Approximately 90% of all gastric cancer cases are associated with Helicobacter pylori infections. Eradication of these pathogens in healthy asymptomatic individuals or in the general population appears to reduce the incidence of gastric cancer – by 34% versus placebo or no therapy, according to a Cochrane review. However, the authors emphasize that the evidence is of mediocre quality and the number of studies is limited.
Data were examined from the Cochrane Central Register of Controlled Trials, MEDLINE, and EMBASE, as well as hand-selected relevant congress abstracts. In addition, experts were asked about the most significant clinical trials and unpublished material.
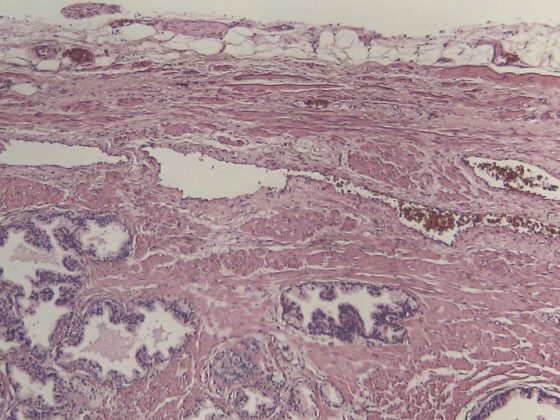
Randomized controlled trials that compared at least one week of H. pylori therapy with placebo or no therapy and tested its preventive effect were eligible for analysis. Gastric cancer was defined as any adenocarcinoma of the stomach (intestinal differentiated or diffuse undifferentiated type, with/without specified histology). Follow-up had to be for at least 2 years and ≥2 individuals had to have actual gastric cancer at the time of study completion. However, at baseline, participants were not allowed to have any symptoms or disease apart from their confirmed positivity for H. pylori.
Much of the data comes from Asia
Only just six studies with a total of 6497 participants met the strict selection/quality criteria. Five of the six analyses referred to an Asian population, which is not surprising since, for example, Japan has a comprehensive eradication program and a “test and treat” strategy in the course of gastric cancer prevention (not least because of the significantly higher prevalence of H. pylori infections compared with other countries). The authors estimated the risk of bias to be high in two studies, low in three, and unclear in one.
Quality of examinations is mediocre
The main objective of the meta-analysis was to determine the extent of the preventive effect of eradication. Using mediocre evidence from the six studies used, they conclude that the risk ratio for developing subsequent gastric cancer versus no therapy or placebo is 0.66 (95% CI 0.46-0.95). 1.6% from the eradication group became ill, while this was true for 2.4% from the untreated group. Or, to put it another way, eradication reduced the risk of disease by 34%. Whether this also reduces the risk of death from gastric cancer could not be determined from the data, because the confidence intervals varied widely. Three studies with 4475 participants had examined this parameter and found a risk reduction of 33%, but the associated values of the 95% confidence interval ranged from 0.4-1.11. A relevant effect on all-cause mortality could not be demonstrated in any of the four studies investigating this factor.
Side effects of eradication were described to an insufficient extent, which is why the authors refrain from making a conclusive statement.
Effect on esophageal tumors
Only one study examined the effect of eradication on esophageal tumor development. Two of 817 participants in the eradication group and one in the placebo group (n=813) developed such neoplasia (RR 1.99; 95% CI 0.18-21.91). Consequently, the presence of H. pylori could possibly even reduce the risk in this case, but the results do not allow a clear conclusion and thus do not help to clarify the controversial data in this area.
Limitations
Overall, the authors note that it is unclear whether the results of their meta-analysis can be applied to other, non-Asian populations. Also critical is the weight given to large studies in such a small sample of six studies. Finally, the delicate resistance situation and multidrug-resistant germs that threaten every antibiotic therapy must be mentioned – after all, by far not all cases of antibiotic eradication are successful. One way of limiting the use of antibiotics is to define risk groups that are eligible for eradication. This remains a major challenge, however, as numerous individual risk factors must be taken into account in addition to H. pylori infection.
Source: Ford AC, et al: Helicobacter pylori eradication for the prevention of gastric neoplasia. Cochrane Database of Systematic Reviews 2015; 7: CD005583. DOI: 10.1002/14651858.CD005583.pub2.
InFo ONCOLOGY & HEMATOLOGY 2015; 3(11-12): 4.