Peeling indications are incipient photoaging resp. superficial melasma (superficial peel); more prominent wrinkles, lentigines solares, actinic keratoses, deeper melasma, incipient elastosis cutis, superficial scars (medium-depth peel); extensive areas of actinic keratoses, severe actinic elastosis cutis with deep wrinkles, deep bowl-shaped acne scars (deep peel). Correct patient selection and careful care before, during and after treatment are the basis for an all-round satisfactory treatment. Complications are largely avoidable if relatively simple rules are followed and patients are fully cared for in the pre- and especially in the post-operative period.
In the second part of the series, the most important peeling indications are discussed first. After that, it’s all about patient selection and care, and avoiding complications.
Superficial peels (Fig. 1): In general, the deeper the peel, the more effective the expected result. Superficial peels address superficial structures such as incipient photoaging (superficial hyperpigmentation or fine wrinkles) or superficial melasma. A good indication for superficial peeling is refreshing the face. The effect is achieved only after multiple treatments and repeat cycles once or twice a year are recommended. When used correctly, these peels are highly valued, as the appearance of the skin improves significantly after the first treatment cycle, and after multiple treatments there is a measurable tightening of the facial skin. The downtime of superficial peels is usually negligible. Reactions such as irritative redness and minor peeling usually last no longer than 24 hours and are very easy to treat cosmetically (camouflage).

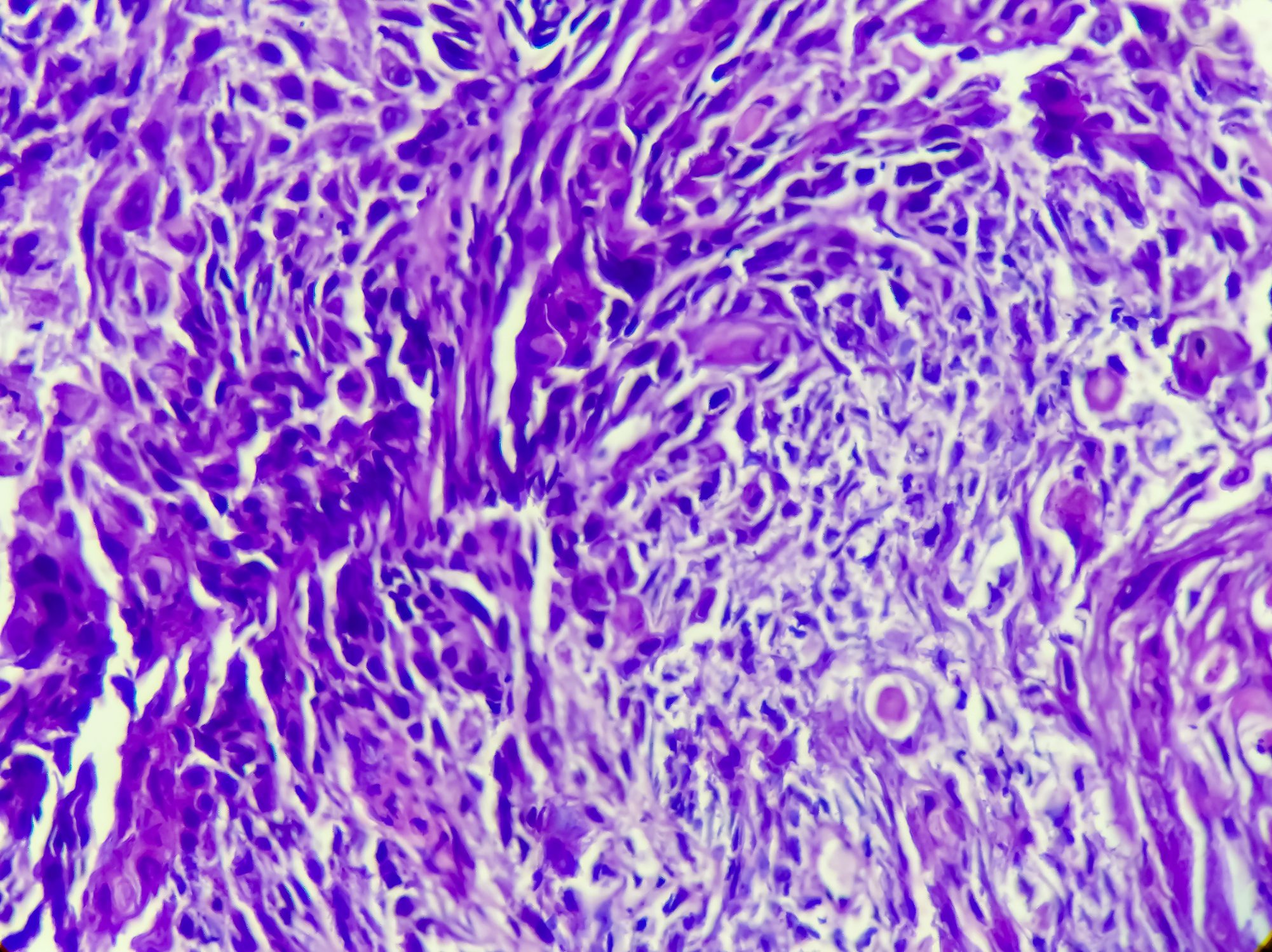
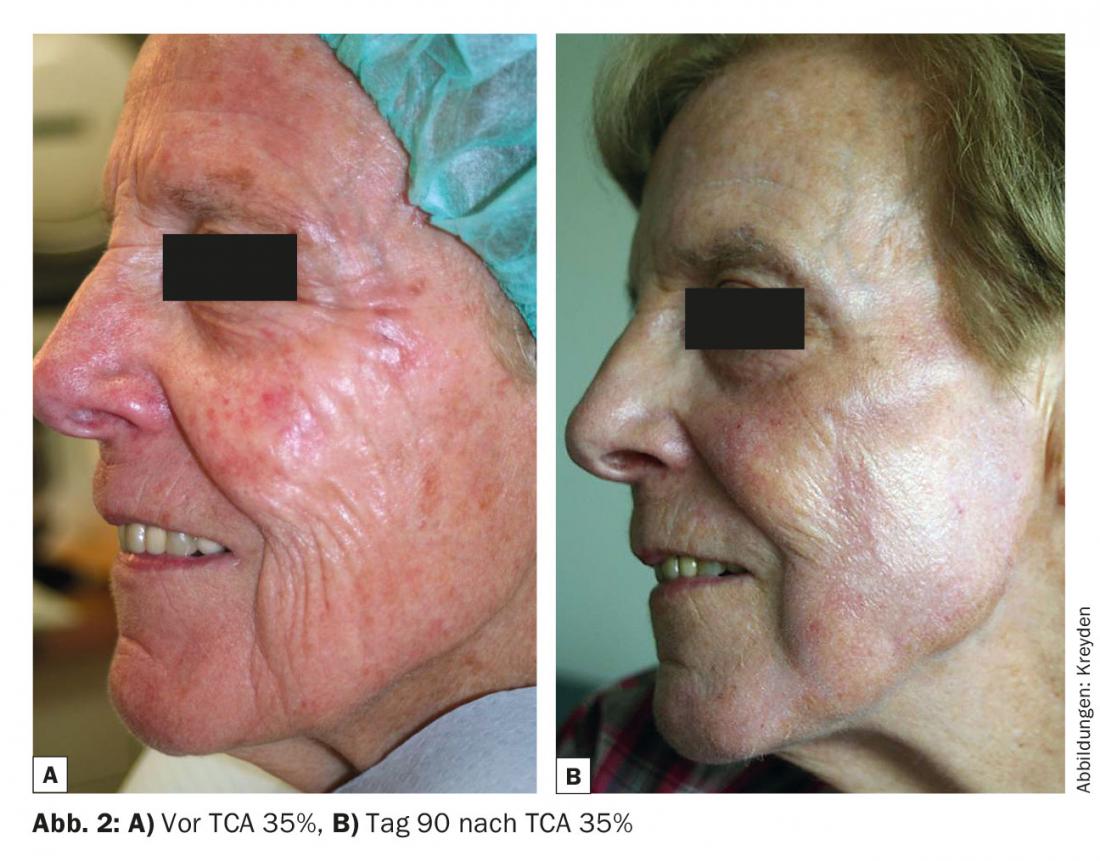
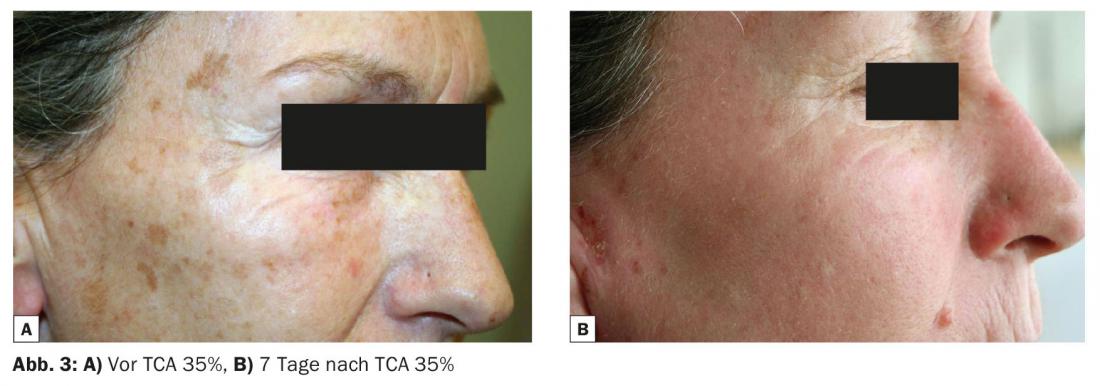
Medium-depth peels (Figs. 2 and 3): If the wrinkles are already more prominent, show clear actinic signs such as lentigines solares or also actinic keratoses, medium-depth peels are indicated. TCA 35% can also be used very successfully for deeper melasma or to improve incipient elastosis cutis. Superficial scars can also be positively influenced by TCA 35%. With medium-deep peeling, a certain degree of lifting effect can already be achieved. The downtime of medium depth peels is approximately five to seven days. Reactions begin with a leathery discoloration of the skin associated with increasing erythema and moderate swelling (days 1-3), followed in some cases by extensive peeling, which lasts about three to five days.
Deep peels (Fig. 4): Phenol peeling is the “supreme discipline” of peelings. When used correctly, the results are sometimes impressive. Indications range from severe actinic elastosis cutis with deep wrinkles to extensive areas of actinic keratosis (e.g. scalp of men) to deep bowl-shaped acne scars. Of course, the above-mentioned superficial changes are also effectively and permanently addressed. A disadvantage of phenol peelings is the relatively complicated procedure, as a corresponding therapy requires co-supervision of an experienced anesthesiologist. Phenol peels are painful and require sedo-analgesia (usually fentanyl in combination with propofol), which in turn entails further monitoring of patients several hours post interventionem. In addition, the considerable postoperative inflammatory reaction associated with sometimes severe swelling and peeling effects that begin after a few days are among the negative aspects of phenol peeling. The downtime for phenol can be specified as seven to ten days. Due to the deep effect of the phenol, in the vast majority of cases there is a prolonged erythema formation (up to twelve weeks) and subsequently a permanent, albeit moderate, reduction in pigmentation of the treated area. However, with good information and correct treatment with harmonious and regular results, these disadvantages are readily accepted when the result is compared.

Patient selection
As in other aesthetic dermatological subfields, correct patient selection is an extremely important building block for a universally satisfactory treatment in peeling, especially in medium-depth and deep peeling. There are “soft” inputs and outputs. Exclusion criteria such as patient-specific characteristics. Patients at risk are those with unrealistic expectations or non-objectifiable findings. Patients who are difficult to manage psychologically or who are undecided after multiple orientations also fall into this category [1]. The “hard” inputs and outputs include Exclusion criteria include the correct medical indication and the assessment of the efficacy or safety of the treatment. side effect profile. At times, it may well be difficult to assess whether the patient requires a medium-depth peel with TCA 35% or a deep peel with phenol.
Since all peels, including superficial peels, are associated with a certain downtime, prior accurate patient information is extremely important. This applies in particular to the planning of medium-depth TCA and deep phenol peels. A good indication for a medium-depth or deep peel is given when the treating physician is sure that the indication is correct and that the treatment will be successful, and when the patient to be treated is looking forward to the therapy and above all to the result.
Patient Care
The sometimes severe post-peel reactions require extremely careful and also careful as well as professional care of the patients throughout the peeling process. Care begins long in advance and ends weeks after the actual treatment.
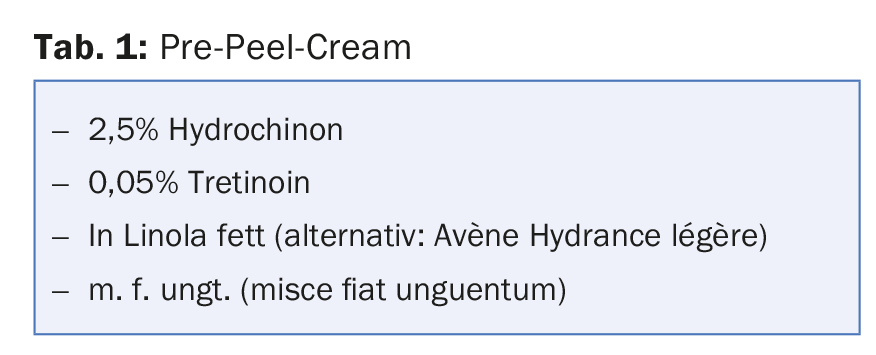
Pretreatment: The preoperative correct patient selection and the exact patient education are – besides a correct therapy – probably the most important cornerstones in the successful peeling treatment. The enormous reaction after a medium-deep or deep peel means considerable physical, but also psychological stress for the treated person. This is all the more serious if it occurs unexpectedly – however, it can be reduced to a maximum with intensive detailed information. Long-term planning of the procedure is extremely important, and patients should not experience any additional stressful moments during the first week after the procedure. It has proven useful to involve the patient’s partner in the discussion. Showing pictures of other patients directly and a few days post interventionem can help to explain the reactions after the peeling. If the patient knows in all details what to expect and can estimate from the explanation which reaction is normal and which one to report, he can well tolerate the relatively short period of the first reactions. To improve the final result, it has proven useful to subject patients with a planned medium-deep or deep peel to a prepeel four weeks before the procedure (Table 1). This bleaching and slightly irritating pre-treatment, which is applied regularly at night for four weeks, can increase the depth effect of the subsequent peeling.
Treatment: Regardless of whether a superficial, medium-depth or deep peel is performed, a standardized professional approach is essential during treatment. The correct handling with the different peeling solutions will be shown at various workshops. Before any peeling treatment, appropriate training of the specialist is a sine qua non. All patients receive herpes prophylaxis using valacyclovir 2× 500 mg/d until complete re-epithelialization – regardless of whether or not there is a positive history of herpes infections. Although even medium-depth and deep peels cause little pain after treatment (phenol peels require consistent and also effective pain prophylaxis during the first 24 hours after the procedure), patients should receive NSAIDs during the acute inflammatory phase to reduce inflammatory swelling.
Aftercare: In principle, appropriate aftercare is not necessary for superficial peels. Patients are told to apply a rich day and night cream in sufficient quantity for the days immediately following. During the inflammatory phase, sun protection is of great importance to avoid post-lesional hyperpigmentation. Elevation of the face after medium-deep or deep peeling, application of cooling compresses and constant application of cream with ointment-based externals weaken the tendency to edema and tightness of the treated skin during the first few days. It is recommended that patients be admitted every day in order to remove the scabs or crusts after moist compresses. carefully remove the peeling skin. Experience shows that the patients treated very much appreciate this care, especially since in the vast majority of cases there are uncertainties despite correct information in advance. Once the acute inflammatory-exudative phase is over and epithelialization forms, it is possible to switch from ointment bases to treatment with creams.
Complications and their prevention
We need to distinguish expected responses from unexpected complications. The deeper the peeling, the more pronounced the postoperative inflammatory-exudative phase. These reactions are therapy-specific and must be approached with an empathic professionalism. If sins of omission are committed here, further-reaching complications very quickly loom. First and foremost are prolonged wound healing, long persistent erythema with possible formation of telangiectasias and post-lesional hyperpigmentation. The risk of eczema herpeticatum in deepithelialized skin must be addressed with mandatory herpes prophylaxis. The most serious complication is likely to be scarring, as this is usually irreversible.
Such complications are largely avoidable if relatively simple rules are followed and patients are fully cared for in the pre- and especially in the post-operative period. If wound healing is threatened, externals containing antibiotics are used in alternation with halogenated corticosteroid ointments. Many of the above complications are secondary to protracted wound healing. Doctors who perform peeling treatments must be precisely trained and relatively experienced. This is achieved by educating oneself theoretically (literature and congress visits), but also practically (live workshops). The still inexperienced physician should approach peeling treatments and first perform superficial peels on patients who enjoy his trust. Follow-up examinations of your own patients bring a rapid learning curve, so that relatively soon medium-depth and later deep peels can also be performed.
Literature:
- Kreyden OP, et al; Swiss Group of Esthetic Dermatology and Skincare (SGEDS): The satisfied patient in aesthetic dermatology. Consensus paper on patient satisfaction in botulinum toxin A treatment. Dermatologist 2015 Feb; 66(2): 131-136.
DERMATOLOGIE PRAXIS 2015; 25(6): 40-43