When we talk about cardiomyopathy, we can be talking about different clinical pictures with different causes and symptoms. The actual cause may be genetic, acquired, or a mixture of both. Especially in very early or very advanced forms, the cause of the cardiomyopathy often cannot (yet) be determined. Imaging is then an important parameter to perform risk stratification of the affected individuals.
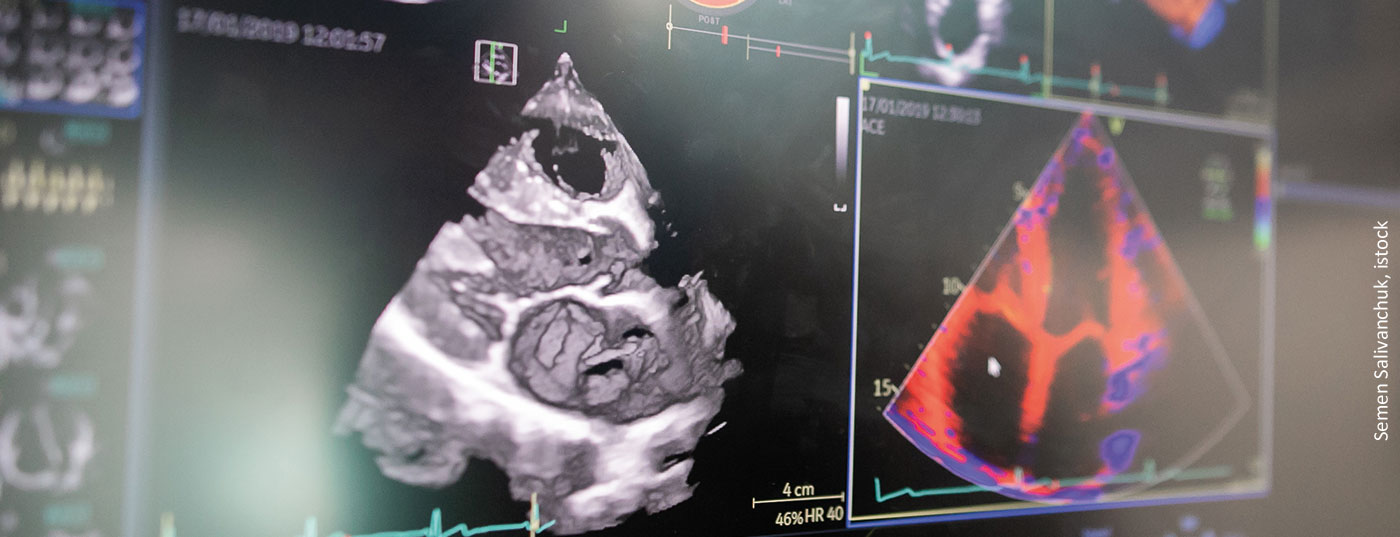
Around the question of how to stratify a patient’s risk and where to look closely, Prof. Fabian Knebel, MD, Berlin (D), explained the use of imaging as a key tool. Risk management of cardiomyopathies was addressed over one hundred years ago. At that time, the credo was still that therapy depended on the actuity of heart failure, not on its etiology. Black coffee, champagne and cognac were recommended as therapy to improve circulation. In the meantime, fortunately, we have made some progress. The current ESC position paper on cardiomyopathies recommends echocardiography as a critical imaging component after clinical findings have been obtained. This can be used to assess cardiac structure and function and to identify specific etiologies. Ultimately, dilated, restrictive, and hypertrophic cardiomyopathy should be differentiated.
Since ejection fraction (EF) alone is not sufficient, additional deformation imaging is needed. EF-based echocardiographs are guided by radial function, whereas deformation imaging can be used to capture longitudinal function. This is because patients may well have preserved pump function but reduced strain. However, these affected individuals have a much worse prognosis than patients with a normal strain, the expert said.
Targeting risk patterns
Different patterns can be detected for risk stratification. These include, for example, the hypertrophic cardiomyopathies with their genetic forms, storage diseases, neuromuscular and mitochondrial disorders, and malformations. Regarding pathomechanisms, in addition to wall thickness, we observe whether the patient has a SAM phenomenon and/or ejection tract obstruction. In addition, the gradient should be worked out. However, caution is required, especially in HCM, because different phenomena can also overlap. The strain per se forms a risk marker of HCM. If the strain is <16%, sufferers show significantly worse survival than sufferers whose strain is >16%. Mechanical dispersion can be used as a second tool for risk stratification. In addition, contrast echocardiography should be used to observe whether the septal branch into which the contrast agent was injected is the one blocking outflow.
Supportive imaging
In restrictive cardiomyopathies, the first priority is to work out by imaging whether it is a constriction with a problem primarily in the pericardium, or whether the problem is primarily in the myocardium and therefore it is a restriction. Common to both is impaired ventricular filling and diastolic heart failure. Restrictive cardiomyopathy can be divided into noninfiltrative, infiltrative disorder, storage disease, and endomyocardial disorder. These may include endomyocardial fibrosis, sarcoidosis, eosinophilic myocarditis, or Fabry disease. Specific to this patient is often that the papillary muscle is markedly thickened.
Source: risk management in cardiomyopathies. Imaging as a key tool in individual risk management. Working group meeting, 20.04.2022, 15:30-17:00
Congress: 88th Annual Meeting of the German Society of Cardiology (DGK)
CARDIOVASC 2022; 21(2): 23