A.P.) developed nocturnal bronchial asthma about six months before his first presentation to the allergy ward of the University Hospital Zurich, which soon extended throughout the day, including weekends. No other symptoms, such as rhinitis or conjunctivitis, occurred. The workup at the allergy ward occurred after the primary care physician, who was treating the patient symptomatically with asthma medications, noted an elevated total serum IgE of 1000 E/ml.
Anamnestic, possible triggering factors initially included pets, a desert jumping mouse and a budgie, and occupational solvent exposure. However, the fact that the patient was not symptom-free during the weekend spoke against the latter.
Skin testing showed negative immediate reactions in the prick test to pollen and also negative results in the intradermal test to house dust mites, animal epithelia and molds. Clearly positive immediate reactions were obtained to house dust extract (today this test is obsolete), house insect mixture, ornamental bird feathers and silk, but not to wild silk (we have discussed wild silk allergy in DERMATOLOGIE PRAXIS 2017 Vol. 27, no. 2, pp. 26-30 reported).
Based on the allergological testing, the patient was advised to remove the budgie and the jumping mouse along with their cage and a thorough dust cleanup; he certainly did not own a silk blanket.
At follow-up one month later, the patient stated that he had removed the pets, but there had been no improvement. A scratch test with the company’s own dust samples turned out negative.
Further questioning revealed that the patient had owned an aquarium for some time. The fish were not considered pets and had not been reported at the initial consultation. Frozen red mosquito larvae were fed almost daily.
Supplementary allergological clarification
The subsequent prick test modified with the frozen red mosquito larvae (Fig. 1) showed a strong immediate reaction, specific IgE (Phadebas-RAST) to red mosquito larva (Chironomus thummi) (i73) were strongly positive with a total serum IgE of 859 E/ml class 3.
Diagnosis
Asthma bronchiale allergicum in sensitization to red mosquito larvae.
Comment
We had reported on sensitization to red mosquito larvae (twitch flies), Chironomus thummi, which can lead to respiratory, conjunctival and cutaneous symptoms, with Jörg Knüsel in 1983 [1]. Chironomids are non-biting mosquitoes, allergenic relationship among individual species has been demonstrated. As early as 1980, a polypeptide sequence in the hemoglobin of red mosquito larvae was found to be a potent allergen (Chi t1) [2]. In aquaristics, both live, frozen and dried, powdered red mosquito larvae are offered, and many fish foods also contain chiriniomids as a component.
Course
The patient was discharged with the recommendation to stop using fish food containing chirinomides (even in dry form).

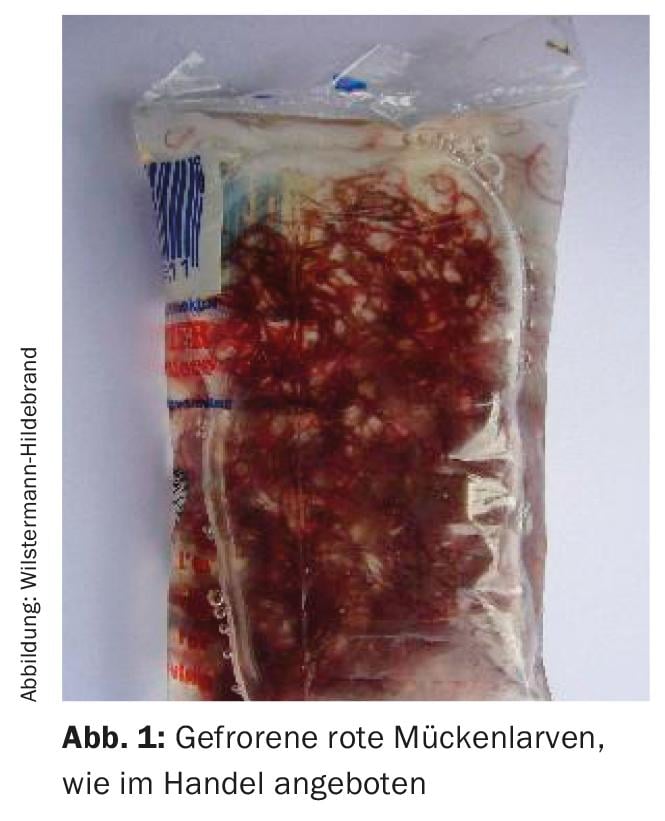
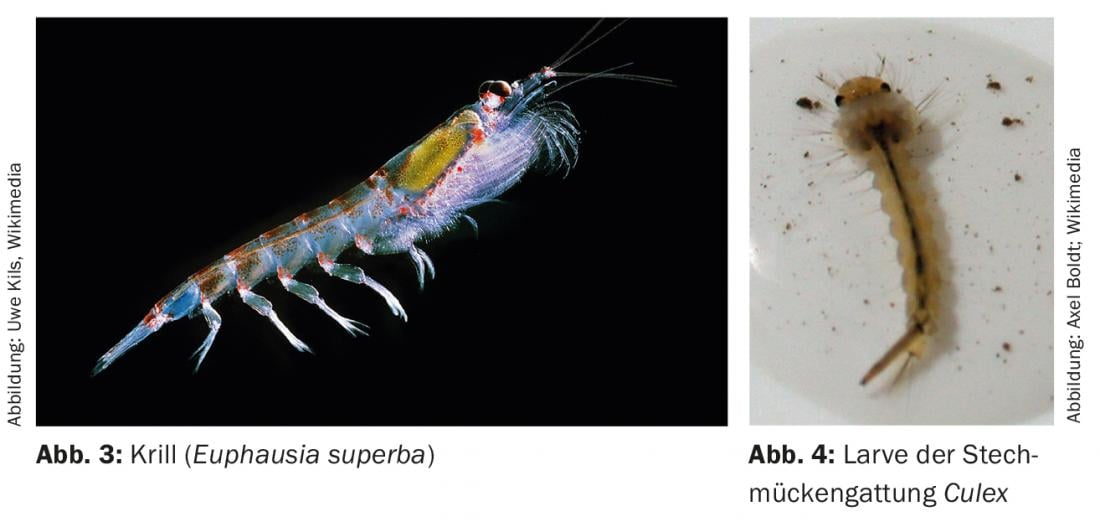
A quarter of a year later, the patient reappeared because there had been no improvement in asthmatic symptoms despite supposed allergen abstinence. Skin tests were now performed with the fish diets that continued to be used; strong immediate reactions occurred to daphnia (Fig. 2), krill (Fig. 3) , and mysis (all small crustaceans), as well as black mosquito larvae (Culex) (Fig. 4) and three different dry diets.
Intracutaneous tests with shrimp and crawfish extract were also clearly positive. RAST determination on shrimp (prawn) and crab were highly positive with class 4. The patient reported that he had last eaten shrimp three years ago, and subsequently experienced nausea and dizziness. Until now, he had assumed that it had been spoiled food. In retrospect, however, it seems to have been more of an allergic event.
The patient was now advised to eliminate the aquarium and strictly refrain from ingesting crustaceans.
Just two nights later, the patient was able to sleep through the night for the first time, and after a few weeks he was completely free of symptoms.
Final diagnosis
- Allergic bronchial asthma in “aquarium” allergy due to polyvalent sensitization to red and black mosquito larvae, daphnia, krill, and mysis.
- Status after gastrointestinal food allergy to crustaceans.
Fish food allergy
As several publications in this field show [1–3], fish feed is a significant allergen source in aquaristics. The fine powder dust of the dry powders is mostly responsible for the inhalation sensitizations. Dried food is marketed in various forms, mainly either as lyophilized species (partially ground) or pressed and mixed with other animal and vegetable additives in the form of flakes or tablets. The risk of sensitization is mainly when the flakes or tablets are crushed with the fingers and the dust is inhaled. But also living or frozen creatures, as offered in the trade, can cause allergies, e.g. also when dipping the arm into the aquarium. The main allergens are usually small organisms of lower animal species living in the water, such as mosquito larvae, small crustaceans and various worms, but also ground larger crustaceans and plants. The most important and best researched allergen is the red mosquito larva (Chironomus thummi thummi), but allergies to dried daphnia (freshwater fleas, i.e. small crustaceans) are also described in the literature, as in the casuistry shown. Are fed, in addition to mosquito larvae and water fleas (Daphnia), also krill (Euphausia superba), a small crayfish that lives in massive swarms in Antarctic waters, the gill-foot crayfish (or brine shrimp). Artemia salina – here the commercially available eggs are prepared with water and the freshly hatched larvae are fed -, copepods (Cyclops), mudworms or stream tubeworms, better known as. Tubifex, Small fruit fly (Drosophila melanogaster), large fruit fly (Drosophila hydei), aceticelia (a small worm from the nematode family), paramecia (the protozoa Paramecia), Mexican psyllid (Hyalella azteca) , brook psyllid (Gammarus pulex), enchytraea, such as Enchytraeus albidus , white microworms, and grindal worms (Enchytraeus buchholzi), i.e., a variety of possible allergen sources. That is why the term “aquarium allergy”, coined by us, has become popular.
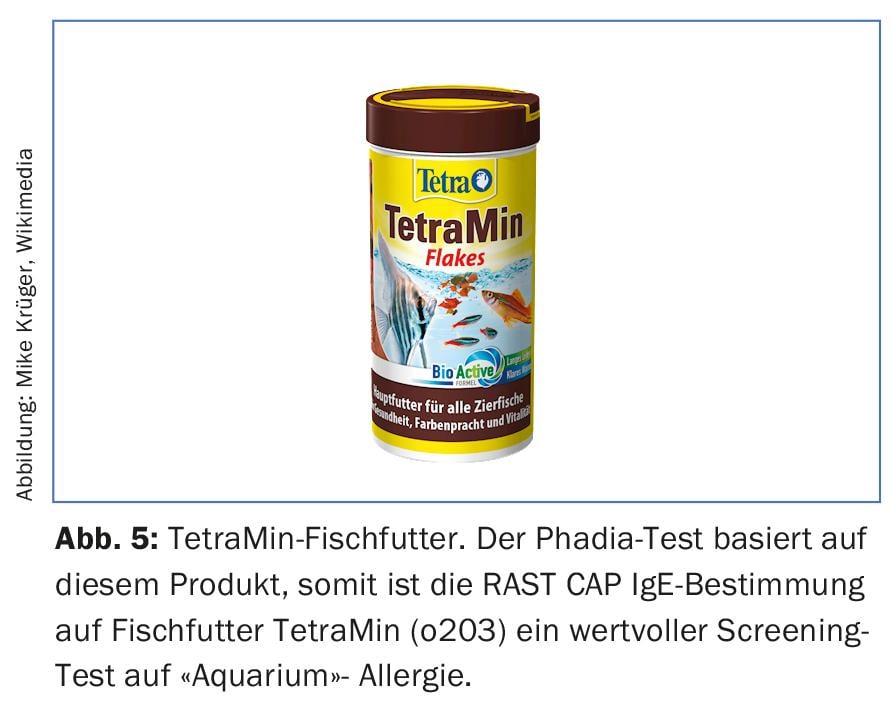
Diagnostically, it is significant to even think of an “aquarium” allergy. The allergist will perform prick or scratch tests with fish food components under increased caution (caveat: anaphylaxis when testing highly sensitized!). Commercially available IgE assays (RAST CAP, Phadia) for red mosquito larvae (Chironomus Thummi) (i73), fish food Artemisia salina (o202), fish food Daphnia (o207) and fish food TetraMin (o203), according to the manufacturer it is a carefully selected mixture of high quality and functional nutrients with vitamins, minerals and trace elements for a complete, daily nutrition. (Fig.5). Thus, IgE determination to fish food TetraMin (o203) can be a valuable screening test for “aquarium” allergy for the general practitioner.
Conclusion
The particular interest of the case described above, which was published in extenso by Regine Dietschi and myself in 1987 [3], lies in the relevant sensitization to all fish foods used, whereas mostly – with respect to fish foods – monovalent sensitization to chirinomids is followed [1]. Very beautifully by this observation also illustrates that the question about domestic animals is generally insufficient and purposefully with allergologischer clarification with “indoor” symptomatik also after aquariums together with green plants [4,5] or wild silk bed contents [6–8] should be investigated.
Reading tips on the Internet: www.alles-zur-allergologie.de for the search term “pet food
https://de.wikipedia.org/wiki/Zierfischfutter
Acknowledgments: We would like to express our sincere thanks to the former assistants of the allergy ward, Dr. Regine Dietsch and Dr. Jörg Knüsel, for their cooperation at that time in the publications on which this report is based.
Literature:
- Knüsel J, Wüthrich B: “Aquarium allergy”: fish food, also a domestic allergen. Schweiz Med Wschr 1983; 113: 658-662.
- Baur X: Hemoglobins of chirinomids (twitch flies): previously unknown aggressive inhalation antigens for humans. Clin Wschr 1980; 58: 1163-1164.
- Dietschi R, Wüthrich B: “Aquarium” allergy: bronchial asthma due to polyvalent sensitization to various fish food constituents. Dermatologist 1987; 38: 160-1.
- Wüthrich B, Anliker M, Bircher A: Indoor allergens: Ficus benjamina and other green housemates. HAUSARZT PRAXIS 2017; 12(4): 14-19.
- Wüthrich B., Bircher A., Schmid-Grendelmeier P: Nocturnal allergy symptoms without apparent cause. DERMATOLOGIE PRAXIS 2017; 27(2), 26-30.
- Wüthrich B, Dietschi R, Keter A, Zortea-Caflisch C: The so-called “wild silk” asthma – a still current inhalation allergy. Schweiz Med Wochenschr 1985; 115: 1387-1393.
- Eng P, Wüthrich B: “Wild silk” – another allergen in the bedroom Schweiz Rundschau Med (PRAXIS) 1994; 83: 402-406.
- Wüthrich B: Nocturnal asthma attacks instead of “dreamy and cozy sleep”. DERMATOLOGIE PRAXIS 2016; 26(6): 46-50.
DERMATOLOGIE PRAXIS 2017; 27(4): 39-42
DERMATOLOGIE PRAXIS 2018 Special Edition (Anniversary Issue), Prof. Brunello Wüthrich