Heartburn and acid regurgitation are symptoms that are a common cause for presentation to the primary care physician’s office. If there are no other complaints, however, an endoscopy can usually be dispensed with at first. Rather, probationary PPI treatment should be relied upon. Only if there is no improvement with this pharmacotherapy do further measures come into play.
Reflux disease manifests clinically as esophageal syndromes with heartburn and acid regurgitation and extraesophageal syndromes. If no endoscopic lesions can be detected, the disease is non-erosive reflux disease (NERD), which is found in 70% of cases. As Prof. Dr. med. Wolfgang Fischbach, Aschaffenburg (D), further explained, the remaining 30% can be assigned to erosive reflux disease (ERD). In them, strictures, Barrett’s esophagus, or carcinoma can be seen. Extraesophageal syndromes manifest predominantly laryngopharyngeally with dental erosions. The therapy goals are clear: patients primarily want to achieve freedom from symptoms. Physicians go a step further and additionally aim to cure lesions, achieve remission, and prevent complications and progression. In addition to general measures, drug interventions and surgical antireflux surgery are available for this purpose.
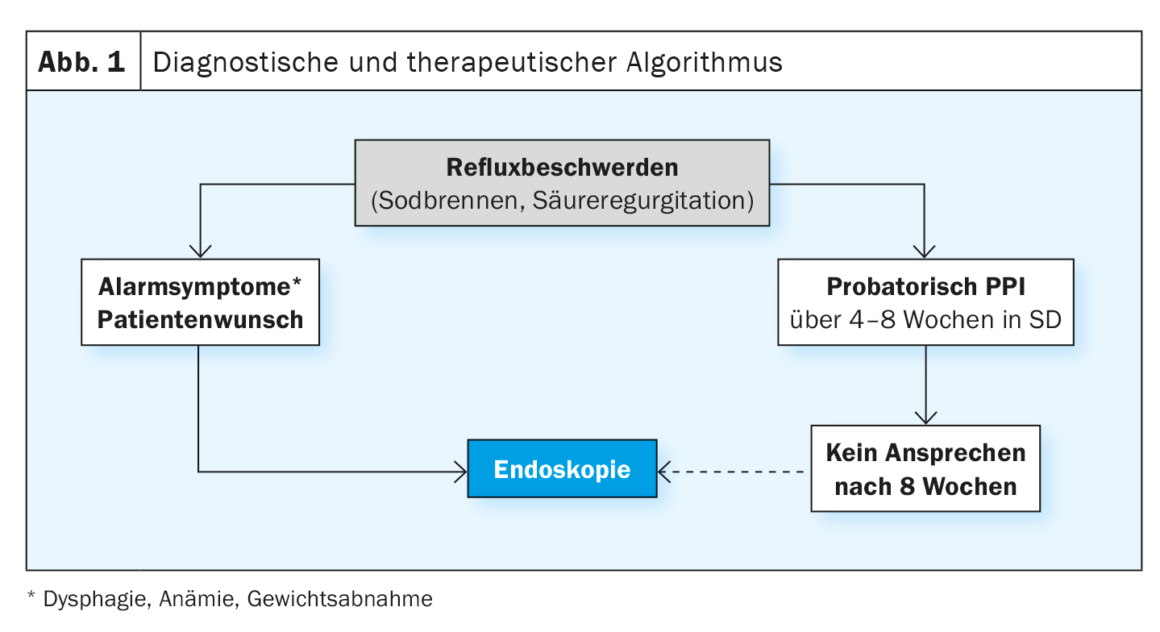
Diagnosis and therapy algorithm
Patients with reflux symptoms should first be treated with a proton pump inhibitor (PPI) on a trial basis for four to eight weeks. This is followed by an outlet attempt. However, PPIs should not be discontinued abruptly, but should be phased out at half the dose for one week and then only every other day for another week, the expert emphasized. If discomfort occurs, an antacid or alginate may also be administered. If the affected person does not respond to the PPI after eight weeks of treatment, an endoscopy should be performed. However, at the patient’s request or in the event of alarm symptoms such as dysphagia, anemia, and weight loss, this is used earlier – namely even before the probatory PPI administration (Fig. 1) .
PPIs are first-line agents in acute therapy and in maintenance therapy as permanent or on-demand medication. In most cases, they are very well tolerated. However, fatigue, dizziness, headache, sleep disturbances, skin changes or increased liver levels may rarely occur. If pharmacotherapy is not tolerated or if symptoms persist, a switch to another PPI as well as another drug treatment option and add-on therapy may be considered. Laparoscopic antireflux surgery is appropriate for patients who do not respond to adequate doses of PPIs, do not desire long-term medication, and have nonacid or high-volume reflux. However, sufferers should be aware that in more than 50% of cases, acid inhibition will be required again down the road, Fischbach said.
General measures that can support treatment management include weight reduction, avoidance of late meals, exclusion of individual food intolerances, upper body elevation, smoking cessation, and reduction of alcohol consumption.
Conclusion
The expert summarized that reflux complaints are very common. PPIs are very effective and safe in treatment. They can be used primarily on a trial basis and, if necessary, as a permanent medication. Endoscopy should be performed when there are alarm symptoms or during the course of the disease. If a patient does not respond to first-line treatment with PPIs, alternatives and adjunctive measures can be considered. In addition, if symptoms are not present, a discontinuation of pharmacotherapy should be considered.
Source: “Gastroenterology I: Esophagus, Stomach, Small Intestine, Pancreatitis”, Prof. Dr. med. Wolfgang Fischbach, Aschaffenburg, fresh up Hausarztmedizin, March/April 2023.
HAUSARZT PRAXIS 2023; 18(6): 37 (published 6/23, ahead of print)